Abstract
Background
Many shoulder diseases are related to glenohumeral joint synovitis and effusion. The purpose of the present study is to detect effusion within the biceps long head tendon sheath as the sign of glenohumeral joint synovitis using ultrasonography, and to evaluate the clinical meaning of effusion within the biceps long head tendon sheath.
Methods
A consecutive series of 569 patients who underwent ultrasonography for shoulder pain were reviewed retrospectively and ultimately, 303 patients were included. The authors evaluated the incidence and amount of the effusion within the biceps long head tendon sheath on the ultrasonographic short axis view. Furthermore, the authors evaluated the correlation between the amount of effusion within the biceps long head tendon sheath and the range of motion and the functional score.
Results
The effusion within the biceps long head tendon sheath was detected in 58.42% of the patients studied: 69.23% in adhesive capsulitis, 56.69% in rotator cuff tear, 41.03% in calcific tendinitis, and 33.33% in biceps tendinitis. The average amount of the effusion within the biceps long head tendon sheath was 1.7 ± 1.6 mm, and it was measured to be the largest in adhesive capsulitis. The amount of effusion within biceps long head tendon sheath showed a moderate to high degree of correlation with the range of motion, and a low degree of correlation with the functional score and visual analogue scale for pain in each type of shoulder disease.
Conclusions
The effusion within the biceps long head tendon sheath is closely related to the range of motion and clinical scores in patients with painful shoulders. Ultrasonographic detection of the effusion within the biceps long head tendon sheath might be a simple and easy method to evaluate shoulder function.
The glenohumeral joint is a synovium-lined joint.1) Patients with shoulder disease frequently have glenohumeral synovitis, which produces a joint effusion. Hurt and Baker2) reported that calcific tendinitis is often associated with inflammatory conditions, such as synovitis or bursitis. Shindle et al.3) suggested that increased synovial inflammation is correlated with the tear size of the supraspinatus tendon. They also described that reducing synovial inflammation may break the cycle and mitigate the progression of tears. Therefore, it seems important to detect the presence of synovitis and assess the amount of joint effusion.
Ultrasonography is a non-invasive, rapid and relatively cost-effective imaging method which is used to assess a variety of shoulder diseases. Therefore, many surgeons use ultrasonography to detect various shoulder diseases in outpatient clinics, such as rotator cuff tear, calcific tendinitis, and bursitis.45) Ultrasonography generally detects rotator cuff tears with a sensitivity and specificity of up to 95%.678) However, it is still difficult to detect and quantify the joint effusion by ultrasonography due to the deep location of the glenohumeral joint.
Many ultrasonographic methods have been introduced to detect effusion of the glenohumeral joint. In 1989, Koski9) introduced a new ultrasonographic method to detect intra-articular effusion in the glenohumeral joint by measuring the distance between the humerus and the joint capsule in the axillary ultrasonographic view. Luukkainen et al.10) used Koski's method to detect intra-articular effusion of the glenohumeral joint in patients with rheumatoid arthritis, and emphasized that ultrasonography is necessary for the accurate diagnosis of glenohumeral joint effusion. Sanja and Mirjana11) evaluated glenohumeral joint effusion using a different method; they measured the distance between the joint capsule and the inferior margin of the infraspinatus tendon, and values above 2 mm were considered to be positive signs. They detected glenohumeral joint effusion in 28.6% of rheumatoid arthritis patients by this method. However, they could only detect the presence of glenohumeral joint effusion itself, and did not quantify the amount of effusion. Zubler et al.12) reported that glenohumeral joint effusion can be detected and quantified most reliably in the posterior glenohumeral joint recess, with the arm in external rotation. However, these ultrasonographic methods are difficult to perform and sometimes require expert skills, and there is interobserver bias as well. Zubler et al.12) also reported an easier method that involved measuring the width of the biceps tendon sheath for evaluating joint effusion. However, in their study, they simply checked the change in the width of the biceps tendon sheath after an injection of fluid into the glenohumeral joint.
We hypothesized that the effusion within the biceps long head tendon (BLHT) sheath would be related with variable shoulder diseases, and that there is a close relationship between the amount of effusion within the BLHT sheath and the functional outcome of shoulder. The purpose of the present study is to detect the effusion within the BLHT sheath using ultrasonography and to evaluate the clinical meaning of the effusion within the BLHT sheath.
A consecutive series of 569 patients with shoulder pain who underwent ultrasonography between December 2008 and January 2010 were included retrospectively. A single orthopaedic surgeon performed ultrasonographic examination in cases where the authors suspected specific shoulder diseases on plain radiograph and physical examinations, such as rotator cuff tear, frozen shoulder, calcific tendinitis, or biceps tendinitis. The inclusion criterion was any condition with a painful shoulders that underwent ultrasonographic examination. The exclusion criteria were as follows: patients under 18 years of age, a history of fracture and shoulder surgery, a history of intra-articular injection before ultrasonographic examination, and biceps deformation including partially or completely ruptured BLHT.
Ultimately, there were 303 patients available for the present study. The patients' average age was 57.22 years (range, 26 to 88 years). Men comprised 37.95% (n = 115) of the patients studied, whereas women comprised 62.05% (n = 188). All patients underwent ultrasonographic examinations before they received any treatment of the affected shoulder.
For the diagnosis of rotator cuff tear, the authors first used ultrasonography and then confirmed the final diagnosis by magnetic resonance imaging (MRI). On ultrasonographic examination, a hyper-echogenic signal change or focal decrease in the thickness of the tendon was considered to be a partial-thickness rotator cuff tear, and a hyper-echogenic gap in the tendon substance with retraction was considered to be a full-thickness rotator cuff tear. All patients who demonstrated these ultrasonographic findings underwent MRI to confirm the final diagnosis. For the diagnosis of calcific tendinitis, the authors made the diagnosis by plain radiograph. On standard anteroposterior radiographs, radio-opaque lesions visible in the rotator cuff area were considered to be calcific tendinitis. Furthermore, the authors checked the rotator cuff integrity on ultrasonography to rule out rotator cuff tearing. The authors considered the diagnosis of biceps tendinitis in patients with point tenderness in the bicipital groove and positive findings on Speed's test. Furthermore, the authors performed MRI in these patients to confirm biceps tendinitis and to rule out other pathologic conditions, including rotator cuff tear. On MRI, biceps tendinitis demonstrated a signal change within the tendon or an irregular margin and a change in the diameter of the tendon.
Adhesive capsulitis is well known to be characterized by a functional restriction of both active and passive shoulder motions, and the radiographs of the glenohumeral joint in this condition are essentially unremarkable.13) However, there is no confirmed definition of the degree of shoulder motion restriction. In the present study, the authors defined shoulder stiffness as forward flexion that was less than 120° on passive motion, or external rotation with the arm at the side of less than 30° on passive motion, or internal rotation at the back that was lower than the third lumbar vertebral level passively.14) The authors performed ultrasonography and MRI on all patients with adhesive capsulitis to rule out combined shoulder lesions. If shoulder stiffness was combined with other lesions, it was categorized as part of the main shoulder disease, and not as adhesive capsulitis; for example, a rotator cuff tear with stiffness was considered part of the rotator cuff tear group, and not as part of the adhesive capsulitis group.
Ultrasonographic examination was performed by a single orthopaedic surgeon experienced in ultrasonography and blinded to the clinical test. A Philips HD11 XE ultrasound machine (Amsterdam, The Netherlands) was used with a high-frequency 12 to 5 MHz linear-array transducer.
The patients were seated in the upright position with the arm in the neutral position, the elbow flexed to 90° and the palm face up. The ultrasonographic transducer was placed in the short axis of the BLHT at about 1 cm inferior to the coracoid process. The BLHT was scanned in the short axis. If low-echogenic fluid was detected around the BLHT in the short axis view, the authors considered that there would be an appreciably sized glenohumeral joint effusion present. We measured the amount of effusion within the BLHT sheath as the length of effusion in the short axis view, that is, the longest distance from the sheath to the tendon margin was evaluated (Fig. 1). Zubler et al.12) reported that in their ultrasonographic study, the fluid collection in the BLHT sheath was 0.6 mm and that it increased to more than 0.9 mm after an injection of 8 to 12 mL fluid into the glenohumeral joint. Therefore, we considered shoulders showing an effusion of more than 0.9 mm to indicate effusion within the BLHT sheath.
The clinical data and functional scores were checked at the same time of the ultrasonographic examination by another single orthopaedic surgeon. The clinical data were assessed by the visual analogue scale (VAS) for pain and the passive range of motion of the affected shoulder: forward flexion with fixed scapular motion, external rotation in 90° abduction, external rotation at the side, and internal rotation at the back. The VAS for pain ranged from 0 to 10, with 10 being the worst pain. The passive range of motion was measured with a full-circle manual goniometer for forward flexion and external rotation. The internal rotation level was checked by an indirect method, where the hand was passively placed behind the back and the vertebral level that was reached by the tip of the extended thumb was recorded. For easy statistical analysis, we converted the internal rotation levels into contiguously numbered groups: 0 for sacral level, 1 to 5 for L5 to L1, and 6 to 12 for T12 to T6.
The functional scores, including the American Shoulder and Elbow Surgery (ASES) score, Simple Shoulder Test (SST) score and the Korean Shoulder Score (KSS) were also evaluated at the time of the ultrasonographic examination. The study protocol was approved by the Institutional Review Board of Seoul St. Mary's Hospital, College of Medicine, The Catholic University of Korea (Study No. KC13RISI0356).
All statistical analyses were performed using the IBM SPSS ver. 22.0 (IBM Co., Armonk, NY, USA), and p-value < 0.05 was considered statistically significant. The one-way analysis of variance and Student t-test were performed to determine the difference in the amount of effusion within the BLHT sheath between the diseases. Pearson correlation coefficients (PCC) were calculated to determine the correlation between the amount of the effusion within the BLHT sheath and the functional outcome.
There were 157 shoulders with rotator cuff tear, 104 shoulders with adhesive capsulitis, 39 shoulders with calcific tendinitis, and three shoulders with biceps tendinitis. All patients with calcific tendinitis showed no combined rotator cuff tear, and rotator cuff tear combined with small calcification less than 2 mm were categorized to rotator cuff tear group. All shoulders with biceps tendinitis showed signal changes with the fraying of the biceps tendon on MRI.
The average of the VAS for pain was found to be 4.8 ± 2.7 in the rotator cuff tear group, 5.3 ± 2.9 in the adhesive capsulitis group, 4.7 ± 2.8 in the calcific tendinitis group, and 4.5 in the biceps tendinitis group. The overall results for the ASES score were 58.5 points in the rotator cuff tear group, 58.8 points in the adhesive capsulitis group, 58.1 points in the calcific tendinitis group, and 53.3 points in the biceps tendinitis group. For the SST score, the results were as follows: 58.0 points in the rotator cuff tear group, 45.6 points in the adhesive capsulitis group, 51.9 points in the calcific tendinitis group, and 58.3 points in the biceps tendinitis group. For the KSS score, the results were as follows: 42.4 points in the rotator cuff tear group, 40.8 points in the adhesive capsulitis group, 41.8 points in the calcific tendinitis group, and 41.0 points in the biceps tendinitis group.
Effusion within the BLHT sheath was detected in 58.42% (n = 178) of the patients in this study: 69.23% (n = 72) of patients with adhesive capsulitis, 56.69% (n = 89) of patients with rotator cuff tear, 41.03% (n = 16) of patients with calcific tendinitis, and 33.33% (n = 1) of patients with biceps tendinitis (Fig. 2).
The average amount of the effusion within the BLHT sheath was 1.7 ± 1.6 mm: 2.0 ± 1.6 mm in patients with adhesive capsulitis, 1.6 ± 1.6 mm in patients with rotator cuff tear, 1.2 ± 1.6 mm in patients with calcific tendinitis, and 1.1 ± 1.8 mm in patients with biceps tendinitis. The amount of the effusion within the BLHT sheath in patients with adhesive capsulitis was significantly larger than that in patients with calcific tendinitis (p = 0.03). However, there were no statistically significant differences between the other shoulder diseases (Fig. 3). The correlation coefficient of the intraobserver reliability was 0.80 (p < 0.05).
The amount of the effusion within the BLHT sheath overall had a negative correlation with the range of motion in all patients: forward flexion (PCC = -0.491; p < 0.05), external rotation in 90° abduction (PCC = -0.381; p < 0.05), external rotation at the side (PCC = -0.356; p < 0.05), and internal rotation (PCC = -0.486; p < 0.05). In patients with adhesive capsulitis, PCC was -0.349 with forward flexion (p < 0.05), -0.310 with external rotation in 90° abduction (p < 0.05), -0.280 with external rotation at the side (p < 0.05), and -0.385 with internal rotation (p < 0.05). In patients with rotator cuff tear, the PCC was -0.509 with forward flexion (p < 0.05), -0.379 with external rotation at 90° abduction (p < 0.05), -0.364 with external rotation at the side (p < 0.05), and -0.506 with internal rotation (p < 0.05). In patients with calcific tendinitis, PCC was -0.769 with forward flexion (p < 0.05), -0.456 with external rotation in 90° abduction (p < 0.05), -0.432 with external rotation at the side (p < 0.05), and -0.537 with internal rotation (p < 0.05) (Table 1).
The amount of the effusion within the BLHT sheath had a negative correlation with the functional score in each disease group. However, the correlation coefficients were relatively low: in patients with adhesive capsulitis, ASES PCC = -0.311 (p < 0.05), SST PCC = -0.268 (p < 0.05), and KSS PCC = -0.342 (p < 0.05); in patients with rotator cuff tear, ASES PCC = -0.449 (p < 0.05), SST PCC = -0.402 (p < 0.05), and KSS PCC = -0.380 (p < 0.05); and in patients with calcific tendinitis, ASES PCC = -0.400 (p < 0.05), SST PCC = -0.275 (p < 0.05), and KSS PCC = -0.343 (p < 0.05). Furthermore, the VAS for pain showed a weak positive correlation with the amount of the effusion within the BLHT sheath in each shoulder disease: adhesive capsulitis PCC = 0.109 (p < 0.05), rotator cuff tear PCC = 0.183 (p < 0.05), and calcific tendinitis PCC = 0.188 (p < 0.05) (Table 2).
The effusion within the BLHT sheath was detected in 58.42% of all patients and the average amount was 1.7 ± 1.6 mm in all patients of the present study. Among them, patients with adhesive capsulitis showed effusion within the BLHT sheath most frequently, and the average amount of that group was larger than that of the other shoulder diseases. Because the effusion within the BLHT sheath looks like a fried egg, the authors newly deemed it as the "fried egg sign." The amount of effusion within the BLHT sheath showed a negative correlation with the range of motion and functional scores in each group. In particular, the forward flexion and internal rotation levels were most closely correlated with the amount of effusion within the BLHT sheath in each group.
The glenohumeral joint cavity communicates with the BLHT sheath; thus, profuse effusion of the glenohumeral joint may lead to an increase in the effusion within the tendon sheath. Zubler et al.12) reported that in their ultrasonographic study, the width of the anechoic fluid collection in the BLHT sheath was increased after 8 to 12 mL of fluid was injected into the glenohumeral joint in most cases. These findings suggest that the amount of hypoechogenic fluid in the BLHT sheath may represent the ratio of the amount of glenohumeral joint effusion to the volume of the glenohumeral joint cavity. In the other words, effusion in the BLHT sheath can represent synovitis and capsultis. However, Zubler et al.12) did not evaluate the correlation between the effusion within the BLHT sheath and clinical outcomes, they suggested that the effusion within the BLHT sheath might represent glenohumeral joint effusion.
In the present study, the effusion within the BLHT sheath was more frequently observed in adhesive capsulitis and the amount of effusion within BLHT sheath showed a negative correlation with the range of motion. Joint shrinkage is generally observed in shoulders with adhesive capsulitis. In adhesive capsulitis, the axillary fold is contracted, and that reduces the joint volume to below 15 mL.15) Furthermore, joint shrinkage might push the joint fluid to another space, the BLHT sheath. Therefore, the more the joint shrinks, the more joint fluid is collected in the BLHT sheath. The results of the present study correspond well with this hypothesis.
The amount of effusion within the BLHT sheath showed a higher correlation with the range of motion than with the variable functional score or shoulder pain. The effusion within the BLHT sheath was thought to be related to the status of synovitis or capsulitis. Several studies with synovial or capsular biopsy specimens from patients with adhesive capsulitis have demonstrated that variable proinflammatory cytokines and neovascularizations are involved in synovial hyperplasia and capsular fibrosis.1617) Adhesive capsulitis, initially described by Neviaser,18) is thought to be a combination of synovial inflammation and capsular fibrosis.15) Thus, the limitation of the range of motion is thought to be closely correlated with joint synovitis, and in the present study, the range of motion was also closely correlated with the amount of effusion within the BLHT sheath. Therefore, in adhesive capsulitis, combined synovitis and capsulitis can lead to increased joint effusion and joint cavity shrinkage, and these conditions might produce the appearance of the effusion within the BLHT sheath in shoulders with adhesive capsulitis. Functional scores and shoulder pain are mainly affected by the severity of each disease; however, in this study, we aimed to evaluate the clinical meaning of the effusion within the BLHT sheath, something we frequently encountered during ultrasonographic examinations.
Effusion within the BLHT sheath was detected in 56.69% of patients with rotator cuff tear. Several studies showed that low- to mild-grade synovial inflammation is present in shoulders with rotator cuff tears.31920) The expression levels of interleukin 1-beta and several degradative enzymes were highly upregulated in the synovium of patients with rotator cuff lesions, and these findings suggest that chronic synovitis is associated with rotator cuff tears.19) Therefore, chronic synovitis combined with rotator cuff tears might lead to an increase in joint effusion, and these findings would be detected as effusion within the BLHT sheath.
In calcific tendinitis, there was a stronger correlation between the amount of effusion within the BLHT sheath and range of motion than in rotator cuff tears. Calcific tendinitis can be divided into three distinct stages: precalcific, calcific, and postcalcific.21) Among these stages, the postcalcific stage usually shows milky or creamy calcific deposits which frequently induce acute sharp pain, combined with acute synovitis or bursitis. Thus, acute synovitis in calcific tendinitis might induce increased joint effusion and severely painful limited range of motion. This may be the reason for the stronger correlation between the amount of effusion within the BLHT sheath and the range of motion in calcific tendinitis.
Several studies have suggested that a fluid collection in the biceps tendon sheath may be induced by biceps tendinitis.2223) In the present study, only three patients had biceps tendinitis, and among them, only one patient showed effusion within the BLHT sheath. We had only three cases of biceps tendinitis, because our categorization, exclusion criteria, and low incidence of ultrasonographic examination in isolated biceps lesions. Because of low sample size of biceps lesions in the present study, the authors could not evaluate this lesion to a statistical degree. However, it is believed that the fluid collection in the biceps tendon sheath may be influenced by joint effusion, rather than by the condition of the local bicep.
There are some limitations in the present study. First, this was a retrospective time-zero study. Although, the final diagnosis was confirmed at the last follow-up, the authors did not trace the patients' symptoms and functional outcomes after the ultrasonographic examination. Furthermore, because patients underwent different treatments according to their individual diagnosis, the correlation between the effusion within the BLHT sheath and disease prognosis could not be evaluated. Second, in the present study, if shoulder stiffness was combined with another shoulder disease, it was categorized as the main shoulder disease, and not as adhesive capsulitis. We simply categorized the rotator cuff tear patients with stiffness into the rotator cuff tear group, for example. However, it is well known that there are many differences between rotator cuff tear with stiffness and rotator cuff tear without stiffness, including symptoms and treatment. Third, there was no control group. We did not evaluate normal shoulders as control group. Because, there would be asymptomatic effusion within BLHT sheath, the percentage of 'fried egg sign' in each disease and conclusion of the present study might be different if the results were compared with control group. Lastly, we evaluated the effusion within the BLHT sheath using ultrasonography, so a bias might occur according to direction and location of ultrasonographic transducer (the intraobserver reliability was 0.80). The location and thickness of the biceps tendon within the BLHT sheath also could provide a bias. To reduce the variance, the examiner tried to locate the transducer at the same location in the same shoulder position and shoulders with biceps deformation, especially with biceps tendinitis or biceps tear, were excluded in the present study.
In conclusion, the effusion within the BLHT sheath is closely related to the range of motion and clinical scores in patients with painful shoulders. The ultrasonographic detection of the effusion within the BLHT sheath might be useful to evaluate shoulder functions. However, further studies are required to understand the correlation between the effusion within the BLHT sheath and disease prognosis.
Figures and Tables
Fig. 1
Effusion within the biceps long head tendon sheath. The longest distance from the sheath to the tendon margin of the long head biceps tendon (arrow) was measured as the amount of the effusion within the biceps long head tendon sheath. GT: greater tubercle, LT: lesser tubercle.

Fig. 2
The incidence of effusion within the biceps long head tendon sheath in each type of shoulder disease.
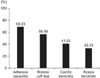
Fig. 3
The amount of effusion within the biceps long head tendon sheath in each type of shoulder disease.
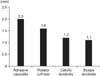
Table 1
Correlations between the Amount of Effusion within the Biceps Long Head Tendon Sheath and Range of Motion

Table 2
Correlations between the Amount of Effusion within the Biceps Long Head Tendon Sheath and Functional Score

References
1. Middleton WD. Ultrasonography of the shoulder. Radiol Clin North Am. 1992; 30(5):927–940.
2. Hurt G, Baker CL Jr. Calcific tendinitis of the shoulder. Orthop Clin North Am. 2003; 34(4):567–575.

3. Shindle MK, Chen CC, Robertson C, et al. Full-thickness supraspinatus tears are associated with more synovial inflammation and tissue degeneration than partial-thickness tears. J Shoulder Elbow Surg. 2011; 20(6):917–927.

4. Saboeiro GR. Sonography in the treatment of calcific tendinitis of the rotator cuff. J Ultrasound Med. 2012; 31(10):1513–1518.

5. Yablon CM, Bedi A, Morag Y, Jacobson JA. Ultrasonography of the shoulder with arthroscopic correlation. Clin Sports Med. 2013; 32(3):391–408.

6. Al-Shawi A, Badge R, Bunker T. The detection of full thickness rotator cuff tears using ultrasound. J Bone Joint Surg Br. 2008; 90(7):889–892.

7. Iannotti JP, Ciccone J, Buss DD, et al. Accuracy of office-based ultrasonography of the shoulder for the diagnosis of rotator cuff tears. J Bone Joint Surg Am. 2005; 87(6):1305–1311.

8. Teefey SA, Rubin DA, Middleton WD, Hildebolt CF, Leibold RA, Yamaguchi K. Detection and quantification of rotator cuff tears: comparison of ultrasonographic, magnetic resonance imaging, and arthroscopic findings in seventy-one consecutive cases. J Bone Joint Surg Am. 2004; 86(4):708–716.
9. Koski JM. Axillar ultrasound of the glenohumeral joint. J Rheumatol. 1989; 16(5):664–667.
10. Luukkainen R, Sanila MT, Luukkainen P. Poor relationship between joint swelling detected on physical examination and effusion diagnosed by ultrasonography in glenohumeral joints in patients with rheumatoid arthritis. Clin Rheumatol. 2007; 26(6):865–867.

11. Sanja MR, Mirjana ZS. Ultrasonographic study of the painful shoulder in patients with rheumatoid arthritis and patients with degenerative shoulder disease. Acta Reumatol Port. 2010; 35(1):50–58.
12. Zubler V, Mamisch-Saupe N, Pfirrmann CW, Jost B, Zanetti M. Detection and quantification of glenohumeral joint effusion: reliability of ultrasound. Eur Radiol. 2011; 21(9):1858–1864.

13. Zuckerman JD, Rokito A. Frozen shoulder: a consensus definition. J Shoulder Elbow Surg. 2011; 20(2):322–325.

14. Oh JH, Kim SH, Lee HK, Jo KH, Bin SW, Gong HS. Moderate preoperative shoulder stiffness does not alter the clinical outcome of rotator cuff repair with arthroscopic release and manipulation. Arthroscopy. 2008; 24(9):983–991.

15. Hsu JE, Anakwenze OA, Warrender WJ, Abboud JA. Current review of adhesive capsulitis. J Shoulder Elbow Surg. 2011; 20(3):502–514.

16. Rodeo SA, Hannafin JA, Tom J, Warren RF, Wickiewicz TL. Immunolocalization of cytokines and their receptors in adhesive capsulitis of the shoulder. J Orthop Res. 1997; 15(3):427–436.

17. Ryu JD, Kirpalani PA, Kim JM, Nam KH, Han CW, Han SH. Expression of vascular endothelial growth factor and angiogenesis in the diabetic frozen shoulder. J Shoulder Elbow Surg. 2006; 15(6):679–685.

18. Neviaser JS. Adhesive capsulitis of the shoulder (the frozen shoulder). Med Times. 1962; 90(8):783–807.
19. Gotoh M, Hamada K, Yamakawa H, et al. Perforation of rotator cuff increases interleukin 1beta production in the synovium of glenohumeral joint in rotator cuff diseases. J Rheumatol. 2000; 27(12):2886–2892.
20. Lo IK, Marchuk LL, Hollinshead R, Hart DA, Frank CB. Matrix metalloproteinase and tissue inhibitor of matrix metalloproteinase mRNA levels are specifically altered in torn rotator cuff tendons. Am J Sports Med. 2004; 32(5):1223–1229.

21. Uhthoff HK, Loehr JW. Calcific tendinopathy of the rotator cuff: pathogenesis, diagnosis, and management. J Am Acad Orthop Surg. 1997; 5(4):183–191.





 PDF
PDF ePub
ePub Citation
Citation Print
Print


 XML Download
XML Download