Abstract
Background
The talus has a very complex anatomical morphology and is mainly fractured by a major force caused by a fall or a traffic accident. Therefore, a talus fracture is not common. However, many recent reports have shown that minor injuries, such as sprains and slips during sports activities, can induce a talar fracture especially in the lateral or posterior process. Still, fractures to the main parts of the talus (neck and body) after ankle sprains have not been reported as occult fractures.
Methods
Of the total 102 cases from January 2005 to December 2012, 7 patients had confirmed cases of missed/delayed diagnosis of a talus body or neck fracture and were included in the study population. If available, medical records, X-rays, computed tomography scans, and magnetic resonance imaging of the confirmed cases were retrospectively reviewed and analyzed.
Results
In the 7-patient population, there were 3 talar neck fractures and 4 talar body fractures (coronal shearing type). The mechanisms of injuries were all low energy trauma episodes. The causes of the injuries included twisting of the ankle during climbing (n = 2), jumping to the ground from a 1-m high wall (n = 2), and twisting of the ankle during daily activities (n = 3).
Ankle injuries are one of the most common reasons for hospital emergency room visits. Ankle sprains account for the highest number of ankle injuries. Ankle ligament injuries represent 14%–21% of total sport lesions. Most ankle injuries are straightforward ligamentous injuries. However, the clinical presentation of subtle fractures can resemble ankle sprains, and these fractures are frequently missed on initial examination. Nearly 18% of patients with ankle injuries present with an associated foot and/or ankle fracture.12)
A talus fracture is uncommon; it comprises 3%–5% of all foot and ankle fractures and only represents 0.1% to 0.85% of all fractures.34) Talus fractures are typically associated with a high-energy mechanism such as a motor vehicle accident (car, motorcycle) and falling down.5) However, some of them also arise from minor ankle injuries, such as an ankle sprain or slip while playing a sport. A literature review revealed that fractures of the lateral, medial, or posterior process of the talus are frequently overlooked and should be considered in the differential diagnosis of patients with acute and chronic ankle pain because an early diagnosis and treatment prevent long-term complications.3678) However, fractures to the main parts of the talus (neck and body) after ankle sprains have not been reported as occult fractures. We present several cases of talar fractures that were not initially recognized and misdiagnosed as ankle sprains.
Following Eulji Medical Center Institutional Review Board (EuljiIRB 14-100) approval, the medical record database maintained by Eulji Medical Center was queried for talus fractures that were either undiagnosed (missed diagnosis) or diagnosed at a later date (delayed diagnosis) between January 2005 and December 2012. The query returned 102 cases of talus fractures that required either surgical intervention or conservative treatment. Chart reviews were performed on each case by a fellow surgeon to establish if the cases could be classed as either a missed or delayed diagnosis of a talus fracture (defined as a case where a patient experienced a delay between the initial examination and treatment of the ankle sprain or a definitive diagnosis of a talus fracture) through dictated reports and imaging documentation. We excluded patients who had been misdiagnosed in spite of initial X-rays showing suspected signs of talus fracture, who had multiple injuries after a high-energy trauma, or who had lateral, medial, or posterior process fractures.
Of the 102 cases returned by the database query, 7 patients were confirmed as cases of a missed/delayed diagnosis of a talus fracture and thus included in the study population. If available, medical records, X-rays, computed tomography (CT) scans, and magnetic resonance imaging (MRI) of the confirmed cases were retrospectively reviewed and analyzed. In addition, multiple data points of the confirmed cases were collected, including the patient's gender, age at the time of the injury, the interval to the definite diagnosis of the fracture (number of days between the missed diagnosis at the initial examination and the definitive diagnosis), formal definitive diagnosis (fracture type and classification), mechanism of injury, physical examination findings of the definitive diagnosis, modality of the initial treatment, techniques (e.g., imaging) used to confirm the definitive diagnosis, and the presence and type of complications seen at the follow-up appointment.
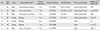
The study population diagnosed with a talus body or neck fracture that was missed at the initial examination included 4 males and 3 females. The average patient age at the time of injury was 42.8 years (range, 24 to 62 years) with an average delay in diagnosis of 4.6 months (range, 2 to 8 months). The mechanisms of injuries were all low energy trauma episodes. The causes of injuries included twisting during climbing (n = 2), jumping to the ground from a 1-m high wall (n = 2), and twisting of the ankle during daily activities (n = 3). In the 7-patient population, there were 3 talar neck fractures (Hawkins type I)9) and 4 talar body fractures (coronal shearing type)10) (Table 1).
There were two clinical consequences of diagnosing the injury as a talus fracture. Firstly, 6 patients were referred from a primary physician care center. They took plain foot and ankle films at the initial hospital visit for the injury, and the films were provided to the primary diagnosing physicians' offices. At that time, according to their statements, no fractures were identified on the standard films (Fig. 1). The patients were released from the primary care center after short-term bracing (2 to 3 weeks) and allowed to place some weight without protection on the ankle due to the diagnosis of the injury as an ankle sprain. When these patients first visited the author's office, they had either previously received an initial diagnosis of a "sprain" or they had booked an appointment with the author after a period of "persistent pain," following a visit to a primary care center. Prior to referral to the author's offices, only 1 patient had undergone MRI (Fig. 2). The rest of them had been diagnosed through a follow-up X-ray and advanced imaging modalities, including MRI (n = 3) and CT (n = 2) in the Eulji Medical Center (Figs. 3, 4, 5, 6). Secondly, a 24-year-old female patient had visited the emergency room of the Eulji Medical Center with an injury to her left foot after falling from a step. On initial examination, the ankle joint was significantly swollen and severely tender. Massive hematomas were present in both the medial and lateral parts of the ankle spreading to the foot. At that time, no fractures had been identified on standard anteroposterior or lateral X-ray images. The patient was released from the hospital with a short-leg, non-weight bearing cast, using 2 crutches due to the diagnosis of a severe ankle sprain. During a follow-up examination 1 week later, the patient still complained of a sharp continuous pain in the ankle. Due to these symptoms, the patient underwent a CT scan. At this point, an undisplaced talar neck fracture was diagnosed (Fig. 7).
One patient who showed a displaced fracture was operatively managed through open reduction internal fixation with screws. The other patients were conservatively managed with pain control or protection by orthosis (n = 6).
Some complications were reported from the patients with talar body fracture: 1 case of avascular necrosis (AVN) (Fig. 1), 1 case of posttraumatic arthritis of the subtalar joint, and 4 cases of posttraumatic arthritis of the tibiotalar joint (Figs. 1, 2, 3, 4). However, the remaining 3 patients who had talar neck fractures did not report any complications. The patient who showed AVN during the final follow-up imaging study complained of persistent pain during standing position or walking. He continued to wear a brace and perform limited daily activities. The other patients were finally diagnosed with arthritis in the ankle. They complained of ongoing pain when working outside. In particular, one of them had to quit his job and find a new one. The patient who was diagnosed with subtalar joint arthritis complained of intermittent discomfort when running or walking long distances.
Acute ankle injuries are the most common injuries in emergency rooms with an estimated incidence of 1 per 10,000 patients per day. Ankle sprains comprise 4.7% to 24.4% of all sports-related injuries.11) The lateral ankle ligaments are the structures that are most frequently damaged, specifically the anterior talofibular ligament and the calcaneofibular ligament.12) However, many structures, both bone and soft tissue, have the potential for injury during a foot and ankle inversion stress. The osseous structures that are at risk include the talar dome, talar lateral process, fifth metatarsal base, distal and proximal fibula, and the anterior process of the calcaneus. In addition to the lateral ankle ligaments, the soft tissue structures at risk include the distal tibia-fibula ligament, posterior talofibular ligament, subtalar interosseous ligaments, peroneal tendons, peroneal retinaculum, superficial peroneal nerve branches, and the medial ankle structures.
Fractures of the lateral process of the talus are frequently overlooked and should be considered in the differential diagnosis of patients with acute and chronic ankle pain.6) The lateral process fracture is rare, missed initially in about 50% of cases, and usually needs to be fixed internally. The diagnosis of a fracture of the posterior process is usually difficult, especially if the displacement is not significant. It is important to recognize these fractures because they result in severe limitations in ankle and subtalar motions.37) Our study is the first report of talar body or neck fractures after such minor injuries, suggesting the fractures of the talar neck or body should be considered as occult fractures after ankle sprains.
The mechanism of the talar neck fracture is similar to that of the talar body fracture. According to Higgins and Baumgaertner,13) a talar neck fracture occurs with forced dorsiflexion, and the anterior tibial lip is a wedge over which the talar neck is split. They stated that pure dorsally directed shear force at the talar head or just at the distal, with the ankle locked in neutral, reliably produced a vertical talar neck fracture on a fresh cadaver specimens.13) The mechanism of shear fractures of the talar body is not well documented and understood but is thought to be similar to that of talar neck fractures possibly with an added element of axial compression.1314) The injury mechanism in our study includes jumping on the ground, tripping down the stairs, and twisting the ankle when climbing. All the patients in our study would have had a dorsiflexion moment or dorsally directed shear force in their injury mechanisms.
A talar body or neck fracture would be more difficult to diagnose than a lateral process fracture or a posterior process fracture of the talus. In the series of lateral process fractures, this injury was attributed to a dorsiflexion/inversion mechanism.1516) On the other hand, some reports have described alternative mechanisms of the fracture of posterior process: such an injury can occur when the foot is in plain dorsiflexion, plantar flexion, or supination.171819) According to these reports, rotational force was included in the injury mechanism for a lateral or posterior process fracture. Therefore, these fractures could be displaced more. However, in the talar body or neck fracture, pure shear force or compressive axial force was applied. As such, displacement would be minimal in cases of such a low energy injury.
Fractures of the talus can be anatomically grouped into fractures of the neck, the dome, the talar processes, and the body.20) Undisplaced fractures of the talar neck or body are rare and represent an important diagnostic problem. Misdiagnosis is possible due to the inappropriate interpretation of conventional X-rays and a low level of awareness. As the most frequent diagnosis of ankle injuries is ankle sprain, many fractures of the ankle are often misdiagnosed as severe sprains.21)
Sneppen et al.10) introduced a classification of the body of the talus, which includes a compression fracture, coronal shearing fracture, sagittal shearing fracture, fracture in the posterior tubercle, fracture in the lateral tubercle, and crush fracture. In our 4 cases of talar body fractures, they were all coronal shearing fractures. Though the displacement was minimal without comminution, the prognosis of these patients was serious. Sneppen et al.10) demonstrated a poor prognosis for body fractures mainly because of malunion and subluxation. Such intra-articular fractures have a poor prognosis due to the high incidence of malunion and early degenerative symptomatic osteoarthritis.20) In our study, 4 cases of talar body fractures showed secondary arthritic changes in the tibiotalar joint and subtalar joint and 1 case of AVN. For type I fractures of the talar neck, good to excellent results were reported in 40% to 100% of patients.14) The wide variance in outcomes of type I fractures may be secondary to the placement of some minimally displaced (or underdiagnosed) fractures in the type I category. In the current study, 3 cases of undisplaced talar neck fractures showed no complications, such as union problems, arthritis, or AVN.
An inherent limitation of this study was related to the retrospective design. Data collection relied on the patients' memories of the diagnosis process and this created a potential recall bias. In addition, most of the patients were transferred from other hospitals, which meant lack of adequate data. Furthermore, the current study did not include a sufficient number of cases to confirm the conclusion of nondisplaced talar neck and body fractures. Despite these limitations, this study still adds value to the body of research on this subject because it is the first report on talar body or neck fractures after minor ankle injuries.
In conclusion, the significant risks of AVN, long-term posttraumatic arthritis, and subsequent suboptimal outcomes serve to increase the difficulty of managing talus fractures. A timely diagnosis is the most critical factor in a talus fracture. Surgeons need to be highly aware of the possibility of a talus fracture when evaluating a patient with acute and persistent chronic ankle pain. In addition, the patient's history of injury, duration of pain, and location of pain are essential to making an accurate diagnosis and a treatment decision that ensures a good clinical outcome. On occasion, treatment may include a series of X-rays at weekly intervals, a CT scan, and MRI to thoroughly evaluate the abnormality and diagnose the fracture. In conclusion, a talar body fracture includes a coronal shearing fracture and a talar neck fracture should be considered in the differential diagnosis of patients with acute and chronic ankle pain after minor ankle injuries.
Figures and Tables
 | Fig. 1(A) Frontal view of the ankle at initial presentation in the accident and emergency department. (B) Lateral view of the ankle at initial presentation in the accident and emergency department. (C, D) Frontal and lateral views of the ankle, showing a coronal shearing body fracture of the talus when the patient visited the clinic 5 months after the injury. (E) Sagittal magnetic resonance imaging demonstrating a coronal shearing body fracture of the talus accompanying avascular necrosis. |
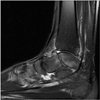 | Fig. 2Sagittal magnetic resonance imaging demonstrating a coronal shearing body fracture of the talus with a secondary arthritic change of the tibiotalar and subtalar joints. |
 | Fig. 3(A) Lateral view of the ankle, showing a coronal shearing talar body fracture with some displacement when the patient visited the clinic 3 months after the injury. (B) Sagittal magnetic resonance imaging demonstrating a coronal shearing body fracture of the talus with secondary arthritic change of the subtalar joint. |
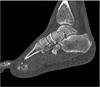 | Fig. 4Sagittal computed tomography demonstrating a coronal shearing body fracture of the talus with secondary arthritic change of the subtalar joint. |
 | Fig. 5Lateral view of the ankle, which shows a talar neck fracture with a malunion, when the patient visited the clinic 8 months after the injury. |
 | Fig. 6(A) Lateral view of the ankle, showing a minimally displaced talar neck fracture, 4 months after the injury. (B) Sagittal magnetic resonance imaging demonstrating a minimally displaced talar neck fracture. |
 | Fig. 7(A) Lateral view of the ankle at initial presentation in the accident and emergency department showing no abnormal findings. (B) Sagittal computed tomography demonstrating a minimally displaced talar neck fracture. |
Table 1
Clinical and Radiological Data of the Patients
References
1. Dowling SK, Wishart I. Use of the Ottawa Ankle Rules in children: a survey of physicians' practice patterns. CJEM. 2011; 13(5):333–338.

2. Morris N, Lovell ME. Demographics of 3929 ankle injuries, seasonal variation in diagnosis and more fractures are diagnosed in winter. Injury. 2013; 44(7):998–1001.

3. Rogosić S, Bojanic I, Boric I, Tudor A, Srdoc D, Sestan B. Unrecognized fracture of the posteromedial process of the talus: a case report and review of literature. Acta Clin Croat. 2010; 49(3):315–320.
4. Santavirta S, Seitsalo S, Kiviluoto O, Myllynen P. Fractures of the talus. J Trauma. 1984; 24(11):986–989.

5. Shakked RJ, Tejwani NC. Surgical treatment of talus fractures. Orthop Clin North Am. 2013; 44(4):521–528.

6. Mukherjee SK, Pringle RM, Baxter AD. Fracture of the lateral process of the talus: a report of thirteen cases. J Bone Joint Surg Br. 1974; 56(2):263–273.
7. Nyska M, Howard CB, Matan Y, et al. Fracture of the posterior body of the talus: the hidden fracture. Arch Orthop Trauma Surg. 1998; 117(1-2):114–117.

8. Sharma S. Fracture of lateral process of the talus presenting as ankle pain. Emerg Med J. 2003; 20(1):E2.

10. Sneppen O, Christensen SB, Krogsoe O, Lorentzen J. Fracture of the body of the talus. Acta Orthop Scand. 1977; 48(3):317–324.

11. Guillodo Y, Varache S, Saraux A. Value of ultrasonography for detecting ligament damage in athletes with chronic ankle instability compared to computed arthrotomography. Foot Ankle Spec. 2010; 3(6):331–334.

12. DIGiovanni BF, Fraga CJ, Cohen BE, Shereff MJ. Associated injuries found in chronic lateral ankle instability. Foot Ankle Int. 2000; 21(10):809–815.

13. Higgins TF, Baumgaertner MR. Diagnosis and treatment of fractures of the talus: a comprehensive review of the literature. Foot Ankle Int. 1999; 20(9):595–605.

15. Hawkins LG. Fracture of the lateral process of the talus. J Bone Joint Surg Am. 1965; 47(6):1170–1175.

16. Heckman JD, McLean MR. Fractures of the lateral process of the talus. Clin Orthop Relat Res. 1985; (199):108–113.

17. Chen CW, Hsu SY, Wei YS. Fracture of the medial tubercle of the posterior process of the talus. Formos J Musculoskelet Disord. 2011; 2(2):62–65.

18. Dougall TW, Ashcroft GP. Flexor hallucis longus tendon interposition in a fracture of the medial tubercle of the posterior process of the talus. Injury. 1997; 28(8):551–552.

19. Gutierres M, Cabral T, Miranda A, Almeida L. Fractures of the posteromedial process of the talus: a report of two cases. Int Orthop. 1998; 22(6):394–396.
20. Schenck RC Jr, Heckman JD. Fractures and dislocations of the forefoot: operative and nonoperative treatment. J Am Acad Orthop Surg. 1995; 3(2):70–78.

21. Judd DB, Kim DH. Foot fractures frequently misdiagnosed as ankle sprains. Am Fam Physician. 2002; 66(5):785–794.




 PDF
PDF ePub
ePub Citation
Citation Print
Print


 XML Download
XML Download