Abstract
Background
For early detection of developmental dysplasia of the hip (DDH), neonatal hip screening using clinical examination and/or ultrasound has been recommended. Although there have been many studies on the reliability of both screening techniques, there is still controversy in the screening strategies; clinical vs. selective or universal ultrasound screening. To determine the screening strategy, we assessed the agreement among the methods; clinical examination by an experienced pediatric orthopedic surgeon, sonographic morphology, and sonographic stability.
Methods
From January 2004 to June 2009, a single experienced pediatric orthopedic surgeon performed clinical hip screenings for 2,686 infants in the neonatal unit and 43 infants who were referred due to impressions of hip dysplasia before 3 months of age. Among them, 156 clinically unstable or high-risk babies selectively received bilateral hip ultrasound examinations performed by the same surgeon using the modified Graf method. The results were analyzed statistically to detect any correlations between the clinical and sonographic findings.
Results
Although a single experienced orthopedic surgeon conducted all examinations, we detected only a limited relationship between the results of clinical and ultrasound examinations. Ninety-three percent of the clinically subluxatable hips were normal or immature based on static ultrasound examination, and 74% of dislocating hips and 67% of limited abduction hips presented with the morphology below Graf IIa. A total of 80% of clinically subluxatable, 42% of dislocating and 67% of limited abduction hips appeared stable or exhibited minor instability on dynamic ultrasound examination. About 7% of clinically normal hips were abnormal upon ultrasound examination; 5% showed major instability and 3% showed dysplasia above Graf IIc. Clinical stability had small coefficients between ultrasound examinations; 0.39 for sonographic stability and 0.37 for sonographic morphology. Between sonographic stability and morphology, although 71% of hips with major instability showed normal or immature morphology according to static ultrasound examination, the coefficient was as high as 0.64.
Conclusions
Discrepancies between clinical and ultrasound examinations were present even if almost all of the exams were performed by a single experienced pediatric orthopedic surgeon. In relation to screening for DDH, it is recommended that both sonographic morphology and stability be checked in addition to clinical examination.
Established developmental dysplasia of the hip (DDH) represents one of the more common musculoskeletal disorders in childhood, with a reported prevalence of 0.1–2 per 1,000 infants.123) The wide range reflects differences in screening strategies (clinical vs. selective or universal ultrasound [US] screening), differences in the indications for treatment, and differences in the definitions of early and late DDH.
For early detection of DDH, neonatal hip screening was advocated by von Rosen.4) Indeed, neonatal hip screening using clinical examination techniques has shown excellent results in some reports.5678) However, these methods could not succeed in preventing late presentation of DDH.9101112) The Ortolani and Barlow clinical tests for neonatal hip instability can result in high numbers of false-positive and false-negative results, especially in inexperienced hands.101113) Nevertheless, there is evidence that neonatal clinical examination by expert examiners can favorably influence rates of late presentation.8)
Although US examination either by static or dynamic means is now well established,14) and that US offers specificity and sensitivity in excess of 90%,15) universal screening of all newborns with hip US is not generally recommended. However, screening of all newborn infants with a physical examination followed by selective use of US is widely accepted.11617) We also applied this protocol and provided the result in a previous report.18) On the other hand, previous studies reported that there were some discrepancies between the results from clinical examination and US examination.1920) However, those studies had limitations: clinical examinations were performed by a group of examiners of varying levels of experience, and different examiners performed the clinical and US examinations. These factors may have resulted in a lack of concordance between the two screening methods. There may have been technical issues that arose due to the relative inexperience of the examiners, possible interobserver error from clinical examination, or operator dependency in relation to how US examinations were performed or interpreted.
Therefore, we prospectively assessed the level of agreement between clinical instability, sonographic morphology and sonographic instability, when one experienced pediatric orthopedic surgeon performed both the clinical examinations and selective US examinations for all babies.
In Korea University Anam Hospital, neonatal hip screening using selective ultrasound had been performed since 1996 according to the same protocol. All the babies in the neonatal units received a physical examination within 1 week after birth or admission to the neonatal unit by one experienced pediatric orthopedic surgeon. Babies referred from other institutes under the presumptive impression of hip dysplasia also received the same hip screening procedure at the time of visiting the pediatric orthopedic department. From January 2004 to June 2009, 2,686 babies in neonatal units and 43 babies who were referred before the age of 3 months were included in this study. Of the 2,686 babies who were examined in the neonatal unit, 1,453 babies (54%) were boys and the remaining 1,233 babies (46%) were girls. The distribution of body weight at birth was as follows: 67 babies (2.5%), under 1 kg; 107 (4.0%), 1–1.5 kg; 496 (18.5%), 1.5–2.5 kg; 1,921 (71.5%), 2.5–4.0 kg; and 95 (3.5%), over 4.0 kg.
The Barlow and Ortolani test was used for the physical examinations. Based on the examination results, hips were subjectively divided into the following 5 groups: (1) normal; (2) noisy hip or suspicious instability; (3) subluxatable; (4) dislocatable or dislocated; and (5) limited abduction similar to the clinical assessment of hip stability described by Laborie et al.21)
US examination was selectively performed in babies with abnormalities according to clinical hip examination as described above, risk factors such as leg asymmetry, i.e., different thigh fold and leg length discrepancy, foot deformity or torticollis, and female babies with breech presentation. All US examinations were completed within 2 weeks (most within 1 week) after the clinical examination, and were performed for both hips by the same pediatric orthopedic surgeon who did the clinical screening, or under his supervision. US examination was performed using the 7.5 MHz linear US transducer and iU22 (Philips Ultrasound, Bothell, WA, USA) real-time US machine was used.
According to Graf methods,22) coronal scans of each hip were obtained, and significant emphasis was placed on producing the correct standard section. Based on morphological features and the alpha and beta angles, the hips were divided into 4 groups according to a modified version of the Graf method:23) (1) Graf I (normal); (2) Graf IIa (immature); (3) Graf IIc (minor dysplasia); and (4) Graf IId or higher dysplasia (major dysplasia which needs treatment).
In order to determine hip stability by ultrasound, a modified Barlow maneuver (a provocation test) was performed during US examination. Based on the concentricity and the gap between the acetabulum and femoral head, US stability of the hips was divided into 4 groups according to a modified version of the Rosendahl method.24) These groups are (1) stable: no gap or minimal gap between the femoral head and acetabulum, or slight cranial deflection of the labrum; (2) minor instability: a gap can be visualized between the femoral head and the acetabulum; (3) major instability: a gap over 1/2 of the acetabular depth including dislocatable but relocated after release of stress; and (4) dislocated without stress. Under the these definitions, stable hips were categorized as normal and recommended for open follow-up, and hips with minor instability were considered borderline and recommended for regular US follow-up without treatment until normal US morphology and stability were obtained. The hips with major instability were recommended for close US observation with treatment such as Pavlik methods.
The classified grades for clinical stability, sonographic stability and sonographic morphology were compared respectively. From clinical examination, the 'limited abduction' group, which is not associated with hip instability itself, was not included. The associations of grades of the 3 examinations were checked using correlation analysis and Kendall's coefficient of concordance. The statistical evaluation was performed using SPSS ver. 12.0 (SPSS Inc., Chicago, IL, USA) and p-values less than 0.05 were considered statistically significant.
Of the 2,729 babies included in this study, selective US examinations were performed for 156 babies (5.7%). Clinical abnormalities in 115 babies (19 hip noise, 77 subluxatable, 10 dislocating or dislocated, and 9 limited abduction on the worse side) led to US examination. Additionally, 41 babies with clinically normal hips underwent US examination due to the presence of one or more of the risk factors described earlier. US examination was performed in both hips of 156 babies, giving a total of 312 hips. Clinical presentations of the 312 hips, which received US examination, were as follows; normal hips in 176 (56.4%), hip noise in 26 (8.3%), subluxatable hips in 82 (26.3%), dislocating or dislocated hips in 19 (6.1%), and limited abduction of hips in 9 (2.9%). For assessment of sonographic morphology, 223 hips (72%) were Graf I, 70 hips (22%) were Graf IIa, 14 hips (4%) were Graf IIc, and 5 hips (2%) were Graf IId or higher. Sonographic instability assessment revealed that 203 hips (65%) were normal, 68 hips (22%) had minor instability, 38 hips (12%) had major instability, and 3 hips (1%) were dislocated.
The correlation analysis between sonographic morphology and sonographic stability is shown in Table 1. Among the 203 hips that were stable on dynamic US examination, 188 (92.6%) were Graf I (normal morphology), 14 (6.9%) were Graf IIa, and only 1 (0.5%) was Graf IIc. None were Graf IId or higher on static US examination. Among the 68 hips that had minor instability, 64 (94.1%) were Graf I or Graf IIa and 4 (5.9%) were Graf IIc. Of the 38 hips included in the major instability group, 7 (18.4%) were Graf I, 20 (52.6%) were Graf IIa, 9 (23.7%) were Graf IIc, and the remaining 2 (5.3%) were Graf IId or higher. All 3 dislocated hips were Graf IId or higher dysplasia on dynamic US examination. Among the 223 hips grouped as Graf I on static US examination, 216 (96.9%) were stable or had minor instability on dynamic US examination, but all 5 dysplastic hips had major instability or were dislocated on dynamic US examination. Additionally, 71% (27 of 38) of the hips with major instability on dynamic US examination were Graf I or IIa on static US examination. The Kendall's coefficient of concordance was 0.64, implying a positive correlation between sonographic morphology and stability.
Among the 176 hips adjudged as normal on clinical examination, 171 (97.2%) were Graf I or IIa on static US examination. All 26 noisy hips were Graf I or IIa on static US examination. Of the 82 subluxatable hips, 76 (92.7%) were Graf I or IIa, only 3 (3.6%) were Graf IIc, and the remaining 3 hips were Graf IId or higher. Fourteen (73.7%) of the 19 dislocating or dislocated hips were Graf I or IIa on static US examination, while the remaining 5 hips (26.3%) were Graf IIc or higher. Five of the 9 limited abducted hips were Graf I, 1 hip was Graf IIa, 3 hips were Graf IIc, and no hip were Graf IId or higher (Table 2). The hips of limited abduction were excluded in the correlation analysis because this finding could be caused by adduction contracture of the hip in babies with congenital pelvic obliquity (a feature of moulded baby syndrome), and is not associated with clinical instability. Clinical stability and sonographic morphology were weakly correlated, with a correlation coefficient of 0.37.
Among the 176 hips adjudged normal on clinical examination, 141 (80.1%) were stable on dynamic US examination, 27 (15.3%) had minor instability, and the remaining 8 (4.5%) had major instability. Among the 26 noisy hips, only 2 (7.7%) exhibited major instability, while out of the 82 subluxatable hips, 63 (76.8%) were stable or had minor instability, 18 hips (21.9%) had major instability and 1 hip was dislocated on dynamic US examination. Only one of the 19 dislocating hips was stable and 7 had minor instability. On dynamic US examination, these 8 hips (42.1%) were included as normal variants. Of the 9 limited abduction hips, 6 hips were stable, 2 had minor instability, and 1 had major instability (Table 3). The correlation coefficient between clinical stability and sonographic stability was only 0.39, indicating a weak correlation between the results of the 2 examinations.
The purpose of current study was to clarify the correlation between clinical examination and sonographic result in neonatal hip screening for DDH. Despite the fact that all procedures in our study were performed or supervised by one experienced pediatric orthopedic surgeon, the correlations between clinical stability and sonographic results were weak. Under the assumption that US examination is more reliable than clinical examination, these weak correlations contradict the suggestions of some previous studies. The findings in this study suggest that 'only clinical examination' has definite limitations as a diagnostic tool for DDH.
Paton et al.2) had reported that an abnormality was not found on US examination in an at-risk infant with a clinically normal hip, and that the routine development of targeted US screening for at-risk hips as a national program could not be justified based on a cost-benefit analysis. Another study reported a high association between hip US morphology and stability.25) However, the interobserver reliability of clinical and US examinations for DDH is low in much of the literature. This low sensitivity may be partly explained by technical problems arising from the involvement of many examiners of different levels of experience,262728) or by interobserver variability in US image acquisition and measurement.29) Therefore, they emphasized the need for an experienced examiner to ensure screening accuracy.262728) All examinations in this study were performed or supervised by one experienced pediatric orthopedic surgeon so as to minimize the bias from inexperienced examiners and to reduce interobserver error, but still the correlation was found to below. A previous study also reported that sonography after physical examination by even experienced orthopedic surgeons led to a change in diagnosis in 52% of hips and a change in the management plan among 32% of hips.30) These findings demonstrated the risk of 'neonatal hip screening by only clinical examination.'
The correlation between sonographic morphology and stability was strong in this study, and this finding is consistent with that of Rosendahl et al.23) who reported that morphology and stability are strongly associated in neonatal hips. The correlation coefficient in that report was 0.95, indicating a stronger correlation than that observed in this study. This difference may be due to the difference in the scope of US examination application (i.e., universal or selective). The majority of cases included in the study by Rosendahl et al.23) had clinically normal hips that also exhibited normal US findings. In contrast, only hips with suspected DDH by clinical screening were included in this study, implying that the correlation between sonographic stability and morphology is also strong in neonatal hips with suspected DDH.
However, there are some cases showing inconsistencies between the 2 types of US examinations in this study. Major instability on dynamic US examination is a meaningful finding for treatment and follow-up, but most of the hips with major instability were Graf IIa or below. Normal morphology (Graf I) was also observed in 18% of those hips on static US examination. Malkawi et al.19) reported a similar result in which there were many unstable hips with sonographic normal or immature –but not dysplastic– morphology in the neonatal period because bony changes took longer to be seen or become evident. Rosendahl et al.2425) also reported that 25%–49% of unstable hips had normal or immature morphology. This study supports that report. This discordance suggests that there are many unstable hips with normal morphology, and the use of static US examination only, which was recommended by some authors,31) may lead to an underestimation of instability.
Limited abduction is a clinically significant finding that is usually assumed to be a diagnostic clue for DDH, and was found in 9 hips. Among these, only one hip had major instability on dynamic US examination, 3 hips had Graf IIc dysplasia, but no hip was dislocated. This result indicates that some hips that exhibited limited abduction at this age were not related to DDH. Congenital pelvic obliquity with adduction contracture of the hip, a feature of moulded baby syndrome, could show the same clinical finding due to abduction contracture.9) Because clinical examination cannot distinguish this feature from hip dysplasia, hips with limited abduction should be examined by US in order to confirm whether the hip is dysplastic or not.
The course of management of hips in this study was decided based upon morphology and stability after US examination, comparable to the protocol of Rosendahl et al.27) Babies with normal US morphology and stability were discharged with no treatment. Any babies with hips of abnormal US morphology or instability underwent US follow-up with or without treatment, using the Pavlik method until normal US morphology and stability were obtained. Treatment with Pavlik methods was applied to 44 babies. These babies were (1) of Graf IId or higher on US morphology; (2) of major instability or dislocated on dynamic US; and (3) had failed normalization of type Graf IIb or IIc on US morphology, or minor instability on US. The incidence of treatment in this study does not reflect the true rate of the usual population. The rather higher rate of treatment may be explained by the characteristics of sample used in this study. For example, one factor is that most babies included in this study were referred from another hospital for various causes during the neonatal period; another is the inclusion of 43 babies who were referred after screening at another hospital, and who were presumed to have higher incidence of DDH.
Previous studies have reported that universal US screening can prevent late-presenting DDH.332) However, other authors have reported on cases of DDH undetectable by US examination.133) Therefore, 'surveillance for late-presenting DDH' is recommended and applied.721) The current study demonstrates the limitation of 'clinical screening only' in the neonatal period in terms of detection of hip dysplasia and decisions for treatment. This may suggest that 'clinical screening only' should be followed by surveillance or alternatively supplemented with selective or universal US screening to minimize the incidence of the late-presenting DDH.
This study has its own limitations. There was a time gap between the clinical and US examinations. The interval varied from 3 hours to 2 weeks, with an average period of 5 days. Although this interval is not particularly long, the status of the hip could have changed during that period. Another limitation of this study is that the sample size is not large. The small sample size was a consequence of the fact that we only included cases for which all examinations were performed by the same experienced orthopedic surgeon.
In conclusion, this study focused on prospective hip screening performed using selective US examination by a single experienced pediatric orthopedic surgeon among babies referred to neonatal units. A disparity between clinical findings and US findings has been identified even when all examinations were performed by a single experienced pediatric orthopedic surgeon. 'clinical examination only' screening has some limitations at this stage. It is therefore recommended that, in addition to clinical examination, checks of both sonographic morphology and stability should be considered in screening for DDH.
Figures and Tables
Table 1
Correlation between Sonographic Stability and Morphology
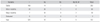
| Variable | I | IIa | IIc | IId, III, IV | Total |
|---|---|---|---|---|---|
| Stable | 188 | 14 | 1 | 0 | 203 |
| Minor instability | 28 | 36 | 4 | 0 | 68 |
| Major instability | 7 | 20 | 9 | 2 | 38 |
| Dislocated | 0 | 0 | 0 | 3 | 3 |
| Total | 223 | 70 | 14 | 5 | 312 |
Table 2
Correlation between Clinical Stability and Sonographic Morphology
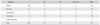
| Variable | I | IIa | IIc | IId, III, IV | Total |
|---|---|---|---|---|---|
| Normal | 149 | 22 | 5 | 0 | 176 |
| Hip noise | 22 | 4 | 0 | 0 | 26 |
| Subluxatable | 43 | 33 | 3 | 3 | 82 |
| Dislocating | 4 | 10 | 3 | 2 | 19 |
| Limited abduction | 5 | 1 | 3 | 0 | 9 |
| Total | 223 | 70 | 14 | 5 | 312 |
References
1. Holen KJ, Tegnander A, Bredland T, et al. Universal or selective screening of the neonatal hip using ultrasound? A prospective, randomised trial of 15,529 newborn infants. J Bone Joint Surg Br. 2002; 84(6):886–890.
2. Paton RW, Hossain S, Eccles K. Eight-year prospective targeted ultrasound screening program for instability and atrisk hip joints in developmental dysplasia of the hip. J Pediatr Orthop. 2002; 22(3):338–341.

3. Rosendahl K, Markestad T, Lie RT. Ultrasound screening for developmental dysplasia of the hip in the neonate: the effect on treatment rate and prevalence of late cases. Pediatrics. 1994; 94(1):47–52.
4. von Rosen S. Diagnosis and treatment of congenital dislocation of the hip hoint in the new-born. J Bone Joint Surg Br. 1962; 44(2):284–291.
5. Barlow TG. Early diagnosis and treatment of congenital dislocation of the hip. J Bone Joint Surg Br. 1962; 44(2):292–301.

6. Bernard AA, O'Hara JN, Bazin S, Humby B, Jarrett R, Dwyer NS. An improved screening system for the early detection of congenital dislocation of the hip. J Pediatr Orthop. 1987; 7(3):277–282.

7. Goss PW. Successful screening for neonatal hip instability in Australia. J Paediatr Child Health. 2002; 38(5):469–474.

8. Macnicol MF. Results of a 25-year screening programme for neonatal hip instability. J Bone Joint Surg Br. 1990; 72(6):1057–1060.

9. Lennox IA, McLauchlan J, Murali R. Failures of screening and management of congenital dislocation of the hip. J Bone Joint Surg Br. 1993; 75(1):72–75.

10. MacKenzie IG, Wilson JG. Problems encountered in the early diagnosis and management of congenital dislocation of the hip. J Bone Joint Surg Br. 1981; 63(1):38–42.

11. Krikler SJ, Dwyer NS. Comparison of results of two approaches to hip screening in infants. J Bone Joint Surg Br. 1992; 74(5):701–703.

12. Sanfridson J, Redlund-Johnell I, Uden A. Why is congenital dislocation of the hip still missed? Analysis of 96,891 infants screened in Malmo 1956-1987. Acta Orthop Scand. 1991; 62(2):87–91.

13. Palmen K. Prevention of congenital dislocation of the hip: the Swedish experience of neonatal treatment of hip joint instability. Acta Orthop Scand Suppl. 1984; 208:1–107.
14. Jones DA, Powell N. Ultrasound and neonatal hip screening: a prospective study of high risk babies. J Bone Joint Surg Br. 1990; 72(3):457–459.

15. Rosenberg N, Bialik V, Norman D, Blazer S. The importance of combined clinical and sonographic examination of instability of the neonatal hip. Int Orthop. 1998; 22(3):185–188.

16. Mahan ST, Katz JN, Kim YJ. To screen or not to screen? A decision analysis of the utility of screening for developmental dysplasia of the hip. J Bone Joint Surg Am. 2009; 91(7):1705–1719.

17. Schwend RM, Schoenecker P, Richards BS, Flynn JM, Vitale M. Pediatric Orthopaedic Society of North America. Screening the newborn for developmental dysplasia of the hip: now what do we do? J Pediatr Orthop. 2007; 27(6):607–610.
18. Lee SH, Park SW, Lee KS, Byun YS, Ha KW, Lee BT. Selective ultrasonography and screening of neonatal hip. J Korean Orthop Assoc. 2000; 35(4):651–656.

19. Malkawi H, Asir B, Tadros F, Khasawneh Z. Sonographic image of the newborn hip with positive Ortolani's sign. Clin Orthop Relat Res. 1992; (279):138–143.

20. Rosendahl K, Markestad T, Lie RT. Congenital dislocation of the hip: a prospective study comparing ultrasound and clinical examination. Acta Paediatr. 1992; 81(2):177–181.

21. Laborie LB, Markestad TJ, Davidsen H, et al. Selective ultrasound screening for developmental hip dysplasia: effect on management and late detected cases. A prospective survey during 1991-2006. Pediatr Radiol. 2014; 44(4):410–424.

22. Graf R. Fundamentals of sonographic diagnosis of infant hip dysplasia. J Pediatr Orthop. 1984; 4(6):735–740.

23. Rosendahl K, Markestad T, Lie RT. Developmental dysplasia of the hip: a population-based comparison of ultrasound and clinical findings. Acta Paediatr. 1996; 85(1):64–69.

24. Rosendahl K, Markestad T, Lie RT. Ultrasound in the early diagnosis of congenital dislocation of the hip: the significance of hip stability versus acetabular morphology. Pediatr Radiol. 1992; 22(6):430–433.

25. Rosendahl K, Markestad T, Lie RT. Developmental dysplasia of the hip: prevalence based on ultrasound diagnosis. Pediatr Radiol. 1996; 26(9):635–639.

26. Dias JJ, Thomas IH, Lamont AC, Mody BS, Thompson JR. The reliability of ultrasonographic assessment of neonatal hips. J Bone Joint Surg Br. 1993; 75(3):479–482.

27. Rosendahl K, Aslaksen A, Lie RT, Markestad T. Reliability of ultrasound in the early diagnosis of developmental dysplasia of the hip. Pediatr Radiol. 1995; 25(3):219–224.

28. Shipman SA, Helfand M, Moyer VA, Yawn BP. Screening for developmental dysplasia of the hip: a systematic literature review for the US Preventive Services Task Force. Pediatrics. 2006; 117(3):e557–e576.

29. Omeroglu H, Bicimoglu A, Koparal S, Seber S. Assessment of variations in the measurement of hip ultrasonography by the Graf method in developmental dysplasia of the hip. J Pediatr Orthop B. 2001; 10(2):89–95.

30. Ashby E, Roposch A. Diagnostic yield of sonography in infants with suspected hip dysplasia: diagnostic thinking efficiency and therapeutic efficiency. AJR Am J Roentgenol. 2015; 204(1):177–181.

31. Lewis K, Jones DA, Powell N. Ultrasound and neonatal hip screening: the five-year results of a prospective study in high-risk babies. J Pediatr Orthop. 1999; 19(6):760–762.





 PDF
PDF ePub
ePub Citation
Citation Print
Print



 XML Download
XML Download