Abstract
Background
Percutaneous iliosacral screw fixation can provide stable fixation with a minimally invasive surgical technique for unstable posterior pelvic ring injuries. This surgical technique is not limited by cases of difficult fracture patterns, sacral dysplasia, and small sacral pedicles that can occur in Asians. The purpose of this study was to investigate the incidence of the sacral dysplasia in the Korean population and determine the optimal direction of iliosacral screws by analyzing pelvic three-dimensional computed tomography (3D-CT) scans.
Methods
One hundred adult patients who had pelvic 3D-CT scans were evaluated. The upper sacral morphology was classified into three groups, i.e., normal, transitional, and dysplastic groups; the cross-sectional area of the safe zone was measured in each group. S1 pedicle with a short width of more than 11 mm was defined as safe pedicle. The incidences of safe pedicles at different angles ranging from 0° to 15° were investigated in order to determine optimal angle for screw direction.
Results
The incidence of normal, transitional, and dysplastic group was 46%, 32%, and 22%, respectively. There were significant increases of the cross-sectional area of the safe zones by increasing the angles from 0° to 15° in all groups. The incidence of safe pedicles increased similar to the changes in cross-sectional area. The overall incidence of safe pedicles was highest at the 10° tilt angle.
Conclusions
The incidence of sacral dysplasia in Koreans was 54%, which is higher than previous studies for Western populations. The cross-sectional area of the safe zone can be increased by anteromedial direction of the iliosacral screw. Considering the diversity of sacral morphology present in the Korean population, a tilt angle of 10° may be the safest angle.
Percutaneous iliosacral screw fixation can provide appropriate biomechanical stability while minimizing further soft tissue injury for fixation of unstable posterior pelvic ring injuries including sacroiliac joint dislocations, sacral fractures, and some sacroiliac joint fracture dislocations.123) Intraoperative fluoroscopic images have been commonly used by examining the inlet and outlet views with a lateral anatomical landmark of the iliac cortical density (ICD) for safe insertion of an iliosacral screw. However, the presence of contrast, intestinal gas, and increased soft tissue density from obesity can cause difficulty in obtaining and interpreting appropriate intraoperative fluoroscopic images. This may lead to malpositioned implants and increased risk of neurovascular injuries.4567) The morphologic variability of the posterior pelvic ring has been studied and radiographic correlations documented. The presence of sacral dysplasia can cause difficulty in placement of screws due to the decreased size of the safe zone.8) To our knowledge, there has been a lack of studies on the variability of the upper sacral segment anatomy as well as the incidence of sacral dysplasia in Asian populations.
The purpose of this study was to investigate the incidence of sacral dysplasia in the Korean population and determine the optimal direction of iliosacral screws by analyzing pelvic three-dimensional computed tomography (3D-CT) scans.
In order to obtain anatomic data necessary to iliosacral screw fixation for Koreans, the upper sacral morphology was classified based on the relationship of sacral body and ala with the radiological characteristics of sacral dysplasia suggested by Routt et al.8) In addition, the cross-sectional areas of the safe zones and the short width around the pedicle were measured using 3D-CT in order to determine the optimal angle of the iliosacral screw; for this purpose, a safe pedicle was defined as the minimum area where a 7.0 mm cannulated screw can be safely placed in the pedicle.
We evaluated the 3D-CT of 100 patients who had visited for pelvic bone checkup. Patients who had traumatic posterior pelvic ring injuries or any evidence of hip dysplasia were excluded. There were 54 males and 46 females with an average age of 46 years (range, 35 to 62 years).
3D-CT scans were obtained by two types of the 16 channel CT scanning equipment (GE ULTRA 16, GE Healthcare, Milwaukee, WI, USA; Siemens Somatom Sensation 16, Siemens, Erlangen, Germany). The slice intervals were at 0.6 mm and 0.62 mm, while the angle was at 0.1° with the precision of 0.1 mm in length. The tomographic images were reconstructed using Advantage Windows 4.1 of the GE Medical System to obtain 3D transparent images. In order to investigate the cross-sectional areas and short width of the safe zones along different angles, we used the oblique sagittal images on multiplanar reformation images that consisted of the axial, sagittal, coronal, and oblique sagittal images in the same screen (Fig. 1). The oblique sagittal images could be simultaneously generated after choosing the points and cross section on the axial image, and their cross sections were shown perpendicular to the sliced plane.
For the incidence of sacral dysplasia, the upper sacral segment morphology was classified as normal, transitional, and dysplastic according to the radiological characteristics, as defined by Routt et al.8) In addition, the amount of prominence of the S1 sacral body over the ICD was measured on reconstructed transparent lateral 3D images. Patients who had no radiographic characteristics of sacral dysplasia and only the sacral promontory superior to the ICD on the lateral view were classified as normal. The patients with some radiographic characteristics of sacral dysplasia and less than half of the S1 sacral body superior to the ICD were classified as the transitional group. The patients with radiographic signs of dysplasia and more than half of the S1 sacral body superior to the ICD were classified as dysplastic (Fig. 2).
For the measurement of the cross-sectional areas of the safe zones, we manually drew outer lines along the pedicle on the oblique sagittal images, which isolated the osseous pathway posterior to the anterior border of the sacral body, anterior to the neuroforaminal tunnel, and inferior to the sacral ala and ICD. This area was calculated for the segment of the S1 osseous pathway from the lateral side of the first sacral neural foramen to its medial side. The area of the safe zone was defined as the area inside the greatest common outer lines that did not violate the cortex of the sacrum anteriorly or superiorly nor the neuroforaminal tunnel posteriorly (Fig. 3). The cross-sectional areas were calculated automatically by the function of the software.
A safe pedicle was defined in patients in which the minimum length of the short width of the safe zone was at least 11 mm. This was considered a wide enough space for the placement of one 7.0-mm cannulated screw with 2 mm margins on both sides of the screws.
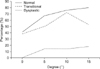
We measured the cross-sectional areas of the safe zones around the pedicle and the lengths of its short widths (Fig. 4) and investigated the incidence of safe pedicle with different angles ranging from 0° to 15° with 5° intervals in order to determine optimal angle for screw direction.
Radiological classification for sacral dysmorphism of 100 Korean adults, according to the degree of sacral protrusion above ala and radiographic characteristics as defined by Routt et al.,8) showed that the normal group was 46%, the transitional group 32%, and the dysplastic group 22% in incidence.
The mean cross-sectional areas and short width of the safe zone in the normal group were 229.4 ± 60.4 mm2 and 12.5 ± 2.7 mm at 0° tilt angle.
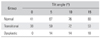
In the transitional group, the mean cross-sectional areas of the safe zones was 163.4 ± 96.6 mm2 and the mean short width of the safe zone was 9.9 ± 4.3 mm; whereas, those in the dysplastic group were 45.2 ± 47.6 mm2 and 4.1 ± 2.2 mm at 0° tilt angle (Table 1).
The mean cross-sectional areas of the safe zones in the three groups at 5° tilt angle were 274.2 ± 59.8 mm2, 214.7 ± 90.9 mm2, and 110.9 ± 80.2 mm2, while by the 10° tilt angle, they were 295.5 ± 58.1 mm2, 249.6 ± 82.7 mm2, and 157.3 ± 76.0 mm2, respectively.
At the 15° tilt angle, the mean cross-sectional area of safe zones were 298.3 ± 57.2 mm2, 264.2 ± 70.0 mm2, and 199.8 ± 65.7 mm2, in the three groups, indicating that the mean cross-sectional areas of safe zones gradually increased as the tilt angle moved from the horizontal 0° to 15° tilt angle.
According to our definition of safe pedicle, the incidences of the safe pedicle at 0° tilt angle were 41% in the normal group, 38% in the transitional group, and 0% in the dysplastic group. The incidences of the safe pedicle at 5° tilt angle were 67% in the normal group, 50% in the transitional group, and 14% in the dysplastic group.
At 10° tilt angle, the incidence was 76%, 72%, and 14% in each of the three groups, respectively; at the 15° tilt angle, the incidences were 80%, 53%, and 18%, respectively (Table 2).
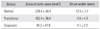
The incidences of the safe pedicle continued to increase as the tilt angle moved from the horizontal 0° tilt to 15° tilt angle in each of the groups, but decreased in the transitional group at 15° tilt angle, indicating that overall incidence of the safe pedicle was highest at 10° tilt angle (Fig. 5).
Unstable posterior pelvic ring injuries are successfully stabilized by percutaneous iliosacral screw fixation. This allows for biomechanically stable fixation through a minimally invasive method.91011)
In order to avoid neurovascular injuries during percutaneous insertion of screws, surgeons are required to pay special attention to locate and verify specific radiologic landmarks on intraoperative fluoroscopic images. However, clear fluoroscopic images are difficult to acquire in cases of obesity, use of contrast, intestinal gas, and unreduced fractures. This may lead to a higher incidence of misplaced iliosacral screws, which might increase the risk of neurovascular injuries. In addition, variations of upper sacral segment anatomy can make it more difficult for surgeons to place the screws into the safe zone of the sacrum.4567)
The anatomical characteristics of the safe zone and variations of the upper sacral morphology have been reported, but similar studies for the Asian population are lacking.121314) The Asian population tends to be smaller in stature than the Western population. This difference reportedly has an impact on the size and design of implants commonly used to treat orthopedic injuries. The dysmorphic sacrum has several key characteristics. The upper portion of the sacrum is relatively colinear with the iliac crests on the outlet radiographic view. Other characteristics include the presence of mammillary bodies, larger and irregular anterior upper sacral foramina, residual upper sacral disks, an acute alar slope oriented from cranial-posterior-central to caudal-anterior-lateral on the outlet and lateral views of the sacrum, a tongue-in-groove sacroiliac joint surface visualized on CT, and cortical indentation of the anterior ala on the inlet radiographic view.815) Recognizing these radiographic features and their impact on the available osseous fixation pathway is crucial for safe placement of iliosacral screws.
This study showed that the incidence of the upper sacral dysplasia of Koreans was 54% (32% in the transitional group and 22% in the dysplastic group).
Besides ethnic differences, difference in incidence of sacral dysplasia could also result from differences in radiographic image used for evaluation of sacral dysplasia. In this study, the 3D-CT scan images were used instead of the radiographic outlet images used by Routt et al.,8) which facilitated more detailed examination. Another possible reason for difference in incidence of sacral dysplasia could be that we added one more criteria on radiographic characteristics proposed by Routt et al.8) in order to define the sacral dysplasia. Those cases in which most of the sacral body protruded above ICD in lateral image were classified as the definite dysplastic group; this was indicative of little overlapped area between sacral body and sacral ala, and hence, difficulty in obtaining a safe corridor of iliosacral screws.
Throughout this study, there was need for a sufficient level of preoperative attention due to the relatively high incidence of sacral dysplasia in Koreans; furthermore, the cross-sectional area and short width of safe zone in the dysplastic group was smaller than that in other groups, which require an alternative fixation method instead of iliosacral screw.
Most of the studies on the safe zone for iliosacral screw through CT scans as well as cadaveric experiments indicate that since the pedicle is the narrowest area linking the sacral body with its ala, it could be the most important structure.5916171819) Examination of the safe area and shape of the pedicle suggested that the safe zone is the 3D safe path with the most commonly shared areas across consecutive images of the pedicle, rather than the narrowest spots in the pedicle (Fig. 2). Thus, inserting the screws along the axis of the pedicle from the posterolateral toward the anteromedial side would be more effective in obtaining a wider safe zone than horizontal direction.1417)
Day et al.17) described a modified oblique pelvic landmark method in which tilting the true lateral images approximately 10° to 20° could be more accurate and safer for percutaneous iliosacral screw fixation. Kim et al.18) reported that the mean axis of the first pedicle of Koreans was at 32.5°. However, in our study, an extension of the safe zones along the axis of the pedicle resulted in violation of the anterior cortex of the sacral body; hence, it is important to determine an appropriate direction of the iliosacral screw between the true lateral direction and the axial direction of the pedicle for safe insertion of a iliosacral screw with proper length.
Accordingly, we measured the changes in the cross-sectional areas of the safe zones by increasing the tilt angles from 0° to 15° with interval of 5° since exceeding 20° of screw direction could violate the anterior cortex of the sacral body and might be difficult in clinical setting.
Our study showed that there were significant increases of the cross-sectional area of the safe zones by increasing the angles from 0° to 15° in all groups. Compared with the 0° tilt angle, the cross section of the safe zones at 15° tilt angle increased 31% in the normal group, 61% in the transitional group, and 342% in the dysplastic group.
A study on the safe zones based on the diameters of screws by Day et al.17) showed that the critical dimension of the safe zones on the basis of a screw was 7.3 mm. The authors defined "safe pedicle" as the case in which the dimension of the pedicle of over 11 mm was large enough to accommodate a 7.0-mm screw with 2-mm margins on both side of a screw; this provides a clinically safer critical dimension of the safe zone. We attempted to determine the safest angle of a screw by examining the incidence of the safe pedicle based on changes in the tilt angles.
This study showed that the incidence of safe pedicle at the 0° tilt angle in the normal group was only 41%, and no safe pedicle in the dysplastic group; furthermore, by increasing the tilt angles from 0° to 15°, the incidences of safe pedicle increased similar to the changes of cross-sectional area, which indicated that anteromedial direction of the screw could be safe, not violating cortical bones of the sacrum. However, in the transitional group, the incidence of the safe pedicle at the 15° tilt angle decreased, as compared to 10° tilt angle from 72% to 53%. Thus, overall incidence of the safe pedicle was highest at the 10° tilt angle, which means that considering the morphological diversity of the sacrum, about 10° anteromedial direction of the iliosacral screw would be safe in clinical practice.
The limitations of this study were the lack of consideration of the superomedial direction of the safe zone and lack of combined cadaveric experiments. However, our study has important implications for the development of criteria of sacral dysplasia and safe optimal tilt angle for iliosacral screw fixation in Koreans.
In conclusion, the incidence of sacral dysplasia in Korean adults was 54%, which is higher than previous studies on Western populations; and even in the normal group, the incidence of the safe pedicle at the 0° tilt angle was only 41%. The cross-sectional area of the safe zone can be increased by anteromedial direction of the iliosacral screw, but 10° tilt angle may be the safest angle when considering the diversity of sacral morphology of Koreans.
Figures and Tables
Fig. 1
Multiplanar reformation images on the same screen. The oblique sagittal image (A) could be simultaneously generated after choosing the points and cross section on the axial (B), sagittal (C), and coronal (D) images and show their cross sections perpendicular to the sliced plane.
Fig. 2
Classification of upper sacrum morphology for iliosacral screw fixation using transparent three-dimensional reconstruction image. (A) Normal group has no radiologic signs of sacral dysplasia. (B) The transitional group has some radiologic characteristics of sacral dysplasia with less than half of the S1 body protruding above the iliac cortical density (ICD). (C) The dysplastic group has some radiologic characteristics of sacral dysplasia and has more than half of the S1 body located above the ICD.
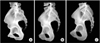
Fig. 3
Oblique sagittal images were obtained along the given axis (arrow) (A). Area of safe zone was defined as the area inside the greatest common outer lines that did not violate the cortex of the sacrum anteriorly or superiorly nor the neuroforaminal tunnel posteriorly. This area was calculated from the lateral side of the first sacral neural foramen (B) to its medial side (C).

Fig. 4
Sagittal computed tomography image showing the cross-sectional area and short width of the safe zone.

References
1. Ebraheim NA, Coombs R, Hoeflinger MJ, Zeman C, Jackson WT. Anatomical and radiological considerations in compressive bar technique for posterior pelvic disruptions. J Orthop Trauma. 1991; 5(4):434–438.
2. Kim HT, Son KM, Cheon SJ, Yoo CI. Treatment of pelvic bone fracture involving the sacrum and sacroiliac joint. J Korean Soc Fract. 2001; 14(3):313–322.

3. Oh JK, Bae SY, Kim JO, Roh KJ, Lee JJ, Chang SY. Radiologic evaluation for the safe zone of percutaneous iliosacral screw fixation. J Korean Soc Fract. 2002; 15(3):336–341.

4. Altman DT, Jones CB, Routt ML Jr. Superior gluteal artery injury during iliosacral screw placement. J Orthop Trauma. 1999; 13(3):220–227.

5. Routt ML Jr, Simonian PT, Mills WJ. Iliosacral screw fixation: early complications of the percutaneous technique. J Orthop Trauma. 1997; 11(8):584–589.

6. Sagi HC, Lindvall EM. Inadvertent intraforaminal iliosacral screw placement despite apparent appropriate positioning on intraoperative fluoroscopy. J Orthop Trauma. 2005; 19(2):130–133.

7. Stephen DJ. Pseudoaneurysm of the superior gluteal arterial system: an unusual cause of pain after a pelvic fracture. J Trauma. 1997; 43(1):146–149.
8. Routt ML Jr, Simonian PT, Agnew SG, Mann FA. Radiographic recognition of the sacral alar slope for optimal placement of iliosacral screws: a cadaveric and clinical study. J Orthop Trauma. 1996; 10(3):171–177.

9. Ebraheim NA, Xu R, Biyani A, Nadaud MC. Morphologic considerations of the first sacral pedicle for iliosacral screw placement. Spine (Phila Pa 1976). 1997; 22(8):841–846.

10. Mirkovic S, Abitbol JJ, Steinman J, et al. Anatomic consideration for sacral screw placement. Spine (Phila Pa 1976). 1991; 16:6 Suppl. S289–S294.

11. Xu R, Ebraheim NA, Robke J, Yeasting RA. Radiologic evaluation of iliosacral screw placement. Spine (Phila Pa 1976). 1996; 21(5):582–588.

12. Conflitti JM, Graves ML, Chip Routt ML Jr. Radiographic quantification and analysis of dysmorphic upper sacral osseous anatomy and associated iliosacral screw insertions. J Orthop Trauma. 2010; 24(10):630–636.

13. Gardner MJ, Morshed S, Nork SE, Ricci WM, Chip Routt ML Jr. Quantification of the upper and second sacral segment safe zones in normal and dysmorphic sacra. J Orthop Trauma. 2010; 24(10):622–629.

14. Wu LP, Li YK, Li YM, Zhang YQ, Zhong SZ. Variable morphology of the sacrum in a Chinese population. Clin Anat. 2009; 22(5):619–626.

15. Miller AN, Routt ML Jr. Variations in sacral morphology and implications for iliosacral screw fixation. J Am Acad Orthop Surg. 2012; 20(1):8–16.

16. Carlson DA, Scheid DK, Maar DC, Baele JR, Kaehr DM. Safe placement of S1 and S2 iliosacral screws: the "vestibule" concept. J Orthop Trauma. 2000; 14(4):264–269.

17. Day CS, Prayson MJ, Shuler TE, Towers J, Gruen GS. Transsacral versus modified pelvic landmarks for percutaneous iliosacral screw placement: a computed tomographic analysis and cadaveric study. Am J Orthop (Belle Mead NJ). 2000; 29:9 Suppl. 16–21.




 PDF
PDF ePub
ePub Citation
Citation Print
Print


 XML Download
XML Download