Abstract
Background
Standard treatments may provide adequate containment in mild to moderate Legg-Calve-Perthes disease (LCPD), but they can be problematic in more severe cases. The purpose of this study was to report the results of combined shelf acetabuloplasty with femoral varus osteotomy in severe LCPD.
Methods
We reviewed 12 patients who had undergone combined shelf acetabuloplasty with femoral varus osteotomy. The indications for this type of operation were: (1) above 8 years of age at clinical onset; (2) massive femoral epiphysis involvement (Catterall group 4, lateral pillar C); (3) femoral head lateral subluxation on the anteroposterior radiograph; and (4) impending hinged abduction on preoperative magnetic resonance imaging or arthrography. The mean age was 9.3 years (range, 8 to 10.8 years). The patients were clinically evaluated with Iowa hip score and leg length discrepancy at the final follow-up. Radiographic outcome was assessed using the Stulberg classification to evaluate femoral head sphericity. The presence of osteoarthritis was evaluated by the Tonnis classification. Correlation analysis was conducted to analyze the preoperative factors that were strongly associated with patients' outcomes.
Results
The mean follow-up period was 10.1 years (range, 7.1 to 13.2 years). Functional grade was excellent in all patients at last follow-up (mean, 92; range, 82 to 99). The mean leg length discrepancy after skeletal maturity was 0.9 cm (range, 0 to 1.7 cm). There were no significant complications or need for additional surgery. Radiographically, 92% of patients reached satisfactory outcomes: Stulberg grade I, 0 cases; Stulberg grade II, 4 cases (34%); Stulberg III, 7 cases (58%), Stulberg IV, 1 case (8%); and Stulberg V, 0 cases. There was no osteoarthritis by Tonnis classification.
Conclusions
The surgical outcomes for combined shelf acetabuloplasty with femoral varus osteotomy in severe LCPD patients over 8 years old are comparable with other advanced surgical methods. In the cases of severe disease that match our inclusion criteria, our containment method could be another treatment option.
Surgical containment has become widely accepted as the best method for treating Legg-Calve-Perthes disease (LCPD).12) Containment treatment is designed to center the femoral head within the acetabulum during the period of "biologic plasticity." This allows the acetabulum to serve as a mold during the healing process.34) The most common methods for surgical containment have been either proximal femoral varus osteotomy5) or Salter innominate osteotomy.6) Either of these methods may provide adequate containment in mild to moderate LCPD, but they can be problematic in more severe cases.
LCPD in over 8-year-old children that is concomitant with massive femoral head involvement and femoral head lateral subluxation could be called severe. Even when patients were classed as early stage by the Waldenstrom classification,7) the results of conventional containment methods in severe disease were not good.8) Full coverage of the enlarged femoral head and correction of subluxation by conventional techniques may be difficult to achieve in severe disease cases.910) For these, a number of advanced treatment methods are being attempted, but as yet, there are no clear standard guidelines.
We performed simultaneous combined proximal femoral varus osteotomy and shelf acetabuloplasty as a means of surgical containment for severe older aged LCPD patients. We assumed that we could not achieve full coverage of the enlarged femoral head solely by femoral varization. In cases of coxa magna with massive femoral head involvement, although the contact surface between the head and the acetabulum is changed through femoral varus osteotomy, iatrogenic hinged abduction could be induced in newly formed contact surfaces.
The purpose of this study was to report the result of combined shelf acetabuloplasty with femoral varus osteotomy in severe LCPD and to recommend another treatment option for proper containment in severe cases.
We retrospectively reviewed 12 pediatric hips with LCPD that had been treated by combined femoral varus osteotomy and shelf acetabuloplasty at Samsung Medical Center from 1997 to 2005. The indication for this type of operation was severe LCPD before Waldenstrom reossification stage, specifically: (1) above 8 years of age at clinical onset; (2) massive femoral epiphysis involvement (Catterall group 4, lateral pillar C); (3) femoral head subluxation on the anteroposterior radiograph; and (4) impending hinged abduction on preoperative magnetic resonance imaging (MRI) or arthrography. "Impending hinged abduction" is defined as when the femoral head forms a lateral hump and the labrum tip migrates upward in the neutral position (Fig. 1A and B) but the femoral head is reducible by hip abduction (Fig. 1C). We excluded: (1) Waldenstrom late stages and (2) definite hinged abduction (nonreducible hip). There were 17 severe LCPD patients who met these inclusion criteria. We included 12 hips of 12 patients (9 males, 3 females) who had reached skeletal maturity at regular follow-up. One patient showed unsynchronous bilateral involvement, although the other side was treated with nonsurgical methods. Mean age at diagnosis was 9.3 years (range, 8 to 10.8 years), and mean age at surgery was 9.5 years (range, 8.1 to 10.9 years).
Preoperatively, seven patients who showed abduction limitations underwent a diagnostic arthrogram, an adductor tenotomy and 6 weeks of Petrie cast. The other five patients underwent MRI and 2 weeks of skin traction before the definite surgery. The range of motion of the hip joint under general anesthesia was full in all patients. Intraoperative dynamic arthrography was performed in all hips to determine the degree of varization and derotation. A double incision was used for this type of surgery. Proximal femoral osteotomy for varization and derotation was performed at the intertrochanteric level. Intraoperatively, neck-shaft angles were never reduced to less than 110°, and the derotation angle was less than 20°.11) Internal fixation of the proximal femur was conducted by using the right-angled blade plate, and, subsequently, shelf acetabuloplasty was performed using the Smith-Peterson anterior approach. The surgical technique was the same as that described by Staheli.12) The length and position of the slot were determined intraoperatively by the need for coverage. After the proximal femoral osteotomy, if more anterior coverage was required, the slot was extended anteriorly (Fig. 1D). Postoperatively, a single hip spica cast was applied for 6 weeks. When the cast was removed, the patient was allowed crutch-assisted walking and gentle range of motion of the hip for an additional 6 to 8 weeks; then, full weight bearing without support was allowed. No subsequent abduction brace was used in any cases.
All preoperative radiographs were accessed with the Waldenstrom classification,7) the Catterall classification,13) and the Herring lateral pillar classification14) at the time of operation. Preoperative radiographic measurements of lateral subluxation were performed using the epiphyseal extrusion index.15) The number of "head at risk" signs was counted. To evaluate the clinical outcomes in this group of patients, we administered the Iowa hip score,16) which considers function, pain, gait, absence of deformity, muscle strength, and the Trendelenburg sign. Leg length discrepancy was evaluated by whole leg plain radiograph (Scanogram) at regular follow-up. Complications associated with surgery were retrieved from electronic medical records. The final, plain follow-up radiographs of the hip joint were assessed by Stulberg classification17) to evaluate the radiological outcomes. Cases of spherical femoral head (Stulberg I or II) were rated as good, ovoid femoral head (Stulberg III) was rated as fair and flat femoral head (Stulberg IV or V) was rated as bad. The presence of osteoarthritis was evaluated using the Tonnis classification.18) The differences in the articulotrochanter distance at the latest follow-up were measured to evaluate the degree of greater trochanter overgrowth. Final follow-up radiographic evaluations were performed by two independent pediatric orthopedic surgeons who were not involved in the patients' initial care. These two observers reached consensus in cases of different opinions.
Statistical analyses were performed with IBM SPSS ver. 19.0 (IBM Co., Armonk, NY, USA), and p-values less than 0.05 were considered statistically significant. The Shapiro-Wilk test was used to assess normality. Spearman correlation analysis was conducted to analyze the preoperative factors that were strongly associated with patient outcomes. Age at diagnosis, number of "head at risk" signs, and degree of lateral subluxation were used as preoperative factors. Iowa hip score and the Stulberg classification were used to determine patient outcomes. Another statistical analysis using the Spearman correlation test was conducted to evaluate whether the degree of femoral varization and stage of femoral epiphysis involvement were associated with leg length discrepancy.
The mean follow-up period after the surgery was 10.1 years (range, 7.1 to 13.2 years). At the time of surgery, all hips were at the Waldenstrom fragmentation stage, Catterall 4, and lateral pillar C. The average preoperative epiphyseal extrusion index was 38.7% (range, 26% to 55%). The mean number of "head at risk" signs was 3.25 (range, 2 to 5) (Table 1).
Functional outcomes measured by the Iowa hip score were excellent in all patients (mean score, 92; range, 82 to 99). Most of the subtraction points in the Iowa score were attributable to leg length discrepancy, and in fact, no patients had pain or functional problems in daily living. Leg length discrepancy was found in 10 patients (83%) in whole leg plain radiographs during regular follow-up. Three patients (25%) had symptoms of leg length discrepancy more than 2 cm and were treated with contralateral distal femur epiphysiodesis. Seven cases (58%) were treated nonoperatively because there were no clinical symptoms. The mean leg length discrepancy after skeletal maturity was 0.9 cm (range, 0 to 1.7 cm). The mean difference in articulotrochanter distance at the latest follow-up was 14.3 mm (range, 1.9 to 30.9 mm). No patient had a limping gait or Trendelenburg sign at final follow-up. There were no significant complications or need for additional surgery.
At the latest follow-up, radiographic outcomes were assessed using the Stulberg classification: Stulberg grade I, 0 cases; Stulberg grade II, 4 cases (34%); Stulberg III, 7 cases (58%); Stulberg IV, 1 case (8%); and Stulberg V, 0 cases. In brief, four hips (34%) were classified as having good sphericity, seven (58%) were classified as having fair sphericity and one (8%) was classified as having bad sphericity. There was no osteoarthritis by Tonnis classification (Fig. 1E).
In the statistical analysis of the factors that affected outcomes, preoperative factors such as age and degree of femoral head lateral subluxation showed no statistically significant correlations with the results. However, there was a statistically significant correlation in the number of "head at risk" signs with the Iowa hip score (p = 0.04); the more the number of "head at risk" signs, the lower the Iowa hip score (correlation coefficient, -0.594). In the statistical analysis of leg length discrepancy, there was no statistically significant correlation between leg length discrepancy and intraoperative neck shaft angle or severity of femoral head deformation at last follow-up.
We performed combined femoral varus osteotomy and shelf acetabuloplasty as a means of surgical containment for severe older aged LCPD patients. In every case, there was massive femoral head involvement accompanying lateral subluxation of the femoral head. The labrum, which had migrated upward in the neutral position, became reduced by the hip joint varus position on intraoperative arthrography. However, additional lateral coverage was needed because of the lateral extrusion of the enlarged femoral head. We added shelf acetabuloplasty to improve coverage of the femoral head without increasing intraarticular pressure. All patients had good clinical outcomes according to the Iowa hip scoring system. Radiographically, 92% of patients reached satisfactory outcomes when we consider satisfactory outcomes as "fair" or "good." Although the disease extent and lateral subluxation of the femoral head in this series were more severe than those of other studies, the results did not differ from other studies that used other advanced surgical techniques (Table 2).192021222324)
The multicenter study of Herring et al.25) found that LCPD in over 8-year-old children, concomitant with massive femoral head involvement and femoral head lateral subluxation, fared less well in response to various therapeutic approaches. An advanced surgical technique was developed for obtaining sufficient lateral coverage and proper containment in these severe LCPD cases. However, there is still controversy concerning the treatment of severe LCPD. The choice of surgery depends on the surgeon's preference or experience. Advanced containment methods have been used for severe disease including: Salter innominate osteotomy combined with a proximal femoral varus osteotomy,192226) triple pelvic osteotomy,232728) and shelf acetabuloplasty.
Olney and Asher26) used Salter innominate osteotomy combined with a proximal femoral varus osteotomy for nine cases of Catterall groups III and IV in patients with an average age of 8 years at the onset of disease. The average epiphyseal extrusion index was 26%. The mean duration of follow-up was 4.2 years. Olney and Asher26) reported radiographic results that 4 (44%) were good, 4 (44%) were fair, and 1 (12%) was poor. Crutcher and Staheli19) performed combined Salter and varus femoral osteotomies in 14 patients with severe disease. The average preoperative epiphyseal index was 30%. Mean duration of follow-up was 8 years. Seven hips (50%) showed spherical congruency on follow-up plain radiography. However, Salter osteotomy has limited effects on acetabular rotation (generally, anterior, 20° to 30°; lateral, 10° to 15°);29) even if femoral varus osteotomy is performed, it is difficult to contain an enlarged and laterally subluxed femoral head. Especially in a child over 8 years old, who will have a less flexible symphysis pubis, the rotation of the acetabulum is suboptimal. Excessive handling of acetabular rotation might increase local pressure on a weakened femoral head's lateral edge.
Poul and Vejrostova28) evaluated the use of the Steel triple osteotomy in severe LCPD. They noted successful containment with subsequent remodeling, even in deformed femoral heads, in 11 of the 12 cases. Wenger et al.23) performed triple pelvic osteotomy on 40 hips at lateral pillar B or C. The follow-up period was 3 to 9 years. The authors reported that 42% had good outcomes (Stulberg I/II), 47% had fair outcomes (Stulberg III), and 11% had poor outcomes. However, the surgical technique of triple osteotomy is somewhat difficult to perform, making it difficult for inexperienced surgeons to achieve uniform surgical outcomes. We believed that a uniform and easily reproducible method of assessing the disease should help elucidate the long-term disease prognosis. Additionally, the long-term results of triple osteotomy were not yet available.
Recently, good results from shelf acetabuloplasty have been reported as a containment treatment of severe LCPD in older children. Kruse et al.30) reported good long-term results in patients with hinge abduction that was treated with shelf arthroplasty. After a mean 19 years of follow-up, two hips rated as Stulberg class II, seven as Stulberg III, five as Stulberg IV and one as Stulberg V. Freeman et al.,31) in a study of shelf arthroplasty that was limited to patients who had hinge abduction, documented excellent results, with one patient rated as Stulberg I, 13 as Stulberg II, 10 as Stulberg III, two as Stulberg IV and one as Stulberg V. Furthermore, we performed shelf acetabuloplasty as a means of containment treatment for severe LCPD in older children. However, we have a slightly different indication for the two types of surgeries. The particular indication of this type of surgery was "impending hinged abduction." In this condition, we thought that hip joint containment would not be improved by only shelf acetabuloplasty. Ghanem et al.,32) in study of shelf acetabuloplasty for severe LCPD patients, documented that combined femoral varus osteotomy was needed in the more severe cases, 15 of the 30 hips. They reported that this combined procedure might have had a positive effect on the overall surgical result.
We described "impending hinged abduction" in the inclusion criteria. All hips showed lateral hump formation of the femoral head and upward migration of the labrum tip. However, all of these condition do not indicate fixed hinge abduction. If the hip joint is reducible before the remodeling stage, the deformation of the hip joint is reversible. The reduced femoral hump within the acetabulum during the period of "biologic plasticity" restores its own sphericity. Choi et al.33) described this as "reducible hinged abduction." They stated that containment treatment can be used in reducible hinged abduction. The reducibility of the subluxated femoral head was determined by dynamic arthrography.3435) Domzalski et al.36) stated that containment treatment was contraindicated in non-reducible hip in dynamic arthrography, which occurs when the labrum tip moves upwards on attempted abduction. Yoo et al.35) categorized the types of labrum in hip abduction as "comfortable" or "uncomfortable." They asserted that a comfortable labrum in hip abduction implies that the lateral part of the cartilaginous femoral head is relatively congruent and does not place pressure on the lateral edge of the acetabulum. We also performed intraoperative dynamic arthrography to exclude non-reducible hips, and we confirmed the reduction of the femoral head by the hip abduction.
Correlation analysis between the preoperative degree of femoral head lateral displacement and the final follow-up results did not show statistically significant results. This might mean that the degree of femoral head lateral subluxation had no effect on the results because all hip joints had sufficient acetabular coverage by shelf procedure. Generally, the leg lengths can roughly 1 cm shorter when femoral varus osteotomy is performed. We supposed that if the degree of varus angulation was severe, final leg length could be short. We performed correlation analysis of intraoperative neck shaft angle and leg length discrepancy and found no association. We further supposed that if femoral head deformation was more severe, the leg length could be shorter. Stulberg classification and leg length discrepancy at the final follow-up were not associated. This result suggests that severity of femoral head deformation or degree of intraoperative varus angulation is not a key factor in leg length discrepancy. The factors that affect leg length discrepancy may be more complex.
Our study has some obvious limitations, mainly the small number of patients and the lack of a control group. Additionally, this study has limited value for femoroacetabular impingement. Therefore, our findings must be interpreted cautiously. However, our study has some worth in that it is the first report of the same surgical technique and the surgical outcome of a homogenous group with defined preoperative inclusion criteria. There were no clearly defined inclusion criteria in most studies about the advanced surgical method for severe LCPD. The mean follow-up periods were relatively short compared with other long-term result reports about LCPD surgical treatment. Long-term follow-up to old age is required, but all patients had reached skeletal maturity at the final follow-up. The degree of femoral head deformation at skeletal maturity may reflect the hip joint state of middle-aged adults.
In conclusion, the surgical outcomes of combined shelf acetabuloplasty with femoral varus osteotomy for severe LCPD patients over 8 years old are comparable with other advanced surgical methods. In cases of severe disease, such as among those patients who matched our inclusion criteria and had collapsed femoral heads that lacked lateral coverage even after varization and that could pivot on the lateral edge of the acetabulum, our containment method could be an another treatment option.
Figures and Tables
Fig. 1
A 9.8-year-old boy with severe Legg-Calve-Perthes disease. (A) Preoperative plain radiograph and magnetic resonance imaging show marked lateral extrusion and extensive collapse of the femoral head. (B) Arthrogram of the patient shows upward migration (arrowhead) of labrum tip due to lateral hump formation of subluxed femoral head. (C) Dynamic arthrogram of the patient shows reduction of femoral head by hip joint abduction, however lateral coverage of enlarged femoral head is insufficient. (D) We performed simultaneous combined proximal femoral varus osteotomy and shelf acetabuloplasty as a means of surgical containment for this patient. (E) Radiograph at 10 years after surgery shows a femoral head that, although not spherical, is congruent and well contained.
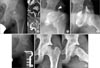
Table 1
Patients' Details
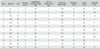
Table 2
Radiographic Results at Follow-up According to Treatment Methods for Severe Legg-Calve-Perthes Disease

| Source | Mean age (yr) | Catterall | Herring | Treatment method | Satisfactory results on radiograph* (%) |
|---|---|---|---|---|---|
| Crutcher and Staheli19) | 8.4 | 4 or 3 | - | Combined Salter and femoral varus osteotomy | 93 |
| Ishida et al.20) | 7.1 | 4 or 3 | - | Salter osteotomy | 78 |
| Aksoy et al.21) | 8.3 | - | C | Varus femoral osteotomy | 77 |
| Javid and Wedge22) | 9.7 | - | C or B/C | Combined Salter and femoral varus osteotomy | 67 |
| Wenger et al.23) | 7.7 | - | C | Triple pelvic osteotomy | 75 |
| Terjesen et al.24) | 7.4 | - | C | Varus femoral osteotomy | 79 |
| Current study | 9.3 | 4 | C | Combined shelf and femoral varus osteotomy | 92 |
References
1. Nguyen NA, Klein G, Dogbey G, McCourt JB, Mehlman CT. Operative versus nonoperative treatments for Legg-Calve-Perthes disease: a meta-analysis. J Pediatr Orthop. 2012; 32(7):697–705.
2. Wiig O, Terjesen T, Svenningsen S. Prognostic factors and outcome of treatment in Perthes' disease: a prospective study of 368 patients with five-year follow-up. J Bone Joint Surg Br. 2008; 90(10):1364–1371.
3. Grzegorzewski A, Synder M, Kozlowski P, Szymczak W, Bowen RJ. The role of the acetabulum in Perthes disease. J Pediatr Orthop. 2006; 26(3):316–321.

4. Kim HK, Herring JA. Pathophysiology, classifications, and natural history of Perthes disease. Orthop Clin North Am. 2011; 42(3):285–295.

5. Beer Y, Smorgick Y, Oron A, et al. Long-term results of proximal femoral osteotomy in Legg-Calve-Perthes disease. J Pediatr Orthop. 2008; 28(8):819–824.

6. Thompson GH. Salter osteotomy in Legg-Calve-Perthes disease. J Pediatr Orthop. 2011; 31:2 Suppl. S192–S197.
8. Rab GT. Theoretical study of subluxation in early Legg-Calve-Perthes disease. J Pediatr Orthop. 2005; 25(6):728–733.
9. Chang JH, Kuo KN, Huang SC. Outcomes in advanced Legg-Calve-Perthes disease treated with the Staheli procedure. J Surg Res. 2011; 168(2):237–242.

10. Wenger DR, Pandya NK. Advanced containment methods for the treatment of Perthes disease: Salter plus varus osteotomy and triple pelvic osteotomy. J Pediatr Orthop. 2011; 31:2 Suppl. S198–S205.
11. Kim HK, da Cunha AM, Browne R, Kim HT, Herring JA. How much varus is optimal with proximal femoral osteotomy to preserve the femoral head in Legg-Calve-Perthes disease. J Bone Joint Surg Am. 2011; 93(4):341–347.

13. Catterall A. Natural history, classification, and x-ray signs in Legg-Calve-Perthes' disease. Acta Orthop Belg. 1980; 46(4):346–351.
14. Herring JA, Kim HT, Browne R. Legg-Calve-Perthes disease. Part I: classification of radiographs with use of the modified lateral pillar and Stulberg classifications. J Bone Joint Surg Am. 2004; 86(10):2103–2120.
15. Green NE, Beauchamp RD, Griffin PP. Epiphyseal extrusion as a prognostic index in Legg-Calve-Perthes disease. J Bone Joint Surg Am. 1981; 63(6):900–905.
17. Stulberg SD, Cooperman DR, Wallensten R. The natural history of Legg-Calve-Perthes disease. J Bone Joint Surg Am. 1981; 63(7):1095–1108.
18. Tonnis D. Congenital dysplasia and dislocation of the hip in children and adults. Berlin, Germany: Springer-Verlag;1987. p. 167.
19. Crutcher JP, Staheli LT. Combined osteotomy as a salvage procedure for severe Legg-Calve-Perthes disease. J Pediatr Orthop. 1992; 12(2):151–156.

20. Ishida A, Kuwajima SS, Laredo Filho J, Milani C. Salter innominate osteotomy in the treatment of severe Legg-Calve-Perthes disease: clinical and radiographic results in 32 patients (37 hips) at skeletal maturity. J Pediatr Orthop. 2004; 24(3):257–264.

21. Aksoy MC, Cankus MC, Alanay A, Yazici M, Caglar O, Alpaslan AM. Radiological outcome of proximal femoral varus osteotomy for the treatment of lateral pillar group-C Legg-Calve-Perthes disease. J Pediatr Orthop B. 2005; 14(2):88–91.
22. Javid M, Wedge JH. Radiographic results of combined Salter innominate and femoral osteotomy in Legg-Calve-Perthes disease in older children. J Child Orthop. 2009; 3(3):229–234.

23. Wenger DR, Pring ME, Hosalkar HS, Caltoum CB, Lalonde FD, Bastrom TP. Advanced containment methods for Legg-Calve-Perthes disease: results of triple pelvic osteotomy. J Pediatr Orthop. 2010; 30(8):749–757.
24. Terjesen T, Wiig O, Svenningsen S. Varus femoral osteotomy improves sphericity of the femoral head in older children with severe form of Legg-Calve-Perthes disease. Clin Orthop Relat Res. 2012; 470(9):2394–2401.

25. Herring JA, Kim HT, Browne R. Legg-Calve-Perthes disease. Part II: prospective multicenter study of the effect of treatment on outcome. J Bone Joint Surg Am. 2004; 86(10):2121–2134.
26. Olney BW, Asher MA. Combined innominate and femoral osteotomy for the treatment of severe Legg-Calve-Perthes disease. J Pediatr Orthop. 1985; 5(6):645–651.

27. Vukasinovic Z, Spasovski D, Vucetic C, Cobeljic G, Zivkovic Z, Matanovic D. Triple pelvic osteotomy in the treatment of Legg-Calve-Perthes disease. Int Orthop. 2009; 33(5):1377–1383.

28. Poul J, Vejrostova M. Triple osteotomy of the pelvis in children and adolescents. Acta Chir Orthop Traumatol Cech. 2001; 68(2):93–98.
29. Salter RB. Innominate osteotomy in the treatment of congenital dislocation and subluxation of the hip. J Bone Joint Surg Br. 1961; 43(3):518–539.

30. Kruse RW, Guille JT, Bowen JR. Shelf arthroplasty in patients who have Legg-Calve-Perthes disease: a study of long-term results. J Bone Joint Surg Am. 1991; 73(9):1338–1347.

31. Freeman RT, Wainwright AM, Theologis TN, Benson MK. The outcome of patients with hinge abduction in severe Perthes disease treated by shelf acetabuloplasty. J Pediatr Orthop. 2008; 28(6):619–625.

32. Ghanem I, Haddad E, Haidar R, et al. Lateral shelf acetabuloplasty in the treatment of Legg-Calve-Perthes disease: improving mid-term outcome in severely deformed hips. J Child Orthop. 2010; 4(1):13–20.

33. Choi IH, Yoo WJ, Cho TJ, Moon HJ. Principles of treatment in late stages of Perthes disease. Orthop Clin North Am. 2011; 42(3):341–348.

34. Daly K, Bruce C, Catterall A. Lateral shelf acetabuloplasty in Perthes' disease: a review of the end of growth. J Bone Joint Surg Br. 1999; 81(3):380–384.
35. Yoo WJ, Choi IH, Cho TJ, Chung CY, Shin YW, Shin SJ. Shelf acetabuloplasty for children with Perthes' disease and reducible subluxation of the hip: prognostic factors related to hip remodelling. J Bone Joint Surg Br. 2009; 91(10):1383–1387.




 PDF
PDF ePub
ePub Citation
Citation Print
Print


 XML Download
XML Download