Abstract
Background
To evaluate risk factors of redisplacement and remind surgeons of key factors regarding conservative treatment of distal radius fracture.
Methods
A total of 132 patients who received conservative treatment for distal radius fractures between March 2008 and February 2011 were included in this study. Radial inclination, radial length, volar tilting angle, ulnar variance, fragment translation, and presence of dorsal metaphyseal comminution were measured on the X-rays taken immediately after reduction, one week after injury during the first follow-up outpatient clinic visit, and after the gain of radiological union. Secondary displacement was defined as a loss of reduction during the follow-up period, and was divided into 'early' and 'late' categories. We analyzed the influence of initial displacement radiologic variables, dorsal cortex comminution, and patient age on the development of secondary displacement.
Results
Development of secondary displacement was significantly associated only with initial displacement radiologic variables (p < 0.001), development of the late secondary displacement was significantly associated with age (p = 0.005), and initial displacement radiologic variables were associated significantly with a serial increase in ulnar variance (p = 0.003).
Conclusions
Greater displacement on the initial radiographs indicates a higher possibility of development for secondary displacement, and older patients had a higher probability of late secondary displacement development. Furthermore, dorsal comminutions did not affect secondary displacement directly.
Distal radius fractures are common, comprising 17% of fractures in the upper extremity.1) While undisplaced, stable distal radius fractures are usually well treated with conservative methods, surgical treatments are required for severely displaced, unstable distal radius fractures. However, unsatisfactory surgical outcomes have been reported in 9% to 32% of cases, depending on the type of fracture and degree of displacement.2345) Given the evidence to date, it is imperative to identify risk factors for redisplacement when choosing a conservative treatment for displaced distal radius fractures and to notify surgeons of key factors regarding conservative treatment for distal radius fractures. Various factors affect secondary displacement of fracture fragments after anatomic or near anatomic initial closed reduction. In particular, the presence of a dorsally comminuted subset of distal radius fractures presents a challenge, even for internal fixation.6) Cooney et al.7) suggested that fractures with severe dorsal comminution and dorsal angulation greater than 20° have a significant chance of redisplacement after reduction. Vaughan et al.8) emphasized the importance of dorsal angulation and radial shortening as factors for redisplacement.
Although many studies have evaluated risk factors of failure on a conservative treatment for distal radius fractures, there are still controversies regarding which factors are statistically significant.9101112) The purpose of our current study is to provide prognostic factors by evaluating the relationship between loss of initial closed reduction and the three most controversial risk factors (e.g., age, dorsal comminution, and degree of initial displacement) in patients who received conservative treatments for distal radius fractures. By analyzing the risk factors, surgeons may be able to better predict prognosis after successful primary reduction so that they can determine the treatment plan for each patient preemptively.
We enrolled patients in this study from a total cohort of 193 consecutive cases treated for distal radius fractures at our hospital between March 2008 and February 2011 and available for more than 6 months of follow-up. The exclusion criteria were patient age of less than 18 years, concomitant radial or ulna shaft fractures or intraarticular fractures, and any patient who had undergone an operation initially. A final group of 132 patients was included in our analysis.
In our study population, closed reduction and stabilization were performed with the use of a U-shape splint initially, and short arm casts were applied subsequently. Initial X-rays were evaluated for fracture type based on the AO classification. Anteroposterior and lateral X-rays of the wrist were taken at every visit in the outpatient clinic. We analyzed the immediate postreduction X-rays, those taken at the first follow-up visit (1 week after injury), and those taken after union (more than 8 weeks after injury). The radial inclination, radial length, volar tilting angle, ulnar variance, and presence of dorsal metaphyseal comminution were measured. In cases that received surgical treatment due to redisplacement during the follow-up period, the X-rays before surgery were analyzed. Dorsal metaphyseal comminution was determined by the presence of free-floating bone fragments at the dorsal cortex on the lateral radiographs according to Makhni's definition (Fig. 1).13) Radiographic parameters constituting 'acceptable alignment' were dorsal tilt less than 10°, volar tilt ranging from 5° to 25°, radial inclination not less than 17°, and fragment translation less than 2 mm (Table 1).31114)
We analyzed the initial displacement radiographic variables, the presence of dorsal cortex comminution, and patient age as factors related to secondary displacement. Minimally displaced fractures were defined as those with no initial radiographic displacement and able to be stabilized by the splint without forceful manipulative reduction. Displaced fractures were defined as those with higher values than the radiographic parameters described in Table 1 and for which forceful closed reduction was necessary. Secondary displacement was defined as loss of reduction during the follow-up period. Cases in which surgery was performed before union were also defined as secondary displacement. Secondary displacement was divided into early secondary displacement in which displacement developed before the first follow-up visit or a surgery was performed before 2 weeks post-injury, and late secondary displacement in which displacement developed after the first follow-up visit or a surgery was performed after 2 weeks post-injury. We also analyzed the effects of initial displacement degree, dorsal cortex comminution, and patient age on serial change of the radiologic measures.
Descriptive statistics were reported as means (and range) for continuous variables and as numbers (and percentage, if possible) for discrete assessments. Differences of the predictor variables between patients who eventually had secondary displacement and those who did not were statistically analyzed by means of t-tests for continuous variables and a chi-square test for categorical variables. The interval changes of radial inclination, radial length, volar tilt, and ulnar variance, and effects of age, initial displacement radiologic variables, and dorsal comminution were analyzed with the help of the general linear model. A multiple logistic regression analysis was used to analyze relationships between development of secondary displacement and predictor variables, such as age, degree of initial displacement, and dorsal cortical comminution. All statistical analyses were performed using PASW ver. 18.0 (SPSS Inc., Chicago, IL, USA), and p < 0.05 was considered statistically significant.
The 132-patient study cohort was comprised of 29 men and 103 women with a mean age of 58 years (range, 21 to 89 years). The mean follow-up period was 8.2 months (range, 6 to 17 months) and the mean duration of cast application was 6.2 weeks (range, 5 to 8 weeks). Based on the AO classification, the fracture types in this cohort were type A in 90 cases, type B in 33 cases, and type C in 9 cases.
Forty-five cases had minimally displaced fractures, and 87 cases had displaced fractures on initial X-rays. Metaphyseal comminution was found in 56 cases at the dorsal cortex and in 15 cases at the volar cortex. Secondary displacement was developed in 47 out of 132 cases (35.6%), in which early and late secondary displacements were found in 33 and 14 cases, respectively. Twenty-nine cases of early secondary displacement and three cases of late secondary displacement had undergone surgical treatment. Our results show that secondary displacement was significantly associated only with degree of initial displacement as compared with the non-displaced group (p < 0.001) (Table 2). Development of late secondary displacement was significantly associated only with age (p = 0.005) (Table 3).
Radial inclination, radial length, volar tilt, and ulnar variance were 21.8°, 11.5 mm, 11.1°, and 0.31 mm after reduction, 20.6°, 10.8 mm, 9.6°, and 0.70 mm at 1 week post-reduction, and 18.9°, 9.2 mm, 8.4°, and 1.7 mm at the last follow-up after union, respectively. The interval changes of radial inclination (p < 0.001), radial length (p < 0.001), volar tilt (p = 0.001), and ulnar variance (p < 0.001) were statistically significant (Table 4). Analysis of the effects of age, dorsal comminution, and initial displacement radiologic variables on each value showed that initial displacement was associated significantly with a serial increase in ulnar variance (p = 0.003) (Table 5). Serial changes in radial inclination, radial length, and volar tilt were not significantly affected by any of these predictive factors.
Surgery is increasingly becoming a good treatment option for distal radius fractures, however, a review of the literature reveals that whether an operation produces better long-term outcomes or not is a subject of debate.15) As an option to avoid this debate, conservative treatment should be considered initially for distal radius fractures. Therefore, it is important to identify risk factors for the development of secondary displacement when planning to start and maintain a conservative treatment for distal radius fractures. There have been many studies about factors affecting fracture instability. Hove et al.16) reported on a large cohort of 645 patients treated conservatively and concluded that volar tilting, radial length, and age are predictive of nonunion. Jenkins17) reported that the extent to which a chronic collapse of the radial angle and length occurred was determined solely by the initial deformity. These authors also reported that the absence of a radiographically visible comminution of the dorsal cortex offered stability against malunion. Makhni et al.18) described secondary displacement developed in 78% and loss of reduction in 89% of patients treated conservatively for distal radius fractures. They concluded that an age above 60 was predictive of an increase in loss of reduction.
Our current study found that the degree of initial displacement is the most important predictive factor for secondary displacement, and our results suggest that there is high possibility of loss of reduction in the late period in older patients. By analyzing the association of secondary displacement with patient age, initial displacement degree, and dorsal comminution, we found that only patient age was significantly associated with late secondary displacement compared to the non-displacement group (p = 0.005). Although we speculated that metaphyseal dorsal comminution had an association with a loss of reduction due to reduced cortical support, the degree of initial displacement was the only predictive factor that caused a serial decrease in ulnar variance. Metaphyseal dorsal comminution was not found to be a major factor in the occurrence of secondary displacement. A study conducted by Vatansever et al.19) reported similar findings. However, there have been studies performed on the relationship between the radiological values of distal radius fracture and its severity. 20) Therefore, dorsal comminution should be taken into account when treating patients conservatively by putting sugar tong splint with the wrist in volar flexion and ulnar deviation (Cotton-Loder position). However, stiffness in the digits and the potential risk for median nerve compression should be observed carefully.
In terms of the instability onset, our results showed that late secondary displacement was significantly associated with patient age. Makhni et al.18) reported that increases in age significantly raise the rate of redisplacement. Additionally, Kim et al.21) previously reported that a loss of reduction in radial angulation, volar tilting, and radial length occurred most commonly at two weeks after the initial injury when conservative treatment was performed. Jenkins17) reported that only 5% of the patients showed a loss of reduction during the first week, and according to a study by Foldhazy et al.,22) dorsal angulation occurred most commonly at 2 to 4 weeks after the initial reduction in older patients. In our present study, early secondary displacement was developed in 33 cases (25%) and late secondary displacement in 14 cases (11%). Early secondary displacement was more prevalent than late secondary displacement.
Greater displacement on initial radiographs may indicate a higher possibility of secondary displacement. And as patient age increases, the probability of late secondary displacement increases. Furthermore, dorsal comminutions did not affect secondary displacement directly, so conservative treatment can be considered for patients with dorsal comminution. As a result, older patients with severe initial displaced distal radius fractures require close observation or operative management.
Figures and Tables
Fig. 1
The lateral radiograph shows a free-floating fragment at dorsal metaphyseal cortex, indicating dorsal comminution.

Table 1

| Parameter | Acceptable value |
|---|---|
| Dorsal tilt (°) | < 10 |
| Volar tilt (°) | 15 ± 10 |
| Radial inclination (°) | ≥ 17 |
| Translation (mm) | < 2.0 |
Table 2
Factors Associated with Secondary Displacement on Logistic Regression Analysis

Table 3
Factors Associated with Late Secondary Displacement on Logistic Regression Analysis

Table 4
Serial Changes of Radiographic Parameters in Each Session
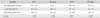
Table 5
Relationships between Predictive Factors Associated with Serial Changes of Radiographic Parameters and Factors Associated with Early and Late Secondary Displacement on General Linear Model Analysis

ACKNOWLEDGEMENTS
This work was supported by the Industrial Strategic Technology Development Program (10041605) funded by the Ministry of Trade, Industry and Energy (MOTIE, Korea).
References
1. Chung KC, Shauver MJ, Birkmeyer JD. Trends in the United States in the treatment of distal radial fractures in the elderly. J Bone Joint Surg Am. 2009; 91(8):1868–1873.

2. Young BT, Rayan GM. Outcome following nonoperative treatment of displaced distal radius fractures in low-demand patients older than 60 years. J Hand Surg Am. 2000; 25(1):19–28.

3. Melone CP Jr. Distal radius fractures: patterns of articular fragmentation. Orthop Clin North Am. 1993; 24(2):239–253.
4. Hove LM, Fjeldsgaard K, Skjeie R, Solheim E. Anatomical and functional results five years after remanipulated Colles' fractures. Scand J Plast Reconstr Surg Hand Surg. 1995; 29(4):349–355.

5. Villar RN, Marsh D, Rushton N, Greatorex RA. Three years after Colles' fracture: a prospective review. J Bone Joint Surg Br. 1987; 69(4):635–638.

6. Gondusky JS, Carney J, Erpenbach J, et al. Biomechanical comparison of locking versus nonlocking volar and dorsal T-plates for fixation of dorsally comminuted distal radius fractures. J Orthop Trauma. 2011; 25(1):44–50.

7. Cooney WP 3rd, Linscheid RL, Dobyns JH. External pin fixation for unstable Colles' fractures. J Bone Joint Surg Am. 1979; 61(6):840–845.

8. Vaughan PA, Lui SM, Harrington IJ, Maistrelli GL. Treatment of unstable fractures of the distal radius by external fixation. J Bone Joint Surg Br. 1985; 67(3):385–389.

9. Grewal R, MacDermid JC, King GJ, Faber KJ. Open reduction internal fixation versus percutaneous pinning with external fixation of distal radius fractures: a prospective, randomized clinical trial. J Hand Surg Am. 2011; 36(12):1899–1906.

10. Bales JG, Stern PJ. Treatment strategies of distal radius fractures. Hand Clin. 2012; 28(2):177–184.

11. Arora R, Lutz M, Deml C, Krappinger D, Haug L, Gabl M. A prospective randomized trial comparing nonoperative treatment with volar locking plate fixation for displaced and unstable distal radial fractures in patients sixty-five years of age and older. J Bone Joint Surg Am. 2011; 93(23):2146–2153.

12. Trumble TE, Schmitt SR, Vedder NB. Factors affecting functional outcome of displaced intra-articular distal radius fractures. J Hand Surg Am. 1994; 19(2):325–340.

13. Makhni EC, Taghinia A, Ewald T, Zurakowski D, Day CS. Comminution of the dorsal metaphysis and its effects on the radiographic outcomes of distal radius fractures. J Hand Surg Eur Vol. 2010; 35(8):652–658.

14. Knirk JL, Jupiter JB. Intra-articular fractures of the distal end of the radius in young adults. J Bone Joint Surg Am. 1986; 68(5):647–659.

15. Handoll HH, Madhok R. Surgical interventions for treating distal radial fractures in adults. Cochrane Database Syst Rev. 2003; (3):CD003209.

16. Hove LM, Solheim E, Skjeie R, Sorensen FK. Prediction of secondary displacement in Colles' fracture. J Hand Surg Br. 1994; 19(6):731–736.

18. Makhni EC, Ewald TJ, Kelly S, Day CS. Effect of patient age on the radiographic outcomes of distal radius fractures subject to nonoperative treatment. J Hand Surg Am. 2008; 33(8):1301–1308.

19. Vatansever A, Piskin A, Kayalar M, Bal E, Ada S. The effect of dorsal cortical comminution on radiographic results of unstable distal radius fractures treated with closed reduction and K-wire fixation. Acta Orthop Traumatol Turc. 2007; 41(3):202–206.
20. Lafontaine M, Hardy D, Delince P. Stability assessment of distal radius fractures. Injury. 1989; 20(4):208–210.





 PDF
PDF ePub
ePub Citation
Citation Print
Print


 XML Download
XML Download