Abstract
Background
To augment cement-bone fixation, Dr. Hironobu Oonishi attempted additional physicochemical bonding through interposition of osteoconductive crystal hydroxyapatite (HA) granules at the cement-bone interface in 1982. He first used the interface bioactive bone cement (IBBC) technique in 12 selected patients (12 hips) in 1982 (first stage) and followed them for 2 years. In 1985, the technique was applied in 25 total hip arthroplasty (THA) patients (second stage) and the effects were investigated by comparing the side with the IBBC technique and the other side without the IBBC technique. He has employed this technique in all THA patients since 1987 (third stage).
Methods
In the IBBC technique, HA granules (2 to 3 g) were smeared on the bone surface just before the acetabular and femoral components were cemented. In the first stage, 12 hips were operated using the IBBC technique in 1982. In the second stage, THA was performed without the IBBC technique on one side and with the IBBC technique on the other side within 1 year in 25 patients. In the third stage, THA was performed with the IBBC technique in 285 hips in 1987.
Results
In the first stage patients, implant loosening was not detected at 30 years after operation. In the second stage patients, revision was required in 7 hips without the IBBC technique due to cup loosening (5 hips) and stem loosening (2 hips), whereas no hip was revised after THA with the IBBC technique at 26 years after operation. In the third stage patients, the incidence of radiolucent lines and osteolysis was very few at 25 years after operation.
Cementing technique has been improved from the so-called first generation technique to the third generation technique, and the survival rates have increased accordingly.1) The focus of such improvements has been placed on securing mechanical interlocking between bone and bone cement. In 1982, Dr. Hironobu Oonishi attempted to obtain additional physicochemical bonding through interposition of osteoconductive crystal hydroxyapatite (HA) granules at the cement-bone interface to augment cement-bone fixation.2) This technique, the interface bioactive bone cement (IBBC) technique, provides bioactivity on the surface of bone cement as HA-coated cementless implants do.
He began to use this technique for 12 selected hips in 1982 (first stage) and followed up these patients for 2 years. In 1985, the technique was applied in 25 total hip arthroplasty (THA) patients (second stage), and the effects were investigated by comparing the side with the IBBC technique and the other side without the IBBC technique. He has employed this technique in all THAs since 1987 (third stage).3)
In this study, we reviewed the outcomes of these patients operated around the inception of the IBBC technique. Although the number of cases was not large, the follow-up periods were sufficiently long. In this study, we classified THA performed with the IBBC technique in 1982, 1985, and 1987 as the first stage, second stage, and third stage, respectively.
The operative technique and postoperative care were the same throughout the stages. All operations were performed under hypotensive general anesthesia (approximately 90 mmHg) by Dr. Oonishi. An anterolateral approach or a transtrochanteric approach was applied in the supine position. In all cases, a cobalt-chromium alloy femoral component (Bioceram Type 6; Kyocera Medical Co., Kyoto, Japan) with a 28-mm alumina ball and a polyethylene acetabular component (PHS socket; Kyocera Medical Co.) were used. The stem was triple-tapered with collar and the surface was grid-blasted. Synthetic porous HA was prepared by sintering at 1,200℃ in air and then crushed into granules (Sumitomo-Osaka Cement Co. Ltd., Chiba, Japan). The granules were sieved to sort by size. HA granules 300 to 500 µm in diameter were used. CMW-I bone cement (CMW Laboratories Ltd, Blackpool, UK) was used in all cases.
For the acetabular side, acetabular bone deficiencies were aggressively supplemented by structural autologous bone graft fixed with screws. Multiple small anchor holes were drilled after reaming. Hemostasis was achieved by temporal compresses at the bleeding points with bone paste obtained by acetabular reaming and rinsing with hydrogen peroxide followed by compressive gauze packing. The HA granules (2 to 3 g) were smeared on the bone surface by gauze just before the acetabular component was cemented. The porous HA granules reached into the cancellous structure and adhered easily to the wet bone surface.
For the femoral side, hemostasis was achieved by rinsing with hydrogen peroxide followed by compressive gauze packing. The HA granules (2 to 3 g) were smeared on the inner surface of the prepared femoral canal using a longitudinally split silicone tube (10 mm in diameter, 3 to 5 cm in length) grasped by a long straight Kocher clamp. This half-split silicone tube acted as an elastic spatula that enabled quick smearing of the HA granules from proximal to distal part of the femoral canal. The femoral component was fixed with second generation cementing techniques using an intramedullary bone plug and a cement gun. These procedures resulted in two to three layers of HA granules on most of the cement-bone interface, while bone cement directly contacted bone without interposition of HA granules in some parts where HA granules failed to be smeared.
In the first stage, 12 hips were operated using the IBBC technique in 1982. During follow-up, 3 patients (3 hips) died and 3 patients (3 hips) were lost to follow-up. Finally, 6 hips were able to be followed.
In the second stage, THA was performed without the IBBC technique on one side and with the IBBC technique on the other side within 1 year in 25 patients. The indication for surgery was degenerative coxarthrosis secondary to acetabular dysplasia in 24 hips and rheumatoid arthritis in 1 hip. Nine patients were lost to follow-up.
In the third stage, THA was performed with the IBBC technique in 285 hips in 1987. The indication for surgery was degenerative coxarthrosis secondary to acetabular dysplasia in 261 hips, rheumatoid arthritis in 14 hips, and osteonecrosis of the femoral head in 10 hips. The average age at the time of operation was 61 years (range, 24 to 88 years). Sixty-nine patients died of causes unrelated to THA and 41 patients were lost to follow-up. Institutional Review Board approval was obtained for these three series.
The presence of radiolucent lines, osteolysis, and loosening was evaluated on plain anteroposterior radiographs. Osteolysis was defined as a focal area of balloon-shaped lucency. Loosening was defined as more than 2-mm lucency around the implant at cement bone interface. The locations of radiolucent lines and osteolysis were identified according to the zones described by DeLee and Charnley4) for the acetabular components and the zones described by Gruen et al.5) for the femoral components.
After the first stage procedure, all 6 hips still functioned 30 years postoperatively. While polyethylene wear was observed, implant loosening was not detected (Figs. 1 and 2).
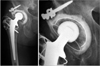
Sixteen patients were followed after the second stage procedure. In the hips without the IBBC technique, revision was required due to cup loosening in 5 hips and stem loosening in 2 hips. In the hips with the IBBC technique, no revision was necessary (Fig. 3). The incidence of radiolucent lines and osteolysis was greater in hips without the IBBC technique at 26 years after operation (Figs. 4 and 5). Osteolysis was observed in only 1 hip with the IBBC technique.
After the third stage procedure, 2 hips were revised due to late infection. No hip was revised due to implant loosening or dislocation. Ultimately, 173 hips could be followed. The incidence of radiolucent lines and osteolysis was very few at 25 years after operation (Fig. 6). The interface between bone and bone cement was intact even with the existence of polyethylene wear (Fig. 7).
In this article, we evaluated the outcomes of THA performed around the inception of the IBBC technique. When a new technology or technique is applied to patient treatment, the introduction should be done in a gradual and cautious manner. The IBBC technique does not require new materials; however, smearing the HA granules on the surface of cancellous bone has a risk of deteriorating the mechanical bonding between bone and bone cement by preventing interdigitation of bone cement into the cancellous bone.6) Thus, introduction of the IBBC technique for THA was advanced gradually in our patients from the first stage through the third stage before applying it to all patients.
With regard to the longevity of cemented THA, the bone-bone cement interface is one of the weak points. It has been reported that late aseptic loosening of cemented components is governed by the progressive resorption of the bone immediately adjacent to the cement mantle.7) This progressive bone resorption has been known to be fueled by polyethylene particles migrating along the bone-bone cement interface, and bone resorption occurs as a result of the macrophage inflammatory response to the polyethylene particles.
In an effort to augment the mechanical bonding between bone and bone cement, physicochemical bonding through addition of bioactive activity to bone cement was attempted. Most of the suggested methods were based on utilizing bioactivity inherent to bone cement. A bioactive bone cement consisting of an apatite- and wollastonite-containing glass ceramic powder, a silica glass powder as the filler, and a bisphenol-a-glycidyl methacrylate based resin as the organic matrix was tested in canine THA models.89) A strontium-containing HA bioactive bone cement was compared with polymethyl methacrylate (PMMA) bone cement in goat THAs.10) These bioactive bone cements have not yet been approved for clinical use. On the other hand, fluoride-containing acrylic bone cement was applied to patients;11) despite the expectation of the enhanced quality of the bone-bone cement interface, fluoride-containing bone cement did not improve stem fixation compared with the conventional cement. The approach suggested by Dr. Oonishi was to concentrate bioactivity at the bone-bone cement interface; by smearing the HA granules on the bone surface, the concentration of HA granules could become much higher than mixing HA granules with bone cement. Furthermore, compared to mixing of HA granules that affects the mechanical property of bone cement, the IBBC technique provides bioactivity at the bone-bone cement interface without deteriorating the mechanical property of bone cement, allowing for custom-made HA-coated cemented implants.
There are several limitations of this article that focuses on the results of THA performed around the inception of the IBBC technique. First, we did not have a control group throughout the stages. It is difficult to conclude the superiority of THA with IBBC technique over the conventional THA; however, the excellent long-term results can be considered to confirm the efficacy of the technique for the improved longevity of cemented THA. Second, the operative technique changed during the second stage; acetabular bone grafting was not aggressively done in cases of THA without the IBBC technique, whereas it was done for almost all cases after the introduction of IBBC technique. Since acetabular bone graft augments containment in dysplastic acetabulum, the use of graft could have contributed to improved results in the hips with THA using the IBBC technique. In general, acetabular bone grafting is a reasonable procedure for acetabular bone deficiency associated with hip dysplasia, thus we will continue to perform acetabular bone grafting for almost all cases.
Considering the aging of the population, osteoporosis might affect the longevity of THA. Histologic studies of retrieved specimens undertaken at 14 and 18 years after THA with the IBBC technique have shown that most of the HA granules were incorporated into the remodeled trabeculae.12) The HA used for cementless HA-coated implants contains amorphous HA in part,13) and thus is absorbed in the years following surgery.14) In contrast, the HA granules used in our technique are pure crystal and scarcely absorbed.1516) According to the histological findings of the 2 retrieved specimens taken from 61 and 60-year-old women, the osteoconductive activity seems to continue indefinitely even after the onset of osteoporosis.12)
The introduction of the IBBC technique for THA has been done gradually since 1982. The long-term follow-up of hips that underwent THA around the inception of IBBC technique revealed low incidences of radiolucent lines, osteolysis, and revision surgery. Based on the histological findings from the retrieved specimens, we can conclude that the bioactivity of crystal HA persists for a long term and the effects of the interposed HA granules obviate the occurrence of osteolysis and osteoporosis.
Figures and Tables
 | Fig. 3The left hip was operated without the interface bioactive bone cement (IBBC) technique 26 years ago. The right hip was operated with the IBBC technique 25 years ago. |
 | Fig. 4Incidence of radiolucent lines in hips with interface bioactive bone cement (IBBC) technique (A) and non-IBBC technique (B) in the second stage. |
 | Fig. 5Incidence of osteolysis in hips with interface bioactive bone cement (IBBC) technique (A) and non-IBBC technique (B) in the second stage. |
ACKNOWLEDGEMENTS
We would like to express the deepest appreciation to Dr. Hironobu Oonishi who created the idea of the IBBC technique and followed patients for a long time. We admire his great works and wish his soul to rest in peace.
References
1. Herberts P, Malchau H. How outcome studies have changed total hip arthroplasty practices in Sweden. Clin Orthop Relat Res. 1997; (344):44–60.

2. Oonishi H, Kadoya Y, Iwaki H, Kin N. Total hip arthroplasty with a modified cementing technique using hydroxyapatite granules. J Arthroplasty. 2001; 16(6):784–789.

3. Oonishi H, Ohashi H, Oonishi H Jr, Kim SC. THA with hydroxyapatite granules at cement-bone interface: 15- to 20-year results. Clin Orthop Relat Res. 2008; 466(2):373–379.
4. DeLee JG, Charnley J. Radiological demarcation of cemented sockets in total hip replacement. Clin Orthop Relat Res. 1976; (121):20–32.

5. Gruen TA, McNeice GM, Amstutz HC. "Modes of failure" of cemented stem-type femoral components: a radiographic analysis of loosening. Clin Orthop Relat Res. 1979; (141):17–27.
6. MacDonald W, Swarts E, Beaver R. Penetration and shear strength of cement-bone interfaces in vivo. Clin Orthop Relat Res. 1993; (286):283–288.

7. Schmalzried TP, Kwong LM, Jasty M, et al. The mechanism of loosening of cemented acetabular components in total hip arthroplasty: analysis of specimens retrieved at autopsy. Clin Orthop Relat Res. 1992; (274):60–78.
8. Fujita H, Ido K, Matsuda Y, et al. Evaluation of bioactive bone cement in canine total hip arthroplasty. J Biomed Mater Res. 2000; 49(2):273–288.
9. Liang B, Fujibayashi S, Fujita H, Ise K, Neo M, Nakamura T. Long-term follow-up study of bioactive bone cement in canine total hip arthroplasty. J Long Term Eff Med Implants. 2006; 16(4):291–299.
10. Ni GX, Lin JH, Chiu PK, Li ZY, Lu WW. Effect of strontiumcontaining hydroxyapatite bone cement on bone remodeling following hip replacement. J Mater Sci Mater Med. 2010; 21(1):377–384.
11. Digas G, Karrholm J, Thanner J. Addition of fluoride to acrylic bone cement does not improve fixation of a total hip arthroplasty stem. Clin Orthop Relat Res. 2006; 448:58–66.
12. Kim SC, Ohashi H, Oonishi H Jr, Oonishi H. Histologic findings at 14 and 18 years after cemented total hip arthroplasty with interface bioactive bone cement technique. J Arthroplasty. 2007; 22(7):1067–1069.
13. Zyman Z, Weng J, Liu X, Zhang X, Ma Z. Amorphous phase and morphological structure of hydroxyapatite plasma coatings. Biomaterials. 1993; 14(3):225–228.

14. Geesink RG. Osteoconductive coatings for total joint arthroplasty. Clin Orthop Relat Res. 2002; (395):53–65.





 PDF
PDF ePub
ePub Citation
Citation Print
Print





 XML Download
XML Download