Abstract
The trapezoid metacarpal dislocation is a rare event. In the literature, it is found in case reports. This injury is caused by direct or indirect high energy trauma. In most cases, the dislocation is dorsal and is difficult to reproduce because the joint is not very mobile. Given the low incidence and little evidence supported in the literature regarding the management, this injury can be treated by open or closed reduction; however, it has been published that most authors use Kirschner wire fixation with good results. Here we present our experience in the management of a male patient with acute trapezoid metacarpal dislocation handled with a splint with good functional results at 6 weeks.
The trapezoid-metacarpal joint dislocation is a rare event because of the stability of the joint,12345678) and there are only few case reports in the literature. This injury is caused by direct or indirect trauma that results in posterior dislocation in the majority of cases. Anterior deformity can also occur, but it is less common.1) The frequent cause is high energy trauma, particularly associated with car accidents, fall from heights, or rotational forces.2) This joint has limited mobility; consequently, some authors state that it is difficult to understand how dislocation can occur without a fracture.1257)
A 25-year-old male patient was admitted to the hospital. He suffered from trauma in the right hand in a motorcycle accident. He complained of swelling, functional limitation, and pain in the injured hand. Physical examination showed dorsal deformity of the metacarpal-trapezoid joint without distal neurovascular deficit. Radiographs showed metacarpal-trapezoid joint dislocation without fracture (Fig. 1). Closed reduction maneuvers were performed under regional block with lidocaine 1% without epinephrine of the dorsal wrist branches of the radial nerve, and improvement in the deformity was achieved. Radiographs showed good position and congruity after the closed reduction. Finally, the hand was protected with a Burkhalter splint for 6 weeks and a functional movement rehabilitation program was started.
The metacarpal-trapezoid joint is an arthrodial diarthrodial joint type5) and it has the characteristic that both bones offer a rigid anchorage.128) The integrity and stability of the joint depend on static and dynamic factors, allowing proper mobility of the arches of the hand.8)
The bone structure of the base of the second metacarpal (2MC) has a long ulnar condyle, which is in relation to the third metacarpal (3MC), and a smaller radial condyle in correspondence with the trapezium.15) There are fewer insertions into the radial side than the ulnar side, which makes the radial side weaker.15)
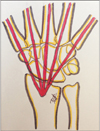
Nakamura et al.5) performed dissection of 80 wrists and found three dorsal ligaments. One in the ulnar region is between the trapezoid and 2MC or to the base of the 3MC. Another bundle is between the 2MC radial base to the trapezoid bone, and the last bundle originates from the 2MC radial base to the trapezium. The intermetacarpal ligament connects the 2MC and 3MC by the base of the ulnar to the radial region,5) the characteristic is the form of "V" connecting the anterior and the posterior part of the metacarpals with an apex towards the 3MC; the length of this ligament is shorter in comparison with that of the other metacarpal ligaments (Figs. 2 and 3).7)
The dorsal intercarpal ligaments are in relation with the capitate bone and the trapezoid, the distal trapezoid with the distal trapezium, and the proximal trapezoid with the proximal trapezium. Volar ligaments in the carpalmetacarpal space extend from the radial base of the 2MC to the trapezium.5) The intermetacarpal palmar ligament originates at the 2MC base and has a distal and dorsal disposition, and it inserts 1-mm distal to the carpal metacarpal joint surface.7)
The joint has an intimate relationship with the extensor carpi radialis longus and extensor carpi radialis brevis tendons; both these ligaments help generate stability.48) Mobility is low because of the configuration of the joint, which is usually 1° of flexion and extension. The flexion movement causes contraction of the dorsal ligaments, and the palmar ligaments are relaxed, the opposite occurs during extension.34789)
Because of the anatomical features of this joint, the occurrence of metacarpal-trapezoid dislocation seems impossible. At present, it is not known exactly how this injury occurs.5) The main mechanisms of this traumatic pathology are secondary to direct injury, fall from a height, or a rotational force (high-energy processes); which often result in posterior dislocation.1289)
Initially, the deforming force is from axial transmission, and it is directed towards the dorsal side because the metacarpal head is subjected to a flexion force that causes dislocation of the metacarpal base.3) When the mechanism of trauma is an indirect force, the result is opposite; a hyperextension force is generated that causes anterior dislocation. 3)
This injury was attempted to simulate in cadavers, but usually fractures were produced before isolated dislocation.7) To reproduce the injury, the anterior and posterior ligaments were cut and then a flexion force was applied on the carpometacarpal articulation in a dorsal direction; this was the only mechanism by which pure dislocation could be acquired.7) There are other speculative causes of the origin of this traumatic pathology associated with the effect of muscle contraction and joint disorders due to previous injury or congenital conditions.57)
After identifying the mechanism of trauma, the following clinical findings are observed in the patient: localized swelling and tenderness over the area of injury.8) Additionally, if there is a posterior dislocation, a dorsal prominence over the base of the 2MC (like a hump) (Fig. 4) with an accompanying rotational deformity of the second finger and a diminution of mobility of the index finger are observed.124) In the case of anterior dislocation, a dorsal depression on the carpometacarpal joint area of the index finger is noted.3) Because of the swelling, this injury can be missed, causing significant morbidity, pain, swelling, weakness of grip, and degenerative arthritis.6810)
Required radiographic projections are anteroposterior (AP) and lateral views, although some authors report that oblique images in 30° of supination should be obtained with the thumb abducted to observe the joint surfaces better. 48) A properly acquired lateral radiograph is sufficient to diagnose this type of injury; however, bone overlap makes the diagnosis difficult.6)
The intention behind performing the AP projection is to determine the loss of parallelism of the affected joint in comparison to the other joints; the two characteristics that should be observed are widening of the joint space of more than 2 mm and abnormal overlapping of the adjacent bones. The lateral view will help identify the volar or dorsal displacement of the metacarpals.38) The parallel M-line of the carpometacarpal joint forms a zig-zag pattern (Fig. 5).810)
If there is some doubt, the carpometacarpal angle can be measured on the lateral view. It is taken from the most volar portion of the 2MC head to the most anterior part of the 2MC base and the most volar part of the fifth metacarpal, the overlap of lines creates an angle that measures between 7° and 11° (Fig. 6).6) A subluxated joint is diagnosed when the angle measures between 13° and 15°, but this must be confirmed with physical examination.6)
The metacarpal cascade lines can be drawn on the AP projection, which is performed for every metacarpal, indicated by a centric vertical line that follows the bone shaft. The researchers should focus on a common point at 2 cm from the articular surface of the radius, and if the relationship of the lines is lost, then a dislocation is highly suspected, with a few false positives (Fig. 7).10)
Computed tomography (CT) has also been used, and it shows the joint and bony structures in greater detail. The disadvantage of CT is that it is expensive and requires more time compared to conventional radiography.10)
There is no classification for this type of pathology, or a time period that mention whether it is acute or chronic. However, Parkinson and Paton9) proposed that a dislocation more than 3 weeks old may be called chronic. This pathology is classified according to the anatomic location or open or closed reduction method. According to the anatomical part, there are two types of dislocation, anterior and posterior dislocation.1234) After considering the type of reduction needed, we can classify a dislocation as simple dislocation if closed reduction is adequate or as complex dislocation if open reduction is required; this is due to tissue interposition especially the extensor carpi radialis brevis tendon.2)
There are two types of treatment in the literature, but a comparison of the two different methods is not possible because of less number of reported cases. Some authors suggest that without an intervention few symptoms and functional alterations are produced, but others suggest limitation in the grip ability and loss of mobility due to the inveterate pathology.8)
The reduction maneuver is not difficult to perform, traction of the index finger is performed, a dorsal pressure force is applied on the deformity (2MC base), and then a Burkhalter splint is used for 6 weeks; radiographs should be made each week for 3 weeks due to the possibility of loss of reduction due to deforming forces produced by extensor carpi radialis longus, extensor carpi radialis brevis, and flexor carpi radialis tendon insertion. The splint is removed after 6 weeks of treatment, and then a physiotherapy program is started. If there is loss of reduction or no possible reduction, surgical management is performed.18)
Various types of surgical management have been described, for example, closed reduction and percutaneous pinning, open reduction and osteosynthesis with Kirschner wires (K-wires), and finally arthrodesis.8) Some authors prefer surgical management due to the possibility of instability.9)
When closed reduction is chosen, K-wires are used to maintain the articular surface, one is directed obliquely through the base of 2MC to the capitate bone, and the second pin is placed transversely from the base of 2MC to the base of 3MC and the joint is immobilized with a volar splint. K-wire fixation is used to maintain the reduction for a minimum of 7 weeks (6 to 8 weeks).238)
The goal of open reduction is to restore the anatomical part that has not been established by nonsurgical treatment or closed methods. Articular reduction is impossible with interposition of the extensor carpi radialis longus or brevis tendon, this produces a hole type injury on the posterior part of the capsule at the base of the 2MC interposing with the trapezoid.2) A dorsal approach is performed for the joint, the interposed tendon is liberated and articular reduction is performed with a periosteal elevator, and then K-wires are placed. Immobilization with a splint is performed for 6–8 weeks.8)
It is not possible to establish the best management for this entity because there are no studies with adequate number of patients to derive a strong conclusion; the majority of authors who performed fixation with wires reported good results but did not specify the scale.
Figures and Tables
 | Fig. 1Anterior (A) and lateral (B) views showing loss of integrity of the trapezoid and second metacarpal articulation. |
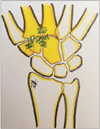 | Fig. 2Dorsal trapezoid and second metacarpal ligaments. (1) Ulnar base of the second metacarpal to trapezoid; (2) radial base of the second metacarpal to trapezoid; (3) trapezoid to ulnar base of the third metacarpal; and (4) dorsal intermetacarpal ligament. |
References
1. Lewis HH. Dislocation of the second metacarpal: report of a case. Clin Orthop Relat Res. 1973; (93):253–255.
2. Carneiro RS, Rancatore E. Dorsal dislocation of the index carpometacarpal joint. J Emerg Med. 2000; 18(1):21–22.

3. Pack DB, Grossman TW, Resnik CS, Gillespie T. Isolated volar dislocation of the index carpometacarpal joint: a unique injury. Orthopedics. 1995; 18(4):389–390.

4. Mehara AK, Bhan S. Rotatory dislocation of the second carpometacarpal joint: case report. J Trauma. 1993; 34(3):464–466.
5. Nakamura K, Patterson RM, Viegas SF. The ligament and skeletal anatomy of the second through fifth carpometacarpal joints and adjacent structures. J Hand Surg Am. 2001; 26(6):1016–1029.

6. Dzwierzynski WW, Matloub HS, Yan JG, Deng S, Sanger JR, Yousif NJ. Anatomy of the intermetacarpal ligaments of the carpometacarpal joints of the fingers. J Hand Surg Am. 1997; 22(5):931–934.

7. Shorbe HB. Carpometacarpal dislocations: report of a case. J Bone Joint Surg Am. 1938; 20(2):454–457.
8. Ahmad S, Plancher KD. Carpometacarpal dislocations of the fingers. Oper Tech Sports Med. 1996; 4(4):257–267.





 PDF
PDF ePub
ePub Citation
Citation Print
Print






 XML Download
XML Download