Abstract
Multicentric reticulohistiocytosis (MRH) is a rare systemic disease, which commonly manifests as muco-cutaneous papulonodules and inflammatory erosive polyarthropathy. In this research, we report the clinical manifestations and management of a rare case of MRH with destructive arthropathy of bilateral hip joints and arthritis mutilans presenting with characteristic deformities. Disabling hip arthropathy that occurs secondary to MRH can be successfully managed with bilateral total hip arthroplasty (THA). Osteopenia and acetabular bone defects must be anticipated during THA. This case is reported due to its rare occurrence and because little literature has been published regarding THA in such patients.
Multicentric reticulohistiocytosis (MRH), which is also called lipoid dermato-arthropathy or lipoid rheumatism, is a rare multisystem disorder commonly presenting with variegated skin lesions and progressive destructive arthropathy. The exact incidence of the disease is obscure; with less than 200 cases described in the literature.1) The etiology of MRH is unknown, probably immunological. Women are affected three times more often than men, with onset usually in their forties. The cutaneous manifestations may precede, co-exist or follow arthropathy. About 52% of the cases may have mucosal involvement.2) A thorough clinical, radiological and histological evaluation is warranted in all patients with suspected MRH. Our case report describes the clinical presentation and successful management of such a rare case of MRH. To the best of our knowledge, there has not been any literature published on total hip arthroplasty (THA) in MRH.
A 56-year-old male presented with complaints of pain that had gradually been getting worse in both hip regions for the past 4 years. He also had difficulty in walking unassisted, sitting, squatting and climbing stairs. He was a known case of histiocytosis, diagnosed and treated 18 years back for skin lesions. On general physical examination, the patient had deformities of bilateral hands-"opera glass hand" or "la main en lorgnette" deformity-and feet (Fig. 1). Evidence of old healed skin lesions was noticed: multiple violaceous nodules and papules were seen over the back, abdominal wall, thighs and forearm (Fig. 2). On local examination, the patient had painful global restriction of movements of both the hip joints. The patient was ambulant with a four-point walker with an antalgic gait.
A radiographic skeletal survey was done. Plain radiographs of the pelvis with bilateral hips revealed gross obliteration of the joint space, osteopenia, sclerosis and lytic lucencies both on the femoral and the acetabular side on both sides: all features that suggest bilateral hip arthritis (Fig. 3). A radiograph of bilateral hands revealed osteopenia, lytic defects, multiple pathological fractures and dislocations of the phalanges and arthritic changes in the wrist, carpometacarpal, metacarpophalangeal and interphalangeal joints: all features that suggest arthritis mutilans with the classical "pencil-in-a-cup" appearance (Fig. 4). A lateral view of the lumbar spine showed osteopenia and incidental pathological collapse of the L1 and L2 vertebrae (Fig. 4). Haematological investigations were within normal limits except for normocytic normochromic anaemia. Tumour work-up was negative.
In view of the patient's significant pain and functional disabilities and his demand for a pain-free, stable and mobile hip, bilateral sequential THA was planned. The left hip was operated on first, as it was more symptomatic. Cemented THA was performed (Exeter femoral stem and acetabular cup, Stryker, Kalamazoo, MI, USA) (Fig. 5). Intraoperatively, defects in the superior and medial wall of the acetabulum were observed. The defect was filled using an autograft harvested from the osteotomized head and neck of the femur. This was supplemented by a medial wall mesh (X-change, Stryker) for containment. After an uneventful two weeks during the postoperative period, surgeons operated on the right hip. Similar to the left hip, cemented THA using Exeter femoral stem and acetabular cup, Stryker, was performed. A femoral head autograft was used to fill up the acetabular defects. No mesh was used on the right side (Fig. 6). Bone and soft tissue samples were sent for histopathological examination during both surgeries. The postoperative period was uneventful. Weight-bearing with a walker was started after 6 weeks of bed rest. The patient was able to sit unassisted and ambulate with a walker without any discomfort.
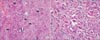
Histopathological examination revealed sheets of multinucleated giant cells in a mixed inflammatory background. The multinucleated giant cells had dense eosinophilic cytoplasm with a ground glass appearance. The mixed inflammatory component comprised of histiocytes, plasma cells and lymphocytes (Fig. 7).
MRH belongs to the category of non-Langerhans cell histiocytoses. This disease usually presents with a myriad of cutaneous manifestations and rapidly progressing destructive arthropathy. The cutaneous manifestations of MRH are highly heterogeneous, commonly presenting as papules and nodules, which may be erythematous, violaceous or flesh-coloured. They can be located anywhere on the body, but, are usually seen over the dorsum of the hands and fingers, periungual regions, pinna of the ears, forearm, elbows and knees.2) They may present in an isolated manner or in a confluent pattern, giving a cobblestone appearance.
Osseoarticular involvement in MRH is characterised by symmetric, erosive, inflammatory polyarthritis. Almost any joint may be involved in arthropathy with predilection for the peripheral joints, especially the distal interphalangeal (DIP) joints. Radiographically, there is evidence of symmetrical well-circumscribed marginal erosions at the joint surface, relatively mild osteopenia and uncalcified soft tissue nodules. The close radiological differential diagnoses at this stage include gout and rheumatoid arthritis. In gout, there is asymmetric joint involvement. In rheumatoid arthritis, DIP joints are rarely involved and there is marked periarticular demineralisation. In nearly 45% of the cases, the arthropathy takes a destructive course culminating in arthritis mutilans.2) Radiologically, the marginal erosion coalesce to involve the entire articular surface leading to loss of articular cartilage, widening of the joint space and marked resorption of sub-chondral bone leading to "pencil-in-a-cup" appearance, foreshortening of the fingers, joint subluxations and/or pathological fractures. Clinically, there might be significant shortening of the fingers leading to a paw-like hand. As a result of the shortening of the phalanges, the excess of overlying skin and soft tissue collapses and becomes transversely folded and telescope into one another. Hence, the following etymology has developed: "la main en lorgnette of Marie and Léri," "opera glass hand," "telescoping fingers," "concertina hand," and "accordion hand" deformity.34) The differential diagnosis for arthritis mutilans include: psoriatic arthritis, rheumatoid arthritis, systemic lupus erythematosus, systemic sclerosis, juvenile idiopathic arthritis, cutaneous T cell lymphoma and idiopathic arthritis mutilans.5) The clinical course of MRH is classic. Characteristically, after a rapid initial progression followed by waxing and waning, the marked inflammation of the joints gradually abates and generally becomes inactive. Following this, hypertrophic changes ensue in the damaged joints.
Apart from dermatological and arthropathic manifestations, MRH can also be associated with fever, weight loss and weakness. Cardiac, pulmonary and hepatic involvement is rare. In 25% of cases, MRH is associated with malignancies of the skin, breast, gastrointestinal tract, genitourinary tract, leukemias and lymphomas. Other associations of MRH include diabetes, hypothyroidism, pregnancy and rheumatoid disorders.6)
Diagnosis of MRH solely depends upon a histopathological and immunohistochemical evaluation. Histopathological features include histiocytes and characteristic histiocytic multinucleated foreign body-type giant cells with a finely granulated, ground-glass eosinophilic cytoplasm, which is periodic acid-Schiff-reactive and diastase-resistant. Immunohistochemistry shows positive staining with CD4, CD45, CD68, human leukocyte antigen DR (HLA-DR), lysozyme, and alpha-1-antitrypsin and negative staining for CD20, S100, and factor XIIIa.7)
The hip joints are involved in 61% of the cases.2) Symptomatic involvement of the hip joint occurred many years after the cutaneous lesions of MRH in our patient. There is no established treatment protocol for the medical management of MRH. Variable therapeutic success has been achieved with a combination of non-steroidal anti-inflammatory agents, steroids, chemotherapeutic drugs, immuno-modulators like tumour necrosis factor-alpha inhibitors and bisphosphonates, especially alendronate during the active stage of the disease.89) The aftermath of MRH arthropathy lead to a significant disability in our patient due to involvement of the bilateral hands and hips. Successful THA offered significant relief from pain and disability. During arthroplasty, the points of concern were osteopenia and acetabular bone defects. To address the issue of compromised bone quality, cemented THA was performed. The acetabular wall defects were reconstructed with a morselised autograft harvested from the patient's osteotomised femoral head and neck. Additionally, we had to use a stainless steel mesh on one side for containment. Therefore, before proceeding to THA in any patient with MRH, the surgeon must be well equipped with allografts and the armamentarium required for acetabular reconstruction including mesh, ring (Muller) and cage (Burschneider or Octopus). Since the patient was reluctant to undergo any surgical treatment for arthritis mutilans, we did not intervene. Otherwise, arthrodesis of the small joints of the hand can be considered a valuable option.10)
A high degree of suspicion is essential for the diagnosis of MRH, which has a myriad of clinico-radiological symptoms. A meticulous histopathological evaluation is the key to making an accurate diagnosis. Bilateral hip arthropathy secondary to MRH can be successfully managed with THA. Osteopenia and acetabular defects should be anticipated in all cases during arthroplasty.
Figures and Tables
Fig. 2
Skin lesions. Multiple violaceous nodules (black arrows) over the back (A) and abdomen (B). (C) Coalescent pinkish macules over the nape of the neck. (D) Multiple confluent skin-colored papules over the back of the forearm (cobblestone appearance).

Fig. 3
Preoperative radiograph of the pelvis with the bilateral hip showing secondary osteoarthritis.

Fig. 4
(A) Radiograph of the lumbar spine showing pathological collapse of L1 and L2 vertebrae. (B) Radiograph of bilateral hands showing arthritis mutilans with "pencil-in-a-cup" appearance.

Fig. 5
Intraoperative images. (A) Defect in acetabulum (black star). (B) Osteotomized section of pathological head and neck of femur. (C) Autograft prepared from the femoral head and neck. (D) Reconstruction of the acetabulum with autograft and mesh.

Fig. 7
Histopathological photomicrograph. (A) Sheets of multinucleated giant cells with eosinophilic, ground glass cytoplasm (black arrows). Star mark indicates bony spicule being engulfed by the multinucleated giant cell. (H&E, ×200). (B) Mononuclear epithelioid cells with ground glass eosinophilic cytoplasm, histiocytes and mixed inflammatory cells in the background (H&E, ×400).
References
1. Santilli D, Lo Monaco A, Cavazzini PL, Trotta F. Multicentric reticulohistiocytosis: a rare cause of erosive arthropathy of the distal interphalangeal finger joints. Ann Rheum Dis. 2002; 61(6):485–487.

2. Barrow MV, Holubar K. Multicentric reticulohistiocytosis: a review of 33 patients. Medicine (Baltimore). 1969; 48(4):287–305.
3. Nelson LS. The opera-glass hand in chronic arthritis: "la main en lorgnette" of Marie and Leri. J Bone Joint Surg Am. 1938; 20(4):1045–1049.
4. Solomon WM, Stecher RM. Chronic absorptive arthritis or opera-glass hand: report of eight cases. Ann Rheum Dis. 1950; 9(3):209–220.

6. Campbell DA, Edwards NL. Multicentric reticulohistiocytosis: systemic macrophage disorder. Baillieres Clin Rheumatol. 1991; 5(2):301–319.

7. Gorman JD, Danning C, Schumacher HR, Klippel JH, Davis JC Jr. Multicentric reticulohistiocytosis: case report with immunohistochemical analysis and literature review. Arthritis Rheum. 2000; 43(4):930–938.

8. Goto H, Inaba M, Kobayashi K, et al. Successful treatment of multicentric reticulohistiocytosis with alendronate: evidence for a direct effect of bisphosphonate on histiocytes. Arthritis Rheum. 2003; 48(12):3538–3541.





 PDF
PDF ePub
ePub Citation
Citation Print
Print




 XML Download
XML Download