Abstract
Background
The aim of this study was to investigate the relationship between clinical symptoms and cross-sectional area (CSA) of the median nerve at the carpal tunnel inlet before and after open carpal tunnel release (CTR).
Methods
Thirty-two patients (53 hands) that underwent open CTR for idiopathic carpal tunnel syndrome were prospectively enrolled. Median nerve CSA at the carpal tunnel inlet was measured preoperatively and at 2 and 12 weeks after CTR by high resolution ultrasonography. The Boston carpal tunnel questionnaire (BCTQ) was also completed at these times.
Results
BCTQ symptom (BCTQ-S) score was significantly improved at 2 weeks postoperatively, but BCTQ function (BCTQ-F) score and CSA were significantly improved at 12 weeks postoperatively. Preoperative CSA was significantly correlated with preoperative BCTQ-S and BCTQ-F scores but was not significantly correlated with postoperative BCTQ scores or postoperative changes in BCTQ scores. Postoperative median nerve CSA was not significantly correlated with postoperative BCTQ-S or BCTQ-F scores, and postoperative changes in median nerve CSA were not significantly correlated with postoperative changes in BCTQ-S or BCTQ-F scores.
Conclusions
The study shows clinical symptoms resolve rapidly after open CTR, but median nerve swelling and clinical function take several months to recover. In addition, preoperative median nerve swelling might predict preoperative severities of clinical symptoms and functional disabilities. However, postoperative reductions in median nerve swelling were not found to reflect postoperative reductions in clinical symptoms or functional disabilities.
Because ultrasonography provides a simple, noninvasive means of visualizing peripheral nerve pathologies, high resolution ultrasonography is viewed as a valuable diagnostic tool for peripheral entrapment neuropathies, particularly carpal tunnel syndrome (CTS).1) In particular, it can exclude anatomical variants such as bifid median nerves and space-occupying lesions, such as ganglia and neural tumors.2) Median nerve cross-sectional area (CSA) at the carpal tunnel inlet is the most commonly used ultrasonographic diagnostic parameter.34) Its use is based on the premise that the median nerve is enlarged proximal to the site of compression in the carpal tunnel due to edema and fibrous tissue proliferation.5)
Several authors have demonstrated correlations between Boston carpal tunnel questionnaire (BCTQ) scores and median nerve CSA enlargement in CTS and suggested CSA can predict symptom severity,678) and others have also reported that CSA has significantly reduced after carpal tunnel release (CTR).591011121314) However, the relation between postoperative CSA and postoperative BCTQ scores was not well addressed. Furthermore, previous studies usually evaluated postoperative median nerve CSA at one time point, and thus, CSA changes after surgery have not been assessed.
The purpose of this study was to investigate whether (1) BCTQ scores and median nerve CSA change with respect to time after open CTR; (2) preoperative CSA has any prognostic value in terms of predicting postoperative BCTQ scores; and (3) there is any relationship between BCTQ scores and median nerve CSAs at different times after open CTR.
This prospective study was approved by Institutional Review Board of Ewha Womans University Mokdong Hospital and all participants provided written informed consent. Patients that underwent open CTR between March 2013 and March 2014 for idiopathic CTS were selected as candidates for this study. Idiopathic CTS was diagnosed based on pain, tingling, or numbness over the distribution territory of the median nerve and on the findings of an electrophysiological study.
One patient with rheumatoid arthritis, 1 patient with hypothyroidism, and 2 patients with hormone therapy for breast cancer were excluded. Two patients with a history of distal radius fracture and 1 patient with a history of CTR on the same extremity were also excluded.
No eligible patient declined enrollment and 32 consecutive patients (53 hands) were enrolled in the study. Four were male and others were female. Mean patient age was 52 years (standard deviation [SD], 6 years), and the mean symptom duration was 11 months (SD, 7 months)
These assessments were performed by one of the authors who had an experience of musculoskeletal sonography for more than 5 years. The affected wrist was assessed ultrasonographically before open CTR and at 2 and 12 weeks postoperatively. Ultrasound studies were performed using an ATL HDI 3500 unit (Phillips Ultrasound, Bothell, WA, USA) and a 7–12 MHz line array transducer. During examinations, patients were seated in a comfortable position with hands supported so as to maintain a position of slight wrist hyperextension with elbows in flexion and forearms in supination. The linear array probe was positioned perpendicular to the surface of the median nerve. Median nerve CSAs were measured at the proximal inlet of the carpal tunnel using the pisiform bone as a reference.8) At this site, CSAs were measured by tracing nerve circumferences (Fig. 1), while excluding the hyperechoic epineurial rim. Measurements were repeated and results were averaged. The intraclass correlation coefficient of these 2 measurements during same testing sessions was 0.91.
Patients also completed the BCTQ preoperatively and at 2 and 12 weeks postoperatively. The BCTQ18) consists of 2 scales that evaluate symptoms (BCTQ-S) and function (BCTQ-F). BCTQ-S consists of 11 questions that address the severity and frequency of pain, numbness, weakness, and loss of dexterity. Five possible responses are offered for each question and are scored from 1 (no symptom) to 5 (severe). Results are expressed as the average scores of the 11 responses. BCTQ-F is composed of 8 questions that address difficulties in performing daily tasks. Responses are also scored using a 5-point scale (1 to 5, where 5 indicates greatest difficulty), and again results are averaged.
The Student t-test was used to compare mean median nerve CSAs and BCTQ scores at the 3 time points (preoperatively and at 2 and 12 weeks postoperatively). Pearson's correlation analysis was used to investigate the relationship between BCTQ scores and median nerve CSAs and the relationship between changes in BCTQ scores and median nerve CSAs at the 3 time points. Results are presented as mean ± SD, and statistical significance was accepted for two-tailed p-values of < 0.05.
BCTQ-S scores were significantly improved at 2 weeks postoperatively, but no further significant improvement was observed at 12 weeks postoperatively. At 2 weeks postoperatively, BCTQ-F scores were not significantly different from the preoperative values, but significant improvement was noted at 12 weeks postoperatively. Preoperative and second postoperative week medium nerve CSAs were not significantly different, but a significant CSA reduction was observed at 12 weeks postoperatively (Table 1).
Preoperative CSAs were significantly correlated with preoperative BCTQ-S (r = 0.38, p < 0.001) and BCTQ-F scores (r = 0.34, p < 0.001). However, preoperative CSAs were not significantly correlated with BCTQ-S or BCTQ-F scores at 2 weeks postoperatively (r = 0.01, p = 0.89 and r = –0.05, p = 0.48, respectively) or BCTQ-S or BCTQ-F scores at 12 weeks postoperatively (r = 0.04, p = 0.51 and r = –0.03, p = 0.69, respectively) (Table 2). In addition, preoperative CSAs were not significantly correlated with BCTQ-S or BCTQ-F score changes from the preoperative assessment to the second postoperative week (r = 0.08, p = 0.31, and r = –0.02, p = 0.78, respectively) or BCTQ-S or BCTQ-F score changes from the preoperative assessment to the 12th postoperative week (r = –0.04, p = 0.53, and r = 0.06, p = 0.45, respectively) (Table 3).
At 2 weeks postoperatively, median nerve CSAs were not significantly correlated with BCTQ-S (r = 0.08, p = 0.34) and BCTQ-F scores (r = –0.10, p = 0.25). Postoperative 12 weeks CSAs were not also significantly correlated with BCTQ-S (r = –0.03, p = 0.66) and BCTQ-F (r = 0.04, p = 0.56) (Table 2). Changes in CSAs from the preoperative assessment to the second postoperative week were not significantly correlated with BCTQ-S or BCTQ-F score changes over the same period (r = –0.12, p = 0.12 and r = 0.07, p = 0.40, respectively), and similarly CSA changes from the preoperative assessment to the 12th postoperative week were not significantly correlated with BCTQ-S score changes (r = –0.10, p = 0.27 and r = 0.04, p = 0.59, respectively) (Table 3).
Several studies591011121314) have been reported on postoperative CSA changes in the median nerve after CTR, and most showed CSAs significantly decreased from 12 weeks after surgery, which concurs with our findings. However, early postoperative median nerve CSA changes have not been previously reported. In the present study, measurable reduction in median nerve swelling was observed at 12 weeks but not at 2 week postoperatively, whereas clinical symptoms recovered rapidly, which implies that median nerve swelling does not necessarily reflect the severity of clinical symptoms during early postoperative period.
The correlation between preoperative BCTQ scores and preoperative median nerve CSAs has been previously reported.678) However, few have examined the relationship between postoperative BCTQ scores and postoperative CSAs. Furthermore, contradictory results have been reported for the associations between postoperative clinical outcomes and postoperative CSA. Smidt and Visser14) measured CTR outcomes using a 6-point ordinal transition scale. In their series, the mean median nerve CSA decreased from 14 mm2 to 11 mm2 in patients with good outcomes but remained almost the same (13 mm2 to 12.5 mm2) in those with poor outcomes. Vogelin et al.5) measured postoperative clinical outcomes using a 4-point Likert type scale and concluded that a postoperative CSA of ≤ 10 mm2 tended to be associated with better clinical outcomes than a postoperative CSA of > 10 mm2. On the other hand, Naranjo et al.13) measured the main outcome variables of CTR using a 5-point Likert scale and concluded ultrasonography was of limited value for assessing patients with poor outcomes after CTR because patients with cure or great improvement and those with slight or no improvement exhibited similar CSA reductions at 3 months after surgery. In the present study, postoperative CSA was not found to be correlated with postoperative BCTQ scores, which implies that postoperative CSA does not reflect postoperative clinical outcomes.
Studies also differ as to whether preoperative CSA has any value in terms of predicting postoperative clinical outcomes. Mondelli et al.12) measured patient satisfaction with CTR using a 5-point Likert scale and reported preoperative CSA predicted patient satisfaction. On the other hand, Smidt and Visser14) measured outcomes of CTR using a 6-point scale and concluded preoperative CSA was not correlated with postoperative outcomes. In the present study, no correlation was found between preoperative CSAs and postoperative BCTQ scores or preoperative to postoperative changes in BCTQ-scores.
Several limitations of the present study require consideration. First, ultrasonographic examinations were performed by one orthopedic surgeon aware of clinical histories. Second, no electrophysiological assessments were performed for comparative purposes.
In conclusion, this study shows that clinical symptoms recover rapidly after CTR but that it takes several months for median nerve swelling to subside and clinical function to be restored. In addition, this study suggests that median nerve swelling might predict preoperative symptom severity and functional disabilities but that it does not predict postoperative clinical outcomes. Furthermore, a postoperative reduction in median nerve swelling was not found to be associated with postoperative reduction in clinical symptoms or functional disabilities.
Figures and Tables
Fig. 1
(A) Transverse image of the median nerve at the proximal inlet of the carpal tunnel. (B) The cross-sectional area (dotted line) was measured by tracing nerve circumferences, while excluding the hyperechoic epineurial rim. *Pisiform bone as a reference.

Table 1
Outcomes at Each Observation Time
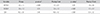
Values are presented as the mean ± standard deviation.
Preop: preoperative, Postop: postoperative, BCTQ: Boston carpal tunnel questionnaire, BCTQ-S: BCTQ symptom, BCTQ-F: BCTQ function, CSA: cross-sectional area of the median nerve at the proximal inlet of the carpal tunnel.
*Preop vs. Postop 2 wk. †Postop 2 wk vs. Postop 12 wk.
Table 2
The Correlation between CSA and BCTQ
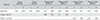
Table 3
The Correlation between Change of CSA and Change of BCTQ

References
1. Hobson-Webb LD, Massey JM, Juel VC, Sanders DB. The ultrasonographic wrist-to-forearm median nerve area ratio in carpal tunnel syndrome. Clin Neurophysiol. 2008; 119(6):1353–1357.

2. Wiesler ER, Chloros GD, Cartwright MS, Smith BP, Rushing J, Walker FO. The use of diagnostic ultrasound in carpal tunnel syndrome. J Hand Surg Am. 2006; 31(5):726–732.

3. Buchberger W, Schon G, Strasser K, Jungwirth W. High-resolution ultrasonography of the carpal tunnel. J Ultrasound Med. 1991; 10(10):531–537.

4. Yesildag A, Kutluhan S, Sengul N, et al. The role of ultrasonographic measurements of the median nerve in the diagnosis of carpal tunnel syndrome. Clin Radiol. 2004; 59(10):910–915.

5. Vogelin E, Nuesch E, Juni P, Reichenbach S, Eser P, Ziswiler HR. Sonographic follow-up of patients with carpal tunnel syndrome undergoing surgical or nonsurgical treatment: prospective cohort study. J Hand Surg Am. 2010; 35(9):1401–1409.

6. Kaymak B, Ozcakar L, Cetin A, Candan Cetin M, Akinci A, Hascelik Z. A comparison of the benefits of sonography and electrophysiologic measurements as predictors of symptom severity and functional status in patients with carpal tunnel syndrome. Arch Phys Med Rehabil. 2008; 89(4):743–748.

7. Karadag YS, Karadag O, Cicekli E, et al. Severity of Carpal tunnel syndrome assessed with high frequency ultrasonography. Rheumatol Int. 2010; 30(6):761–765.

8. Tajika T, Kobayashi T, Yamamoto A, Kaneko T, Takagishi K. Diagnostic utility of sonography and correlation between sonographic and clinical findings in patients with carpal tunnel syndrome. J Ultrasound Med. 2013; 32(11):1987–1993.

9. Abicalaf CA, de Barros N, Sernik RA, et al. Ultrasound evaluation of patients with carpal tunnel syndrome before and after endoscopic release of the transverse carpal ligament. Clin Radiol. 2007; 62(9):891–894.

10. Colak A, Kutlay M, Pekkafali Z, et al. Use of sonography in carpal tunnel syndrome surgery: a prospective study. Neurol Med Chir (Tokyo). 2007; 47(3):109–115.
11. Lee CH, Kim TK, Yoon ES, Dhong ES. Postoperative morphologic analysis of carpal tunnel syndrome using high-resolution ultrasonography. Ann Plast Surg. 2005; 54(2):143–146.

12. Mondelli M, Filippou G, Aretini A, Frediani B, Reale F. Ultrasonography before and after surgery in carpal tunnel syndrome and relationship with clinical and electrophysiological findings: a new outcome predictor? Scand J Rheumatol. 2008; 37(3):219–224.

13. Naranjo A, Ojeda S, Rua-Figueroa I, Garcia-Duque O, Fernandez-Palacios J, Carmona L. Limited value of ultrasound assessment in patients with poor outcome after carpal tunnel release surgery. Scand J Rheumatol. 2010; 39(5):409–412.

14. Smidt MH, Visser LH. Carpal tunnel syndrome: clinical and sonographic follow-up after surgery. Muscle Nerve. 2008; 38(2):987–991.

15. Cellocco P, Rossi C, Bizzarri F, Patrizio L, Costanzo G. Mini-open blind procedure versus limited open technique for carpal tunnel release: a 30-month follow-up study. J Hand Surg Am. 2005; 30(3):493–499.

16. Bromley GS. Minimal-incision open carpal tunnel decompression. J Hand Surg Am. 1994; 19(1):119–120.





 PDF
PDF ePub
ePub Citation
Citation Print
Print


 XML Download
XML Download