Abstract
Synovial osteochondromatosis (SO) can occur idiopathic or secondary to osteoarthritis. SO can be easily diagnosed with plain film radiography and clinical findings. In case of disabling osteoarthritis, total knee arthroplasty and removal of all corpora libra are indicated. We present a 71-year-old woman with significant osteoarthritis and severe SO intra-articular and in the suprapatellar bursa of the right knee. Total knee arthroplasty, extraction of the loose bodies, and partial synovectomy were performed. During a 2.5-year follow-up, the patient regained full function of her affected knee and there was no recurrence of SO. We choose to present this case to show the extensiveness SO can occur in. Our advice is to remove all the loose bodies carefully to prevent damage to the prosthesis. During follow-up, special attention should be paid to prevent recurrence of SO. When recurrence is associated with rapid growth or destruction of joints, malignant reoccurrence must be considered.
Synovial osteochondromatosis (SO) is a benign disorder characterized by proliferation and metaplasia in the synovial membrane. SO is less common than osteochondromatosis, is caused by a disturbance in endochondral ossification, and has an unfavourable course. According to Felbel et al.,1) the epidemiology of SO is 1 per 100,000. Treatment of SO with a low recurrence rate involves open or arthroscopic removal of loose bodies with (partial) synovectomy.2)
We present a case of secondary SO of the knee due to osteoarthritis. The purpose of presenting this case is to show the extensiveness of situations in which SO can occur secondary to degenerative osteoarthritis and to demonstrate the result of removal of loose bodies, partial synovectomy and total knee arthroplasty.
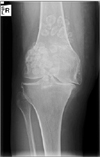
A 71-year-old woman presented with progressive complaints in the right knee. Complaints at presentation were: daily morning stiffness, starting pain, giving way, and pain at night, causing impairment in daily activities and decrease in the walking distance. Conservative therapy (medication and application of a valgus knee brace) was not sufficient. Physical examination showed a clinical varus leg axis, a stable medial collateral ligament, 15° of impaired extension, and 100° of flexion of the right knee. A significant swelling was noted on the dorsal side of the knee. X-ray showed significant osteoarthritis with marked medial joint space narrowing and substantial SO with multiple round calcifications in the intra-articular joint space and in the suprapatellar bursa (Figs. 1 and 2). As the diagnosis was obvious, we did not perform additional imaging. A biopsy was not considered necessary.
Since conservative therapy was not sufficient and X-ray showed significant osteoarthritis, a total knee arthroplasty and extraction of loose bodies were indicated. According to the Spaarne Gasthuis's self-developed "Fast-Track" protocol for total hip and knee arthroplasty, preoperatively, the patient received information about the procedure and revalidation, questionnaires were filled in (patient reported outcome measures), physical examination (as described above) was performed, and nose cultures were taken (if necessary, staphylococcus aureus infection was treated). The patient received 3 doses of perioperative prophylactic cefazolin and multimodal analgesics (meloxicam 15 mg, gabapentin 300 mg, paracetamol 1,000 mg, and local infiltration of analgesics 150 mL, ropivacaine 2 mg/mL). Surgery was performed in a laminar flow area. Perioperatively, the patient received tranexamic acid 1,000 mg. A tourniquet was not used. Via a midline incision, a medial arthrotomy was performed. First, the tibial component was prepared for arthroplasty by removing cruciate ligaments. Then, the femoral component was prepared for arthroplasty, an uncemented mobile bearing total knee arthroplasty, using the low contact stress (LCS) complete knee prosthesis produced by DePuy Synthes (West Chester, PA, USA). Surgery was performed by an experienced orthopaedic surgeon who specialized in knees. Perioperatively, numerous corpora libra were extracted carefully (Fig. 3) and the joint was irrigated. A drain was not used. No perioperative complications occurred, and the patient used the prosthesis under the guidance of a physical therapist 2 hours after surgery. Postoperatively, the patient received analgesics and was discharged after being admitted for 3 days, according to the Fast-Track protocol. The Fast-Track protocol requires a multidisciplinary team effort to be successful. There were no short-term complications. The postoperative X-ray showed no surgical complications (Figs. 4 and 5). During a 2.5-year follow-up, there were no complications and questionnaires were scored maximally. Flexion was 130° and extension was not impaired. Postoperative X-rays (Figs. 4 and 5) showed an unexcised synovial osteochondroma in the tendon sheath dorsal to the total knee prosthesis. During follow-up, this solitary synovial osteochondroma did not increase in size (Figs. 6 and 7). The patient gave permission for anonymous publication.
We chose to present this case since the extensiveness of SO in the intra-articular joint space and in the suprapatellar bursa as large as in this case, secondary to degenerative osteoarthritis, with arthroplasty and a 2.5-year follow-up with good results has not been described before (Table 1).345678)
SO is usually an incidental finding due to the frequently asymptomatic course. SO can occur intra-articularly or extra-articularly (e.g., bursa or tendon sheath). Symptoms include those produced by mass effect, swelling, locking, pain, and giving way. The pain experienced by our patient might be due to osteoarthritis. SO is typically mono-articular and it most commonly affects the knee, but the hip, ankle and elbow can also be affected.9) Physical findings include effusion, synovial thickening, crepitus, and palpable loose bodies.10) SO occurs twice as frequently in men than in women, and it most often presents in the third to the fifth decade of life and it also occurs in children. SO can be idiopathic, or more commonly, secondary to an irritated joint capsule as in degenerative osteoarthritis, osteonecrosis, osteochondritis dissecans, trauma, neuropathic osteoarthropathy, rheumatoid arthritis, and tuberculosis.11)
To diagnose SO, plain film radiography and clinical findings are essential.12) Plain film radiography shows multiple loose bodies varying from a few millimetres to 1 cm in diameter. SO can also present as a large solitary osteochondroma.13) Low- or intermediate-grade osteochondrosarcomas can be quite similar in presentation. When diagnosing SO, a pitfall is missing secondary osteochondrosarcomas, which were estimated to occur in 5% of the patients with SO in one series by Davis et al.14) It is important to keep osteochondrosarcomas in mind.
The purpose of treating SO is to prevent recurrence and to delay progression of secondary joint damage. Untreated SO may result in secondary arthritis due to mechanical injury caused by loose bodies and disturbance of the nutrition mechanism of the articular cartilage.15) In case of primary or secondary osteoarthritis, total knee arthroplasty and removal of all corpora libra are indicated. Ackerman et al.16) described four SO patients who received a total knee arthroplasty with good results, but, SO can recur. When recurrence is associated with rapid growth or destruction of joints, malignant recurrence must be considered.14) Ackerman et al.16) concluded that chondrocytes in primary SO are fairly active and capable of proliferation, whereas chondrocytes in secondary SO are uniform in appearance and inactive, and that this finding may obligate the surgeon to consider performing a complete synovectomy in the face of active synovium. We performed a partial synovectomy since SO was secondary to osteoarthritis.
We advise removal of all corpora libra carefully to prevent damage to the prosthesis and to routinely check patients with a total knee arthroplasty and a history of SO in the same joint every 2 years, to evaluate new or growing synovial osteochondromas. The corpora libra will only be seen on an X-ray if they are ossified enough, but they can cause complaints as described above.
Figures and Tables
Table 1
Case Reports of Synovial Osteochondromatosis

| Article | Case | Follow-up | Therapy | Result |
|---|---|---|---|---|
| Sourlas et al.3) | A 55-year-old man with 3 giant intra-articular SO | 2.5 yr | Evacuation of loose bodies by arthrotomy | Asymptomatic |
| Aydin et al.4) | A 64-year-old woman with an intra-articular solitary synovial osteochondroma | 2 yr | Evacuation by arthroscopy | No recurrence |
| Mackenzie et al.5) | A 49-year-old man with intra- and extra-articular SO, which extended from the bursa into the posterior distal thigh and proximal calf | 3 mo | Two-stage procedure with arthroscopy and open exploration in the popliteal fossa | Similar as contralateral |
| Bozkurt et al.6) | A 58-year-old woman with SO in 4 compartments of the knee, all intra-articular | 1 yr | Removal by arthrotomy and synovectomy | Pain-free |
| Shallop and Abraham7) | A 17-year-old boy with SO of the pes anserine bursa | Not mentioned | Surgical removal | Not mentioned |
| Singh et al.8) | A 32-year-old woman with SO in the suprapatellar, infrapatellar, and popliteal regions | Not mentioned | Radical synovectomy via anterior and posterior approaches | Similar as contralateral |
ACKNOWLEDGEMENTS
We would like to thank the patient and her family for giving permission to anonymously present this case.
References
1. Felbel J, Gresser U, Lohmoller G, Zollner N. Familial synovial chondromatosis combined with dwarfism. Hum Genet. 1992; 88(3):351–354.

2. Ogilvie-Harris DJ, Biggs DJ, Mackay M, Weisleder L. Posterior portals for arthroscopic surgery of the knee. Arthroscopy. 1994; 10(6):608–613.

3. Sourlas I, Brilakis E, Mavrogenis A, Stavropoulos N, Korres D. Giant intra-articular synovial osteochondromata of the knee. Hippokratia. 2013; 17(3):281–283.
4. Aydin N, Gokkus K, Topal C, Aydin AT. Solitary synovial osteochondroma of the knee: mimicking a giant loose body. Int Med Case Rep J. 2012; 5:83–86.
5. Mackenzie H, Gulati V, Tross S. A rare case of a swollen knee due to disseminated synovial chondromatosis: a case report. J Med Case Rep. 2010; 4:113.

6. Bozkurt M, Ugurlu M, Dogan M, Tosun N. Synovial chondromatosis of four compartments of the knee: medial and lateral tibiofemoral spaces, patellofemoral joint and proximal tibiofibular joint. Knee Surg Sports Traumatol Arthrosc. 2007; 15(6):753–755.

7. Shallop B, Abraham JA. Synovial chondromatosis of pes anserine bursa secondary to osteochondroma. Orthopedics. 2014; 37(8):e735–e738.

8. Singh S, Neelakandan K, Sood C, Krishnan J. Disseminated synovial chondromatosis of the knee treated by open radical synovectomy using combined anterior and posterior approaches. J Clin Orthop Trauma. 2014; 5(3):157–160.

9. Mertens F, Jonsson K, Willen H, et al. Chromosome rearrangements in synovial chondromatous lesions. Br J Cancer. 1996; 74(2):251–254.

11. Ko E, Mortimer E, Fraire AE. Extraarticular synovial chondromatosis: review of epidemiology, imaging studies, microscopy and pathogenesis, with a report of an additional case in a child. Int J Surg Pathol. 2004; 12(3):273–280.

12. McKenzie G, Raby N, Ritchie D. A pictorial review of primary synovial osteochondromatosis. Eur Radiol. 2008; 18(11):2662–2669.

13. Edeiken J, Edeiken BS, Ayala AG, Raymond AK, Murray JA, Guo SQ. Giant solitary synovial chondromatosis. Skeletal Radiol. 1994; 23(1):23–29.

14. Davis RI, Hamilton A, Biggart JD. Primary synovial chondromatosis: a clinicopathologic review and assessment of malignant potential. Hum Pathol. 1998; 29(7):683–688.

15. Mora R, Soldini A, Raschella F, Paparella F, Belluati A, Basile G. Primitive synovial chondromatosis of the hip joint. Ital J Orthop Traumatol. 1992; 18(2):231–239.




 PDF
PDF ePub
ePub Citation
Citation Print
Print








 XML Download
XML Download