Abstract
Background
We analyzed the data for primary total hip arthroplasty (THA) in the Korean nationwide database to assess (1) the epidemiology and national trends of bearing surface usage in THAs and (2) the prevalence of each type of bearing surface according to age, gender, hospital type, primary payer, and hospital procedure volume.
Methods
A total of 30,881 THAs were analyzed using the Korean Health Insurance Review and Assessment Service database for 2007 through 2011. Bearing surfaces were sub-grouped according to device code for national health insurance claims and consisted of ceramic-on-ceramic (CoC), metal-on-polyethylene (MoP), ceramic-on-polyethylene (CoP), and metal-on-metal (MoM). The prevalence of each type of bearing surface was calculated and stratified by age, gender, hospital type, primary payer, and procedure volume of each hospital.
Results
CoC was the most frequently used bearing surface (76.7%), followed by MoP (11.9%), CoP (7.3%), and MoM (4.1%). The proportion of THAs using a CoC bearing surface increased steadily from 71.6% in 2007 to 81.4% in 2011, whereas the proportions using CoP, MoP, and MoM bearing surfaces decreased. The order of prevalence was identical to that in the general population regardless of age, gender, hospital type, primary payer, and hospital procedure volume.
Conclusions
The trends and epidemiology of bearing surface usage in THAs in Korea are different from those in other countries, and the CoC bearing surface is the most prevalent articulation. In future, the results of a large-scale study using nationwide data of THAs involving a CoC bearing surface will be reported in Korea.
Total hip arthroplasty (THA) is a treatment option for patients with advanced degenerative joint disease. Despite advances in THA, revision surgeries are necessitated by the long-term failure of implants using the conventional bearing material and polyethylene wear debris-induced periprosthetic osteolysis is the main cause of implant failure.1)
To overcome this problem, several alternative bearing surfaces, including metal-on-metal (MoM) and ceramic-on-ceramic (CoC), were recently adopted for primary THA in young, active patients and yielded favorable midterm results.23) Nevertheless, substantial shortcomings of these alternative bearings have been reported, including metal ion-related problems with MoM THA or ceramic failure with CoC THA.24) Reported rates of adverse soft tissue reactions to metal debris for MoM bearings range from 0% to 39%,56) and the United States Food and Drug Administration (FDA) released a safety announcement in February 2011 addressing these issues. Although the rate of complications associated with CoC bearings is low, unpredictable risks of audible squeaking emanating from the bearing as well as ceramic fractures can be indications for revision.78) These problematic complications have led to a decline in the use of hard-on-hard alternative bearing surfaces in Western countries.910) There are three epidemiological studies of bearing surface usage in primary THAs in the United States.91011) To our knowledge, however, there are no published studies of the epidemiology of bearing surfaces in Asian countries, nor have there been any studies tracking nationwide longitudinal bearing surface utilization in the general population.
The disease pattern and age distribution of patients that undergo THA in East Asia are different from those in Western countries.121314) Therefore, we postulated that the trends for bearing surface usage might also differ among countries. Moreover, taking into consideration the disclosed problems of alternative bearing surfaces, these issues in patients undergoing THA may be predicted by analyzing current national trends of bearing surface usage in primary THAs.
In this study, we analyzed the data for primary THAs in the Korean nationwide database to assess (1) the epidemiology and national trends of bearing surface usage in primary THA in Korea and (2) the prevalence of each type of bearing surface according to age, gender, hospital type, primary payer, and hospital procedure volume.
A total of 40,760 primary THAs, in which the bearing surface type used was identified, were analyzed using the Korean Health Insurance Review and Assessment Service (HIRA) database for 2007 through 2011. The database includes medical claims for all Korean citizens. In Korea, 97.0% of the population is legally obliged to enroll in the Korean National Health Insurance Program. Patients pay on average 30% of the total medical costs to clinics or hospitals. All clinics and hospitals then submit claims data for inpatient and outpatient care, including diagnoses (coded according to the International Classification of Disease, 10th Revision, Clinical Modification [ICD-10-CM]), procedures, prescription records, demographic information, and direct medical costs, to the HIRA to obtain reimbursement for 70% of the medical costs from the government. The remaining 3% of the population not insured by a Korean National Health Insurance Program is covered by the Medical Aid program. Claims data covered by the Medical Aid program are also reviewed by the HIRA, and thus, almost all information about patients and their medical records is available from the HIRA database.
Surgical procedures and medical devices in Korea were translated using the electronic data interchange (EDI) codes from the Korean National Health Insurance Program. Primary THA was identified by its principal procedure code (N0711) in the HIRA database. We thoroughly reviewed all medical devices that were claimed via the EDI code for patients that underwent primary THA. All detailed information about medical devices can be identified using the EDI code, such as product name, manufacturing company, materials used for the implant bearings, and cost. Femoral heads were classified into ceramic head and metal head, and acetabular liners were classified into ceramic liner, polyethylene liner, and metal liner. Bearing surface types were then determined if the femoral head and acetabular liner were used in one patient, and were sub-grouped into CoC, ceramic-on-polyethylene (CoP), metal-on-polyethylene (MoP), and MoM. Patients that underwent primary THA and contralateral revision THA or bipolar hemiarthroplasty, and those that underwent bilateral primary THAs during a single hospital admission were excluded because the combination of femoral head and acetabular liner could not be determined. Hip resurfacing and other combinations of femoral head and acetabular liner were also excluded from the study. A total of 30,881 (75.8%) primary THAs were finally included in the analysis. The proportion of procedures that were excluded remained unchanged throughout the study period (range, 23.1% to 25.2%).
The prevalence of each type of bearing surface was calculated and stratified by age, gender, hospital type, hospital volume, and primary payer. Hospital type in Korea is classified into four levels: clinics, hospital, general hospital, and tertiary hospital. Clinics focus mainly on outpatient care but are legally allowed to have up to 29 inpatient beds. Hospitals have a minimum of 30 inpatient beds and general hospitals are institutions that have a minimum of 100 inpatient beds and provide physician specialist services in major areas. Tertiary hospitals indicate general hospitals that are approved to provide most types of advanced medical care, treat severely ill patients and have a minimum of 20 departments. Hospital volume was divided into three categories according to the number of procedures performed annually: < 50 (low volume), 50 to 99 (medium volume), and ≥ 100 (high volume).
The significance of changes over the 5 years evaluated was assessed using the Cochran-Armitage trend test and the significance of differences in the proportion of bearing surfaces used was assessed using the chi-squared test.
This study protocol was exempted from review by the Institutional Review Board of the Seoul National University Hospital in accordance with the exemption criteria, and approved by the Institutional Review Board of National Evidence-based Healthcare Collaborating Agency (NECA).
A total of 30,881 primary THAs were performed using CoC, CoP, MoP, and MoM bearing surfaces between 2007 and 2011. The number of primary THAs increased by 25.2% from 5,484 in 2007 to 6,866 in 2011. The average age of the entire study population was 58.1 years, and 53.5% were male. Over 60% of all THAs were performed in hospitals with a minimum of 100 inpatient beds or in medium- to high-volume hospitals. National Health Insurance and Medical Aid respectively covered 87.6% and 12.4% of all THAs over the 5 years studied (Table 1).
CoC was the most commonly used bearing surface (76.7%), followed by MoP (11.9%), CoP (7.3%), and MoM (4.1%). The distribution of bearing surfaces was identical to that in the general population regardless of age, gender, hospital type, and primary payer (Table 2). The mean age of patients that received hard-on-hard bearing surfaces (CoC and MoM) was significantly younger than that of patients receiving hard-on-soft bearing surfaces (CoP and MoP) (56.9 years vs. 62.6 years; p < 0.05). During the study period, 55.1% of THAs that used a hard-on-hard bearing surface were performed in males, while 53.0% of THAs that used a hard-on-soft bearing surface were performed in females (p < 0.05). The order of prevalence of bearing surfaces was identical in low- and medium-volume hospitals (CoC was first, MoP was second, CoP was third, and MoM was fourth). In high-volume hospitals, CoC was also the most frequently used bearing surface, while the second most common bearing surface was CoP. According to hospital volume, the proportion of MoP bearing surface usage in high-volume hospitals was significantly lower (5.3%) than those in low- and medium-volume hospitals (18.3% and 14.9%, respectively; p < 0.001). More than half of MoP bearing surfaces was used in low-volume hospitals during the study period (55.3%). The mean hospital charges did not differ according to the bearing surface used, with the exception of CoP, which was associated with a lower mean hospital charge of $5,870 (p < 0.05) (Table 2).
There were no changes in the distribution of bearing surfaces in each year between 2007 and 2011 (CoC was first, MoP was second, CoP was third, and MoM was fourth) (Table 3). Overall, the percentage of THAs that used CoC bearing surfaces increased substantially from 71.6% in 2007 to 81.4% in 2011, while the percentage that used CoP, MoP, and MoM decreased significantly (p < 0.001) (Fig. 1). Despite its relatively low annual prevalence, the use of MoM decreased by half (from 5.8% in 2007 to 2.6% in 2011). Over the 5 years studied, there was minimal change in the mean age of patients receiving CoC, CoP, and MoP bearing surfaces; however, the mean age of patients that received MoM decreased from 57.3 years in 2007 to 52.2 years in 2011. The majority of THAs that used hard-on-hard bearing surfaces were performed in males, while hard-on-soft bearing surfaces were used more commonly in females. This gender difference remained during the study period and the proportion of female patients that received CoC, CoP, and MoP bearing surfaces did not change. However, the proportion of female patients that received MoM bearing surfaces increased significantly from 42.7% in 2007 to 49.4% in 2011 (p < 0.001) (Table 3 and Fig. 2). The mean hospital charges according to bearing surface remained consistent during the study period.
Overall, CoC bearing surfaces accounted for 76.7% of primary THAs and the order of prevalence of bearing surfaces in South Korea was not influenced by age, gender, hospital type, and primary payer (CoC was first, MoP was second, CoP was third, and MoM was fourth). To our knowledge, three epidemiological studies on bearing surface usage have been performed in the United States.91011) One of those studies detailed the national trends for bearing surface usage in patients aged 30 years and younger.9) Lehil and Bozic10) reported the trends for THA implant utilization in 174 hospitals representing 3% of all hospitals registered in the United States. We also identified the overall epidemiology of bearing surface usage and national trends in Australia using data from the Australian joint replacement registry.15)
The predominant usage of CoC bearing surface in primary THAs in Korea was not in agreement with previous reports. In the United States, the most commonly used bearing surface in primary THAs in the general population was MoP (51%), followed by MoM (35%) and CoC (14%) between 2005 and 2006,11) whereas MoM (37.6%) was first, CoC (24.6%) was second, MoP (22.1%) was third, and CoP (15.7%) was fourth in all THAs performed in patients 30 years of age or younger from 2006 to 2009.9) In Australia, information on bearing surfaces was identified using data from the Australian joint replacement registry since 2007; the MoP (57.1%) bearing surface was the most commonly used in primary osteoarthritis patients, followed by CoC (18.9%), CoP (12.8%), and MoM (11.2%), in 2007.15)
In comparison with the findings of Bozic et al.,11) who investigated the epidemiology of bearing surface usage among all age groups in the United States from 2005 to 2006, our study yielded different results. Bozic et al.11) reported substantial differences in bearing surface usage across age groups. Hard-on-hard bearing surfaces were used in 49% of the general population, 33.4% of patients ≥ 65 years, and 64.2% of patients < 65 years. In contrast, hard-on-hard bearing surfaces predominated irrespective of age group in Korea and were used in 80.8% of the general population, 72.8% of patients ≥ 65 years and 85.5% of patients < 65 years. In the United States, MoP was used in > 50% of primary THAs in large hospitals, while in small and medium hospitals, MoP was used in < 50% of THAs. Although there was no significant difference in bearing surface usage according to hospital size in Korea, there were substantial differences in bearing surface usage according to hospital volume. The proportion of MoP bearing surface usage in high-volume hospitals was significantly lower (5.3%) than in low- and medium-volume hospitals (18.3% and 14.9%, respectively; p < 0.001). Thus, the only difference was in the order of prevalence of bearing surfaces in high-volume hospitals (CoC was first, CoP was second, MoP was third, and MoM was fourth), compared to other population subgroups (CoC was first, MoP was second, CoP was third, and MoM was fourth). In a study by Bozic et al.,11) the majority of males (55.5%) received a hard-on-hard bearing, compared with only 42.9% of females. However, a hard-on-hard bearing surface predominated in both males (83.1%) and females (78.0%) in Korea. Similarly, the majority of THAs that used hard-on-hard bearing surfaces were performed in males, while the majority of THAs that used hard-on-soft bearing surfaces were performed in females in Korea. With the expectation of lower wear rate and greater implant longevity, hard-on-hard bearings have been used mostly in younger male patients as an alternative bearing in Western countries, and MoM bearings were used more commonly than CoC bearings.911) In Korea, CoC was the dominant bearing surface in all age groups and the proportion of MoM in hard-on-hard bearing surfaces was minimal during the study period. We could not identify the epidemiology of bearing surface according to age group using data from the Australian joint replacement registry, but CoC was the second most common bearing surface in primary THAs and MoM bearings were the least frequently used in the general population.15)
Why do hard-on-hard bearing surfaces, particularly CoC, predominate in Korea compared to other countries? In Korea, patients seldom affect a surgeon's decision in the choice of bearing surface. Implant costs for all bearing surfaces are almost identical and are controlled by government. In addition, hospital charges for all bearing surfaces are covered by the Korean National Health Insurance Program and Medical Aid program; therefore, reimbursement is not an issue in the selection of a bearing surface. Multiple factors may affect a surgeon's choice of bearing surface for primary THA. The reason for the dominant usage of hard-on-hard bearing surfaces may be that the principal diagnosis of primary THAs and the patient age group distribution in Korea differ from those in other countries. The most common indication for primary THA is osteonecrosis of the femoral head (58%) in Korea.14) In contrast, more than 75% of primary THAs are performed for osteoarthritis in Western countries.1617) Osteonecrosis of the femoral head affects mostly young male adults within their third to fifth decade of life. In our study, 53.5% of patients that received primary THA were male. The mean age in the general population was 58.1 years and the proportion of patients < 65 years was 62.9%. Therefore, a hard-on-hard bearing surface may be preferred by most Korean orthopedic surgeons for the majority of patients undergoing primary THA with an expectation of greater implant longevity. First-generation MoM prostheses had a higher rate of aseptic loosening than Charnley MoP implants, and despite incomplete understanding of the mechanisms of failure, these bearings were largely abandoned by the mid-1970s.618) Although second-generation MoM bearings have low rates of osteolysis comparable to those of CoC bearings, higher rates of adverse reactions to metal debris have been reported and there are no long-term data related to the safety issue.19) With medium- to long-term data for CoC bearings showing successful clinical outcomes and a markedly lower incidence of osteolysis, CoC has become the dominant hard-on-hard bearing for THAs in Korea.202122) In the United States, CoC bearings are often perceived as so-called premium bearings due to their higher cost and potential for greater implant longevity. According to the study by Bozic et al.,11) interestingly, hard-on-hard bearings were used more frequently in patients who were privately insured than in those insured by Medicare, and 22% of patients with private insurance had CoC bearings. Furthermore, patients > 65 years old with private insurance had hard-on-hard bearings more frequently than did Medicare patients. Since in Korea a surgeon's choice of bearing surface is not affected by implant cost or payer characteristics, a surgeon would probably tend to select the same bearing surface regardless of patient characteristics.
Since February 2011, the United States FDA has issued communications related to the safety of MoM devices due to concerns regarding adverse soft tissue reactions to metal debris. Since 2005, adverse soft tissue reactions to metal debris such as osteolysis, aseptic lymphocytic vasculitis-associated lesions, pseudotumor, and soft tissue destruction have been reported in THAs using MoM bearings.232425) Although it may not be nationally representative, a study by Lehil and Bozic10) showed that the usage of MoM bearings has decreased substantially in the United States. At its peak in 2007, 31% of primary THAs used MoM, dropping to 11% in 2010 and 1% in 2012. Nationwide data for the United States also showed that the proportion of THAs that used MoM bearing surfaces in patients ≤ 30 years decreased from 42.9% in 2006 to 29.4% in 2009.9) In Australia, the proportion of MoM bearings peaked at 12.3% in 2009, then dropped to 9.2% in 2012 and 2.3% in 2013.15) The percentage of MoM bearings in South Korea has decreased by more than half since 2007 (from 5.8% to 2.6%).
All epidemiological studies from the United States have shown a decrease in the use of CoC bearings over the past decade (from a peak of 11% in 2004 to 1% in 2012), and the authors assumed that the risk of squeaking and ceramic implant fracture may explain the decline in CoC usage.910111926) However, this trend may not be worldwide because the use of CoC bearings has increased in Australia (from 18.9% in 2007 to 26.2% in 2013) and Korea (from 71.6% in 2007 to 81.4% in 2011).
This study had several limitations. These include the reliance on the accuracy of the EDI code for identifying bearing surfaces and potential recording errors. However, since EDI codes are necessary for reimbursement purposes, they are a reliable source of information. Another limitation of the study was that not all primary THAs were included in the analysis, but our results could be representative of nationwide annual trends because the proportion of procedures excluded was unchanged over the time period examined.
In summary, the trends and epidemiology of bearing surface usage in primary THAs in Korea are different from those in other countries, and the CoC bearing surface is the most prevalent articulation in Korea. The choice of bearing surface may be affected by many factors, including the nation's medical delivery system, payment type, disease pattern, and age distribution of patients that undergo THA. In future, the results of a large-scale nationwide study on primary THAs using CoC bearing surfaces in Korea will be reported.
Figures and Tables
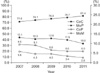 | Fig. 1Trends for bearing surface usage from 2007 to 2011. CoC: ceramic-on-ceramic, MoP: metal-on-polyethylene, CoP: ceramic-on-polyethylene, MoM: metal-on-metal. |
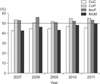 | Fig. 2The proportion of women in patients that received different bearing surfaces. CoC: ceramic-on-ceramic, CoP: ceramic-on-polyethylene, MoP: metal-on-polyethylene, MoM: metal-on-metal. |
Table 1
Demographic Characteristics of Patients

Table 2
Frequencies of Bearing Surface According to Gender, Age, Hospital Type, Hospital Volume, and Payer Type
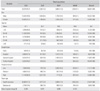
Table 3
National Trends of Bearing Surface Usage for Primary Total Hip Arthroplasty from 2007 to 2011

ACKNOWLEDGEMENTS
This study was funded by the National Evidence-based Healthcare Collaborating Agency (NECA; project No. NECA-B-12-003) and by a grant (#3020130080) from the Seoul National University Hospital Research Fund.
References
1. Beaule PE, Campbell P, Mirra J, Hooper JC, Schmalzried TP. Osteolysis in a cementless, second generation metal-on-metal hip replacement. Clin Orthop Relat Res. 2001; (386):159–165.
2. Hwang KT, Kim YH, Kim YS, Choi IY. Is second generation metal-on-metal primary total hip arthroplasty with a 28 mm head a worthy option? A 12- to 18-year follow-up study. J Arthroplasty. 2013; 28(10):1828–1833.

3. Yoo JJ, Kim YM, Yoon KS, Koo KH, Song WS, Kim HJ. Alumina-on-alumina total hip arthroplasty: a five-year minimum follow-up study. J Bone Joint Surg Am. 2005; 87(3):530–535.
4. Ha YC, Kim SY, Kim HJ, Yoo JJ, Koo KH. Ceramic liner fracture after cementless alumina-on-alumina total hip arthroplasty. Clin Orthop Relat Res. 2007; 458:106–110.

5. Haddad FS, Thakrar RR, Hart AJ, et al. Metal-on-metal bearings: the evidence so far. J Bone Joint Surg Br. 2011; 93(5):572–579.
6. Bosker BH, Ettema HB, Boomsma MF, Kollen BJ, Maas M, Verheyen CC. High incidence of pseudotumour formation after large-diameter metal-on-metal total hip replacement: a prospective cohort study. J Bone Joint Surg Br. 2012; 94(6):755–761.
7. Walter WL, Kurtz SM, Esposito C, et al. Retrieval analysis of squeaking alumina ceramic-on-ceramic bearings. J Bone Joint Surg Br. 2011; 93(12):1597–1601.

8. Allain J, Roudot-Thoraval F, Delecrin J, Anract P, Migaud H, Goutallier D. Revision total hip arthroplasty performed after fracture of a ceramic femoral head: a multicenter survivorship study. J Bone Joint Surg Am. 2003; 85(5):825–830.

9. Rajaee SS, Trofa D, Matzkin E, Smith E. National trends in primary total hip arthroplasty in extremely young patients: a focus on bearing surface usage. J Arthroplasty. 2012; 27(10):1870–1878.

10. Lehil MS, Bozic KJ. Trends in total hip arthroplasty implant utilization in the United States. J Arthroplasty. 2014; 29(10):1915–1918.

11. Bozic KJ, Kurtz S, Lau E, et al. The epidemiology of bearing surface usage in total hip arthroplasty in the United States. J Bone Joint Surg Am. 2009; 91(7):1614–1620.

12. Kobayashi S, Eftekhar NS, Terayama K, Iorio R, Takaoka K. Primary Charnley total hip arthroplasty: a comparison of American and Japanese cohorts followed for 10-20 years. J Arthroplasty. 2001; 16(3):340–350.
13. Hoaglund FT, Oishi CS, Gialamas GG. Extreme variations in racial rates of total hip arthroplasty for primary coxarthrosis: a population-based study in San Francisco. Ann Rheum Dis. 1995; 54(2):107–110.

14. Yoon PW, Lee YK, Ahn J, et al. Epidemiology of hip replacements in Korea from 2007 to 2011. J Korean Med Sci. 2014; 29(6):852–858.

15. Australian Orthopaedic Association National Joint Replacement Registry. Annual report 2014: hip and knee arthroplasty [Internet]. Adelaide: Australian Orthopaedic Association National Joint Replacement Registry;2014. cited 2015 Jun 2. Available from: https://aoanjrr.dmac.adelaide.edu.au/annual-reports-2014.
16. Malchau H, Herberts P, Eisler T, Garellick G, Soderman P. The Swedish total hip replacement register. J Bone Joint Surg Am. 2002; 84:Suppl 2. 2–20.

17. Zhan C, Kaczmarek R, Loyo-Berrios N, Sangl J, Bright RA. Incidence and short-term outcomes of primary and revision hip replacement in the United States. J Bone Joint Surg Am. 2007; 89(3):526–533.

18. Zahiri CA, Schmalzried TP, Ebramzadeh E, et al. Lessons learned from loosening of the McKee-Farrar metal-on-metal total hip replacement. J Arthroplasty. 1999; 14(3):326–332.

19. Rajpura A, Kendoff D, Board TN. The current state of bearing surfaces in total hip replacement. Bone Joint J. 2014; 96(2):147–156.

20. Kang BJ, Ha YC, Ham DW, Hwang SC, Lee YK, Koo KH. Third-generation alumina-on-alumina total hip arthroplasty: 14 to 16-year follow-up study. J Arthroplasty. 2015; 30(3):411–415.

21. Sugano N, Takao M, Sakai T, Nishii T, Miki H, Ohzono K. Eleven- to 14-year follow-up results of cementless total hip arthroplasty using a third-generation alumina ceramic-on-ceramic bearing. J Arthroplasty. 2012; 27(5):736–741.

22. Lee YK, Ha YC, Yoo JJ, Koo KH, Yoon KS, Kim HJ. Alumina-on-alumina total hip arthroplasty: a concise follow-up, at a minimum of ten years, of a previous report. J Bone Joint Surg Am. 2010; 92(8):1715–1719.
23. Willert HG, Buchhorn GH, Fayyazi A, et al. Metal-on-metal bearings and hypersensitivity in patients with artificial hip joints: a clinical and histomorphological study. J Bone Joint Surg Am. 2005; 87(1):28–36.

24. Witzleb WC, Hanisch U, Kolar N, Krummenauer F, Guenther KP. Neo-capsule tissue reactions in metal-on-metal hip arthroplasty. Acta Orthop. 2007; 78(2):211–220.





 PDF
PDF ePub
ePub Citation
Citation Print
Print


 XML Download
XML Download