Abstract
Various types of tumor can occur in the subungual space, including glomus tumors, subungual exostosis, hemangioma, epidermal cysts, and malignant tumors. While fibromatosis can occur at various sites throughout the body, it is very rarely seen in the toe. Here, we are the first to report a case of superficial fibromatosis mimicking a glomus tumor in the subungual space of the second toe. The presentation of this condition shows the possibility of encountering uncommon superficial fibromatosis in the distal phalanx of the toe, and suggests that superficial fibromatosis should be included in the differential diagnosis of a glomus tumor in the toe.
Fibromatosis is a rare tumor caused by the proliferation of well-differentiated fibroblasts whose biological behavior is between that of a benign fibroblastic lesion and fibrosarcoma. Two-thirds of all fibromatosis occurs in the abdomen. Extra-abdominal fibromatosis occurs most frequently in the head, neck, chest wall, shoulder, back and thigh;1) however, superficial fibromatosis in the toe is extremely rare. Here, we report the first case of superficial fibromatosis of the second toe mimicking a glomus tumor. Complete marginal excision and histopathological examination is needed for the differential diagnosis of a glomus tumor.
A 36-year-old, otherwise healthy male, presented with recurrent pain of the left second toe. This started with walking several years earlier. His symptoms included pain over the region of the left second nail bed. There was no history of the trauma or infection. The patient did not exhibit increased temperature sensitivity in the painful region.
Physical examination revealed point tenderness at the nail of the left second toe, with no evidence of deformity or discoloration of the nail. Range of motion of the second toe was intact. Radiographs of the left foot demonstrated a focal osteolytic lesion with a subtle sclerotic margin in the distal phalanx of second toe (Fig. 1). A diagnostic inspection through magnetic resonance imaging (MRI) focused on the presence of a 0.7 × 0.6 × 0.5 cm well-marginated osteolytic lesion, with a low signal rim on all pulse sequences (Fig. 2). We originally diagnosed a subungual glomus tumor.
Surgery was performed in the supine position under spinal anesthesia with a thigh tourniquet, removing the nail from its bed to access the tumor, and a subsequent longitudinal incision was performed directly to the nail bed. A non-encapsulated, grey-white, rubbery mass was isolated with 2.5 loupe magnification (Fig. 3). It was totally marginally excised using a curette, along with the involved bone. The postoperative wound was closed and the removed nail was reattached to protect the nail bed (Fig. 4). The patient was supplied with a postoperative shoe during the wound healing period. Four weeks postoperatively, the patient was able to ambulate without symptoms. At the 1-year follow-up appointment, his symptoms had completely resolved and there was no sign of local recurrence.
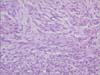
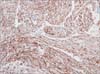
Histopathological examination revealed a typical fibromatosis. Hematoxylin and eosin-stained sections showed poorly circumscribed mass with infiltration of the surrounding adipose tissue, which consisted of cellular proliferation arranged into long fascicles (Fig. 5). The tumor cells were elongated, slender, spindled cells of uniform appearance (Fig. 6). Immunohistochemically, the tumor cells were positive for vimentin (Fig. 7).
Glomus tumors are uncommon, and thought to represent less than 1.5% of all benign soft tissue tumors of the extremities.2) Due to the fact that they appearance in the extremities is rare, their diagnosis is commonly delayed or missed. Radiographically, these tumors appear as well-circumscribed radiolucent lesions, with endosteal erosion of the adjacent cortex or sclerosis of adjacent bone. The radiographic appearance resembles that of an enchondroma, epithelial inclusion cyst, or simple bone cyst.3) MRI can be particularly helpful in the detection of early lesions, which are often smaller and more difficult to diagnose definitively by physical examination.4) MRI features that are considered diagnostic for glomus tumors include intermediate or low-signal intensity on T1-weighted images, marked hyperintensity on T2-weighted images, and strong enhancement after the injection of gadolinium-based contrast material.5) The pathological appearance of the tumor is nests of glomus cells, which are small, uniform, rounded cells surrounding capillary sized vessels. The glomus cells show smooth muscle actin in immunohistochemical stains; however, desmin, CD34, and S-100 proteins are usually negative. Although glomus tumors are benign lesions, excision of the lesion with a sufficient margin of surrounding normal tissue not only confirms the differential diagnosis, but also results in adequate treatment.2)
Fibromatoses are rare lesions, accounting for 0.03% of all tumors.6) Fibromatoses are characterized by proliferation of well-differentiated fibroblasts, infiltrative growth (ill-defined outlines), presence of a variable amount of collagen in between the proliferating cells, lack of cytological features of malignancy and scanty or absent mitotic activity and aggressive clinical behavior (repeated local recurrences but lack of capacity to metastasize distantly).7) Fibromatoses are divided into two large subgroups based on their location, superficial and deep. Superficial fibromatoses are typically small, slow growing tumors, whereas deep fibromatosis are commonly large, faster growing and more aggressive tumors. Superficial fibromatosis includes palmar fibromatosis (Dupuytren disease), plantar fibromatosis (Ledderhose disease), juvenile aponeurotic fibroma, and infantile digital fibromatosis.8) One of the superficial fibromatoses, palmar fibromatosis is the most common, followed by plantar fibromatosis. Fibromatoses of the extremities are generally rare.9) To our knowledge, no reports of superficial fibromatosis at the toe phalanx exist in the literature. Radiographs are frequently normal in patients with palmar and plantar fibromatosis; nevertheless, occasional scalloping of the adjacent bone is seen in patients with juvenile aponeurotic fibroma.10) In the present case, a focal osteolytic lesion with a subtle sclerotic margin was found in the distal phalanx of second toe. These lesions may be difficult to detect and manage, as they have a tendency to infiltrate adjacent structures and reoccur locally. MRI is considered the primary imaging modality in fibromatosis, for the purposes of planning surgery, detecting postoperative local recurrence and evaluating disease progression in patients not treated with surgery.6) Signal characteristics have been shown to correlate with the cellularity of the lesion.8) Fibromatosis does not metastasize, although recurrence rates vary. Treatment is based on either excision of the mass or radiotherapy and chemotherapy if the condition is inoperable; however, wide excision is the most effective method.9) Using microscopy, the lesions contain spindle-shaped myofibroblastic cells, dense deposits of intracellular collagen fibers, variable amounts of extracellular myxoid matrix, and compressed and elongated vessels.7) The present case is distinguished from a glomus tumor by the tumor cytomorphology (H&E) and immunoreactivity, and smooth muscle actin is negative.
The presentation of this condition shows the possibility of encountering uncommon superficial fibromatosis in the distal phalanx of the toe, and suggests that superficial fibromatosis should be included in the differential diagnosis of a glomus tumor in the toe.
Figures and Tables
Fig. 1
Radiographs of the left foot showing the focal osteolytic lesion with a subtle sclerotic margin in the distal phalanx of second toe.

Fig. 2
Coronal T1-weighted (A), sagittal T2-weighted (B), and sagittal gadolinium-enhanced fat-saturated T1-weighted (C) magnetic resonance imaging scans of the left foot showing the approximate 0.7 × 0.6 × 0.5 cm well-marginated osteolytic lesion and low-signal rim with iso signal intensity on T1-weighted and high signal intensity on T2-weighted images compared to adjacent muscles, and homogeneous contrast enhancement in the distal phalanx of the second toe (arrowheads).

Fig. 4
Intraoperative photographs showing the nail bed longitudinal incision and reattachment of the removed nail as a nail bed protector.

References
1. Allen PJ, Shriver CD. Desmoid tumors of the chest wall. Semin Thorac Cardiovasc Surg. 1999; 11(3):264–269.

2. Pater TJ, Marks RM. Glomus tumor of the hallux: case presentation and review of the literature. Foot Ankle Int. 2004; 25(6):434–437.

3. Drape JL, Idy-Peretti I, Goettmann S, Guerin-Surville H, Bittoun J. Standard and high resolution magnetic resonance imaging of glomus tumors of toes and fingertips. J Am Acad Dermatol. 1996; 35(4):550–555.

4. Matloub HS, Muoneke VN, Prevel CD, Sanger JR, Yousif NJ. Glomus tumor imaging: use of MRI for localization of occult lesions. J Hand Surg Am. 1992; 17(3):472–475.

5. Baek HJ, Lee SJ, Cho KH, et al. Subungual tumors: clinicopathologic correlation with US and MR imaging findings. Radiographics. 2010; 30(6):1621–1636.

6. Guglielmi G, Cifaratti A, Scalzo G, Magarelli N. Imaging of superficial and deep fibromatosis. Radiol Med. 2009; 114(8):1292–1307.

7. Rosai J. Rosai and Ackerman's surgical pathology. 9th ed. Edinburgh: Mosby;2004.
8. Robbin MR, Murphey MD, Temple HT, Kransdorf MJ, Choi JJ. Imaging of musculoskeletal fibromatosis. Radiographics. 2001; 21(3):585–600.





 PDF
PDF ePub
ePub Citation
Citation Print
Print




 XML Download
XML Download