Abstract
Background
Clinical and radiologic evaluation and analyses of the surgeries using Buechel and Pappas (B-P) knee implants.
Methods
The study was conducted on 60 patients who underwent 94 total knee replacement arthroplasty with B-P knee implants from May 2009 to December 2010. The results were compared to the results of 41 patients who underwent 60 knee joint surgeries using NexGen-LPS implants from January 2008 to August 2009.
Results
The American Knee Society score of the B-P knee group increased from an average of 66.9 (clinical score) and 65.5 (functional score) to 93.4 and 90.3, respectively; while those for the NexGen-LPS group increased from an average of 68.8 (clinical score) and 62.4 (functional score) to 86.3 and 76, respectively. The average ranges of motion of the B-P knee group and the NexGen-LPS group were 119.1° and 114.8°, respectively, before surgery and improved to 121.0° and 123.0° at final follow-up after the surgery. The visual analogue scale scores for the B-P knee group and the NexGen-LPS group improved from 4.7 and 4.6 to 1.4 and 1.8, respectively. The flexion contracture also improved from 5.1° and 6.3° to 0.64° and 1.72°. The tibio-femoral angle for the B-P knee group and the NexGen-LPS group also improved greatly after the surgery, from varus 0.34° and 0.73° each to valgus 6.7° and 6.9°, respectively.
Total knee replacement arthroplasty using implants is the most reliable treatment method for patients with severe degenerative arthritis. Technological developments and improvements in implantation have helped to relieve pain in patients and to realize a recovery of the knee functions. Conventional knee surgery using fixed bearing implants has a high success rate (range, 90% to 95%) of > 10 years survival. However, the motion between the femoral articular surface and flat polyethylene over time reduces the contact surface and causes problems such as toleration of polyethylene, osteolysis, weak bone, and patellofemoral joint problems.1,2,3) Buechel and Pappas (B-P) knee implants were developed to improve the shortcomings mentioned above. This artificial knee implant was designed to optimize the conformity between the femoral articular surface and polyethylene, by rotating platform bearing, also called mobile bearing. This component provides functional stability by use of proper tension control of the surrounding soft tissues of the knee.
Ceramic coating material is used to improve the surfaces of materials. It prevents scratches on the surface of implants by reducing wear rate, as well as osteolysis caused by the wearing of poly-bearings. Preventing corrosion of the implant's surface by ceramic coating extends the life of poly-bearings. This system also increases the contact area, thus reducing pressure per unit area, polyethylene tolerance, and distributes the pressure transmitted to the joint surface.
We conducted a clinical and radiological study of patients who underwent total knee replacement arthroplasty using the B-P knee implant on either one or both knees. Patient satisfaction, function, and joint motion were evaluated. We tried to determine the advantages of the B-P knee system, as compared to the NexGen-LPS (Zimmer, Warsaw, IN, USA).
We studied 60 persons who received 94 total knee replacement arthroplasty through B-P knee implants on, from May 2009 to December 2010, with a minimum 2-year follow-up. A comparative analysis was conducted with the results of 41 people who received 60 artificial total knee replacement arthroplasty through the NexGen-LPS from January 2008 to August 2009. Inclusion criteria for total knee replacement arthroplasty were severe osteoarthritis with Kellgren-Lawrence classification grade 3-4, osteonecrosis, and posttraumatic arthritis or deformity. Exclusion criteria were contraindications of total knee replacement arthroplasty, ongoing infection of knee, and revision arthroplasty cases.
The average age of patients in the B-P knee group was 67.8 years (range, 49 to 82 years), and that in the NexGen-LPS group was 71 years (range, 53 to 87 years); the average follow-up period was 33 months (range, 22 to 42 months) and 48 months (range, 38 to 57 months), respectively. The B-P knee group was composed of 6 males and 54 females, while the NexGen-LPS group was composed of 2 males and 39 females. The cause of injury was degenerative arthritis in both groups. Patient demographics with respect to age, body mass index, and the proportion of males and females were not statistically different between the 2 groups before surgery (p > 0.05) (Table 1).
The operative procedure was conducted via the midvastus approach.4) The gap technique was performed in all B-P knee patients and the measured resection technique was performed in all NexGen-LPS patients, respectively. The fixation of all replacements was done using cement. The removed bone mass of the patient was measured by an electronic scale in reference to the amputated patella, tibia, and femur.
We attempted to prevent postsurgical bleeding and edema using cryo-cuffs and deep venous thrombosis using antithrombotic stockings. The presence of thrombosis was determined by Doppler ultrasound measurement before and 6 weeks after surgery. The drainage tube was normally removed 2-3 days postsurgery, when drainage reached < 100 mL. The day after removal of the drainage tube, passive knee joint exercises using the continuous passive machine were initiated. We conducted physical therapy for weight-bearing and walking, including active and passive joint motion exercise during hospitalization. Most patients achieved > 90° flexion within 10 days and > 120° flexion in 2 weeks, hence they could be discharged. We administered intravenous antibiotics in the first week, followed by oral administration for the subsequent 2 weeks.
A clinical evaluation and a radiological evaluation were performed at 6 weeks, 3 months, 6 months, and every year after surgery in each patient. We evaluated the clinical and functional performance of the knee joint using the performance evaluation criteria of American Association of Hip and Knee Surgeons. We additionally analyzed radiological findings. Furthermore, we compared the levels of pain in patients before and after surgery via visual analogue scale (VAS) score. The range of movement of the knee joint and flexion contracture were measured using an angle meter before surgery and on final follow-up. Analyses were conducted on the data.
We measured the alignment of the legs with weight-bearing anteroposterior views at one year after surgery using the acute angle between the femur and the tibia axis.
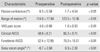
The clinical American Knee Society score (AKSS) improved from 66.9 (range, 58 to 80) to 93.4 (range, 79 to 100) after surgery in the B-P knee patient group, while the NexGen-LPS patient group improved from 68.8 (range, 44 to 89) to 86.3 (range, 62 to 100). There was no difference in the clinical AKSS between the 2 groups before surgery (p > 0.05). Both subject groups demonstrated a significant increase after surgery (p < 0.05). However, the B-P knee group demonstrated a more significant increase than the NexGen-LPS group (p < 0.05).
The function AKSS for the B-P knee group increased from 65.5 (range, 50 to 80) to 90.3 (range, 75 to 100) while it increased from 62.4 (range, 10 to 80) to 76 (range, 10 to 100) for the NexGen-LPS group. There was no difference in the presurgical American Knee Society function scores between the 2 groups (p > 0.05). Both groups showed a significant increase after surgery (p < 0.05). The B-P knee group showed a greater statistically significant increase than the NexGen-LPS group (p < 0.05). Postoperative medial-lateral stability was different between the 2 groups. The percentage of the patients whose medial-lateral stability < 6°, was 73% before surgery and improved to 93% after surgery in the B-P knee patient group, whereas it was 73% before surgery and improved to 79% after surgery in the NexGen-LPS group. The average medial-lateral instability was 2.7° in the B-P knee group and 4.1° in the NexGen-LPS group, which was statistically significant between groups (p < 0.05) (Tables 2 and 3).
The VAS score for degree of pain decreased from 4.69 (range, 3 to 6) to 1.4 (range, 0 to 6) in the B-P knee group, while it decreased from 4.6 (range, 3 to 6) to 1.8 (range, 0 to 6) in the NexGen-LPS group. There was no difference in pain before surgery between the 2 groups (p > 0.05). Pain improvement between the 2 groups from before to after surgery was not significantly different (p > 0.05) (Tables 2 and 3).
The range of motion of the knees increased from 119.1 (range, 10 to 140) to 121 (range, 95 to 140) after surgery for the B-P knee group, while it increased from 114.8 (range, 45 to 140) to 123 (range, 70 to 140) for the NexGen-LPS group. There was no statistically significant difference in the preoperative range of motion of the knees between the 2 groups (p > 0.05). Though the NexGen-LPS group showed a greater range of motion than the B-P knee group, it was not statistically significant (p > 0.05) (Tables 2 and 3).
The flexion contracture was reduced from 5.1° (range, 0° to 40°) to 0.6° (range, 0° to 10°) in the B-P knee group, while it was reduced from 6.3° (range, 0° to 30°) to 1.7° (range, 0° to 20°) in the NexGen-LPS group. There was no statistically significant difference in the preoperative flexion contracture between the 2 groups (p > 0.05). There was greater flexion contracture improvement in the NexGen-LPS group than the B-P knee group, however, it was not statistically significant (p > 0.05) (Tables 2 and 3).
The angle between the femoral and tibial bones from radiography showed an improvement from an average varus of 0.3 to a valgus of 6.7 in the B-P knee group, while it improved from an average varus of 0.7 to a valgus of 6.9 in the NexGen-LPS group. Both groups showed similar improvement with no significant differences (p > 0.05) (Tables 2 and 3).
There were 22 B-P knee patients (41 knee joints) and 14 NexGen-LPS knee patients (23 knee joints) who were in compliance with the bone storage criteria for the bone bank. The removed bone mass was on average 46.85 g (range, 40 to 75 g) for the B-P knee group and 57.82 g (range, 36 to 76 g) for the NexGen-LPS group. The bone mass removed from the B-P knee group was significantly less (p < 0.05) (Table 4).
There was no infection, but there was one case of deep vein thrombosis (DVT) in the B-P knee group. However, one patient who underwent total knee replacement arthroplasty on both knees in the NexGen-LPS group, acquired an infection and underwent further knee revision surgery. Heating sensation and limited range of motion were observed in both knee joints. Methicillin-resistant Staphylococcus aureus was cultured from joint fluid in both knee joints. A prostalac insertion was done in both knees in the first stage and revision was done in the second stage at 6 weeks postantibiotic therapy. There were also 2 cases of DVT within the NexGen-LPS group. There were no liner dislocations in either group.
The purpose of total knee replacement arthroplasty using implants is to reduce the pain, keep the stable motion of the knee, and correct any deformity within the knees. Successful surgeries have been on the rise with the recent developments in knee transplant technology. Additionally, good radiological results and patient satisfaction are also high.5)
The NexGen-LPS system is characterized by a large contact surface area and high joint conformity, due to small concave joint formation with the femoral concave. Ip et al.6) reported that the average knee flexion angle was 115° at 21 months after surgery with posterior-stabilized type NexGen-LPS system. Tests conducted every 2 years by our institute showed an improvement in the range of motion of the knees and conversion to the functional position. Additionally, there have been less complications.7) However, additional research showed that patients with deformities or severe bone loss in the knee joints did not qualify for the NexGen-LPS implant. Several surgeries have resulted in many unstable results, such as the demand for treatment of the patella lateral retinacular release and the high frequency of wearing the transplants. Thus, alternative actions are required.8) The B-P knee implant was designated as an alternative to maximize the contact area between the femoral component and the polyethylene bearing, thus reducing the wear caused by partial contact. With the installation of the pin in front of the tibial component, the probability of the dislocation of the polyethylene bearing and any danger from excessive rotation is reduced. Additionally, the strength and durability of ceramic coated titanium femoral components have greatly increased the life of the B-P knee implant (Fig. 1).
Choi et al.9) discussed patient preferences after the total knee replacement arthroplasty. The percentage of Korean patients who showed a high degree of satisfaction reached 93%. However, there were no adequate improvements in pain and function. For example, patients showed difficulty in rising from the floor and from a squatting position without using their hands. Accordingly, the clinical results of pain and walking would be more important than medical results from the radiological data.
The B-P knee group showed a statistically significant increase in knee scores from an average of 66.9 to 93.4, while the function score increased from 65.5 to 90.3. This result demonstrated a more significant increase in the B-P knee group, as compared to the NexGen-LPS group. Furthermore, the B-P knee group had a relatively excellent outcome similar to previous studies in medial and lateral stability that could affect patient satisfaction postsurgery.
We assumed that the bone mass removed during the knee joint transplant surgery is an important factor in subsequent efficacy of surgery and future re-surgery. If the removed bone mass is large, intraoperative blood loss can be increased. At the revision operation after total knee arthroplasty, there can be surgical difficulties with large bone loss of the tibia and the femur. Bone transplantation, bone cement enhancing screws, metal wedge augmentation, and tibia interposition can be used in revision arthroplasty subsequent to large bone mass removal at primary total knee arthroplasty. We suggest that a suitable resection of bone mass is important not only to lessen intraoperative and postoperative hemorrhage, but also for revision arthroplasty. The average bone masses removed from the knee transplant surgery were 46.85 g and 57.82 g in the B-P knee and NexGen-LPS groups, respectively. This indicated that the B-P knee group recorded a significantly lower bone mass removal (p < 0.05) (Fig. 2).
The tibio-femoral angle after total knee joint arthroplasty is very important for successful results. Lotke and Ecker10) reported that the most favorable angle is from valgus 3° to 7°. Our results showed the tibio-femoral arrangement angle was from varus 0.3° to valgus 6.7° after surgery in the B-P knee group, and from varus 0.7° to valgus 6.9° in the NexGen-LPS group. Deformity correction was satisfactory in both groups.
The dislocation of polyethylene transplants of mobile bearing design reportedly varies from 0% to 9%. Sorrells11) reported that the cause of dislocation may be improper surgery. There were no dislocations of polyethylene implants in this study. The precision of tibial cutting greatly affects the surgery if the knee arthroplasty surgery is conducted using the gap technique. Consequently, it is important to check the precision of cutting with the C-arm at an angle perpendicular to the tibial resection.
This study had limitations, as it was not based on a randomized comparison. However, the study showed that there is no difference between the 2 groups in terms of critical clinical and radiological variables such as flexion angle and range of motion. Moreover, the same operator conducted the same rehabilitation method for the same period. These factors to some extent would compensate for the limitations of this non-randomized comparative study.
We had good results from clinical and radiological evaluations on the knee joint surgery using B-P knee implants. However, the group size may not have been large enough and the follow-up period was not very long. A more developed study for a longer period is needed in future.
The evaluation for > 2 years of total knee replacement arthroplasty using B-P knee implants showed good results. B-P knee implants showed a relatively high degree of satisfaction in clinical knee score and less intraoperative bone mass removal in comparison with NexGen-LPS implants.
Figures and Tables
Fig. 2
(A) Preoperative X-ray of an osteoarthritis (OA) patient: right knee anteroposterior (AP) view shows medial joint space narrowing and varus deformity. (B) Preoperative X-ray of an OA patient: right knee lateral view. (C) Postoperative X-ray of an OA patient with Buechel and Pappas (B-P) knee implants: right knee AP view shows correction of medial joint space narrowing and varus deformity. (D) Postoperative X-ray of an OA patient with B-P knee implants: right knee lateral view.

Table 1
Patient Demographics

Table 2
Comparison of Preoperative and Postoperative Variables in the Buechel and Pappas Knee Group
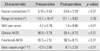
Table 3
Comparison of Preoperative and Postoperative Variables in the NexGen-LPS Group
References
1. Banks S, Bellemans J, Nozaki H, Whiteside LA, Harman M, Hodge WA. Knee motions during maximum flexion in fixed and mobile-bearing arthroplasties. Clin Orthop Relat Res. 2003; (410):131–138.

2. Kim TW, Park SH, Suh JT. Comparison of mobile-bearing and fixed-bearing designs in high flexion total knee arthroplasty: using a navigation system. Knee Surg Relat Res. 2012; 24(1):25–33.

3. Seo SS, Kim CW, Moon SW. A comparison of patella retention versus resurfacing for moderate or severe patellar articular defects in total knee arthroplasty: minimum 5-year follow-up results. Knee Surg Relat Res. 2011; 23(3):142–148.

4. Cooper RE Jr, Trinidad G, Buck WR. Midvastus approach in total knee arthroplasty: a description and a cadaveric study determining the distance of the popliteal artery from the patellar margin of the incision. J Arthroplasty. 1999; 14(4):505–508.
5. Seyler TM, Mont MA, Ragland PS, Kachwala MM, Delanois RE. Sports activity after total hip and knee arthroplasty: specific recommendations concerning tennis. Sports Med. 2006; 36(7):571–583.
6. Ip D, Wu WC, Tsang WL. Early results of posterior-stabilised NexGen Legacy total knee arthroplasty. J Orthop Surg (Hong Kong). 2003; 11(1):38–42.

7. Moon KH, Lee DJ, Lee JS, Kim YT. Total knee replacement arthroplasty with NexGen®-LPS: minimum 5 year follow-up results. J Korean Orthop Assoc. 2011; 46(5):405–411.

8. Lee DC, Sohn OJ. A comparison of mobile-bearing and fixed-bearing total knee arthroplasties in osteoarthritic patients. J Korean Knee Soc. 2007; 19(2):154–160.
9. Choi CH, Kim KW, Sung IH, Park YS. Patient satisfaction interviews after TKA successful rehabilitation achieved and functions still desired by respondents. J Korean Knee Soc. 2006; 18(1):20–25.




 PDF
PDF ePub
ePub Citation
Citation Print
Print



 XML Download
XML Download