Abstract
Background
Previous reports have observed differences only in infection rates between posterolateral fusion and posterior lumbar interbody fusion (PLIF). There have been no reports that describe the particular features of surgical site infection (SSI) in PLIF. In this study, we endeavor to identify the distinguishing characteristics and risk factors of SSI in PLIF.
Methods
Our study undertook a review of a case series of an institute. Patients who had undergone PLIF consecutively in the author's hospital were reviewed. Two proactive procedures were introduced during the study period. One was irrigation of the autolocal bone, and the other was the intradiscal space irrigation with a nozzle. Infection rate and risk factors were analyzed. For subgroup analysis, the elapsed time to a diagnosis (ETD), clinical manifestations, hematologic findings, and causative bacteria were examined in patients with SSI.
Results
In a total of 1,831 cases, there were 30 cases of SSI (1.6%). Long operation time was an independent risk factor (p = 0.008), and local bone irrigation was an independent protective factor (p = 0.001). Two cases of referred SSI were included in the subgroup analysis. There were 6/32 (19%) superficial incisional infections (SII), 6/32 (19%) deep incisional infections (DII), and 20/32 (62%) organ/space infections (O/SI). The difference of incidence among three groups was significant (p = 0.002).The most common bacteria encountered were methicillin-resistant Staphylococcus epidermidis followed by methicillin-resistant S. aureus in incisional infections, and no growth followed by S. epidermidis in O/SI. ETD was 8.5 ± 2.3 days in SII, 8.7 ± 2.3 days in DII and 164.5 ± 131.1 days in O/SI (p = 0.013).
Conclusions
The rate of SSI in PLIF was 1.6%, with the most common type being O/SI. The causative bacteria of O/SI was of lower virulence than in the incisional infection, and thus diagnosis was delayed due to its latent and insidious feature. Contamination of auto-local bone was presumed attributable to the progression of SSI. Irrigation of auto-local bone helped in the reduction of SSI.
Posterior lumbar interbody fusion (PLIF) has been widely applied to various degenerative spinal diseases, being more beneficial than other fusion methods. Sagittal reconstruction is more feasible12) where the fusion rate is higher.345) However, more complications are unavoidable. Retraction of nerve root and cauda equine cause more neurological complications6) and the risk of surgical site infection (SSI) increases due to the extended operation time and tissue damage, increased blood loss, and foreign materials in the interbody space.78) We have observed that PLIF not only has a higher rate of SSI than posterolateral fusion (PLF), but also has different features. The locations of infection, the causative organisms and the patterns of clinical manifestations were different from PLF. Nevertheless, there have been only few reports regarding the SSI of PLIF.
This was a retrospective descriptive and case controlled observational study. The study was approved by the Institutional Review Board. Those who had undergone spinal surgeries in the Seoul Sacred Heart General Hospital between January 2005 and September 2012 were reviewed. The patients who received single or multiple PLIFs, or PLIFs for more than half of the fused segments, were included. All cases were consecutive. Repeated operations of the same patients were counted as different cases. Follow-up period was limited to 2 years. Those who had no complaints or clinical signs suggesting an infection during the follow-up period were regarded as non-infected cases. Image test review was not a prerequisite in all cases; however, all infection cases were reviewed. The overall rate and annual rate of SSI were investigated. Classification was performed as per the criteria of Center for Disease Control and Prevention (CDC) of USA: superficial incisional infection (SII) involves only skin or subcutaneous tissue of the incision, deep incisional infection (DII) involves deep soft tissues (e.g., fascial and muscle layers) of the incision, and organ/space infection (O/SI) involves any part of the anatomy, other than the incision, which was opened or manipulated during the operation. Age, sex, amount of blood loss, operation time, number of fused segments, association with diabetes mellitus, whether virgin or revision surgery, local bone irrigation and intradiscal irrigation, were other features analyzed as parameters of risk factors. Other subgroup analyses included difference of elapsed time to a diagnosis (ETD), local and general manifestations, blood test, loosening of implants, and the causative bacteria among the different types of infections. The time of diagnosis was determined as the time when infectious exudates were discovered from the wound in cases of incisional infection, and as the time when antibiotics were started on the evidences of image and laboratory findings in cases of spondylitis. There were two transferred cases that were excluded from the risk factor analysis and included in subgroup analysis of infection cases.
In the statistical analysis of risk factors, independent t-test for ratio variables and Fisher exact test for nominal variables were applied for single variable analysis, and logistic regression analysis was applied for multiple variables analysis. In the analysis of differences among types, chi-squared test, Fisher exact test and analysis of variance were applied. In subgroup analysis, linear by linear association was applied when expected value was less than 5. Significant p-value was defined as 0.1 in single variable risk factor analysis and 0.05 for the others. SPSS ver. 16.0 (SPSS Inc., Chicago, IL, USA) package was used for all analysis.
There were 2,347 PLIF cases during the study period. Of these, 516 cases were excluded due to ineligibility of medical records. Finally, 1,831 cases were included (Fig. 1). There were 1,322 cases of one segment, 387 cases of 2 segments, 96 cases of 3 segments, and 4 cases of 4 or more segments. A total of 30 cases developed SSI, the incidence being 1.6%. There was a significant difference in annual incidence (p = 0.008) (Fig. 2). Two additional procedures were added during the study period. Irrigation of local bone commenced from February 2007, and intradiscal irrigation with a nozzle began from January 2010. Two SSI cases were transferred from other hospitals. Classification was as follows: 19% (6/32) SII, 19% (6/32) DII, and 62% (20/32) O/SI (all were spondylitis cases) (Fig. 3). The incidence was significantly different (p = 0.002).
According to the single variable analysis, sex, operation time, local bone irrigation and intradiscal irrigation were significant (p < 0.01) (Table 1). However, in multiple logistic regression analysis, the longer operation time increased the risk (p = 0.008; odds ratio [OR], 0.316), and local bone irrigation decreased the risk (p = 0.001; OR, 5.248) significantly (Table 2). Male gender was close to significant level (p = 0.087). Operation time was converted to dichotomous categorical variable. The curr off point was decided as 157 months, which was the point which made largest area under the receiver operating characteristic curve.
Demographics of SSI cases are described in Table 3. SII and DII were confirmed by microbiological or histological examination of the exudates and tissues. SII patients reported having a general fever in 2/6 (33%) cases and local heating in 6/6 (100%) cases. DII patients had 3/6 (50%) and 4/6 (67%) cases, respectively. However, O/SI patients had no local wound manifestation and general fever. Its diagnosis depended on clinical findings such as pain, local tenderness, blood tests and image test. Those who underwent surgical treatment were reconfirmed by microbiological or histological test. Microbiological test was not carried out in a total of 10 cases, and 6 cases showed no growth. Of the 6 SII cases, there were 3 methicillin-resistant Staphylococcus epidermidis (MRSE), 2 methicillin-resistance S. aureus (MRSA), and 1 S. epidermidis infections. Of the 6 DII cases, there were 2 MRSE, 2 S. epidermidis and 2 unidentifiable cases. In the 20 cases of O/SI, there was 1 MRSE, 2 S. epidermidis, 1 S. aureus, 1 S. pyogenes, 1 Escherichia coli and 4 unidentified cases; 10 cases had no microbiological examination.
On image test, there was no implant loosening in SII and DII, but 10/20 (50%) O/SIs showed implant loosening. C-reactive protein was elevated at the time of diagnosis, as compared to preoperative levels, from 0.6 ± 1.3 to 3.6 ± 3.0 (p = 0.000). However, there was no difference among the groups (preoperative, p = 0.430; at the time of diagnosis, p = 0.905). The average ETD was 106 days (range, 6 to 410 days). It differed according to the groups: 8.5 ± 2.3 days in SII, 8.7 ± 2.3 days in DII, and 164.5 ± 131.1 days in O/SI (p = 0.002). In O/SIs, those who had implant loosening showed longer ETD than those who had no loosening (234.0 ± 107.3 days and 94.9 ± 118.1 days, respectively; p = 0.013).
There is an increased application of PLIFs using pedicle screws and cages. It enables to reconstruct the anterior column through a posterior approach. Thus, it is more feasible to achieve sagittal reconstruction and bone union.12345) However, complications occur more frequently as the surgical procedure is more complex and extended. The incidence of SSI in instrumented PLIF has been reported over a wide range from 3.0% to 7.2%.67910) This was higher than instrumented PLF.678910) Yashiro et al.9) indicated that increased blood loss, longer operation time and tissue damage were attributable. While most types of SSI in PLF were incisional infection, majorly was found as spondylitis, especially in the vicinity of grafted bone and cage in PLIF.8) The current study implied the epidemiology of infection in PLIF would be different from PLF, by presenting that 67% of SSI were spondylitis. The local bone chips prepared for graft were usually contaminated by bacteria of the room air, and intradiscal space was contaminated more than the muscle layer after conventional wound irrigation.11) Furthermore, irrigation of local bone chips decreased the infection rate. Based on the above evidences, the mechanism of development of spondylitis was inferred as follows: the bacteria which contaminated local bone chips and intradiscal space adhere to the remaining avascular disc materials and cages. They are protected from antibiotics by a biofilm and thus develop a latent infection. Intradiscal irrigation with a narrow tip nozzle was expected to be effective to prevent spondylitis. However, this was not proved in multivariate analysis. It was thought that the incidence of SSI was remarkably reduced after the implementation of local bone irrigation and it also had colinearity with local bone irrigation.
Diagnosis and classification followed the CDC criteria. 12) A distinctive feature of the criteria is that it includes O/SI which has no infection at the approach route. In spine surgeries, spondylitis, discitis and meningitis are included in this class.12) Though the O/SI began from the disc space, it seemed appropriate to label them as 'spondylitis' because most of the disc was already removed in PLIF. The criteria extend the diagnostic time up to 12 months in case of implant related DII and O/SI.12) Richards13) diagnosed SSI at an average of 27 months after surgeries for adolescent idiopathic scoliosis. Clark and Shufflebarger14) evaluated at 31 months average. These usually showed no growth or low virulence normal flora of the human skin on microbiological exam.15) Clark and Shufflebarger14) succeeded to identify S. epidermidis by extending the culture period up to 10 days. All of their cases were DII. Anaerobic bacterial contamination of disc after spinal operation has also been reported.16171819) Anaerobic bacteria are usually difficult to identify. Therefore, the no growth cases in our study were presumed as anaerobic bacterial infections. In the current study, while SIIs and DIIs were diagnosed at about 9 days, O/SIs were diagnosed at an average of 165 days, and the most delayed case was at 410 days after the surgery. All latent SSIs were O/SIs, and all the causative bacteria were either having low virulence or were not identified. Thus, latent SSI caused by low virulent bacteria was considered as a particular feature of implant related SSI in PLIF.
Contamination during an operation is unavoidable. Dietz et al.20) reported that 58% of the elective orthopedic surgeries had bacterial contamination. According to an intraoperative experiment, surgical wound, local bone harvested from decompression sites, gloves of surgeons and implants were contaminated by the same bacteria which were cultured from the room air of the operation theater, and the degree of contamination increased proportionally to the exposed time.1121) Latent spondylitis in PLIF has been reported as an unusual case.2223) However, our study showed that it was the major type of SSI in PLIF and strongly suggests that it could be a cardinal reason why PLIF has more SSI than PLF. It made us hypothesize that the chance of contamination by low virulence bacteria is higher and there are more refuges for them. The vectors more liable in contamination are local bone chips and cages, and the refuges are avascular disc material and intradiscal space which are not irrigated effectively. The reasons why diagnosis of O/SI was delayed include the late development of clinical symptoms, and inappropriate workup because of vague clinical manifestation. All O/SIs of the current study had no general fever or local inflammatory symptoms. Local tenderness and pain, which increased with motility, were the only clinical findings. All of them had compatible hematologic findings. Therefore, diagnosis depended on suspicion through clinical findings, and was confirmed by hematological and image tests. However, these kinds of symptoms are not rare in spine fusion patients, and simple radiological findings, such as implant loosening or erosion of end plates, are akin to aseptic nonunion. Many of the current cases were treated mistakenly as usual chronic back pain and received epidural steroid injections, even though manifestations of infection had already begun. Thus, the first step of diagnosis is having a suspicion. If it is supported by hematological examinations and image tests such as magnetic resonance imaging (MRI) and computed tomography (CT) scan, diagnosis can be decisive.
There were several limitations in the current study. All potential variables for risk factors were not considered due to its retrospective design. Interbody graft materials were not unified. Even though auto-iliac bone, demineralized bone matrix, calcium phosphate, and fresh allergenic bone were added to extend the graft material, the major component was auto-local bone in all cases.
The rate of SSI in PLIF was 1.6%. The particular feature was O/SI, i.e., spondylitis, which did not have incisional infection. This kind of infection showed either no bacterial growth or bacteria with low virulence, and was not accompanied by general manifestations of infection. Contamination of local bone chips which were harvested while performing decompression was regarded as an important cause, and irrigation of these had a preventive effect. Longer operation time also increased the risk independently. Latent spondylitis caused by low virulence bacteria developed later. Furthermore, appropriate diagnosis and treatment were delayed due to its vague and confusing clinical and radiological findings. Thus, having a clinical suspicion should be followed by hematological tests and image tests such as MRI and CT to reach a confirmatory diagnosis. Given the causative organisms were normal floras of human skin, thorough control of operation environment is considered to reduce SSI in PLIF.
Figures and Tables
 | Fig. 1Flow chart of patients as a whole. PLIF: posterior lumbar interbody fusion, F/U: follow-up, SSI: surgical site infection. |
 | Fig. 3A typical case of organ/space infection. (A) The simple lateral radiograph of spondylitis shows osteolysis of both facing end plates, migration of cages, and loosening of pedicle screws. (B) The T1-weighted sagittal magnetic resonance imaging view shows low signal change of both facing end plates and vertebral bodies. However, there was no infection signal at approach route. (C) The axial view of computed tomography shows Swiss cheese-like end plate resorption. |
Table 1
Single Variable Analysis of Risk Factors
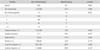
Table 2
Multivariate Logistic Regression Test on Risk Factors

Table 3
Demographics of Surgical Site Infection Cases

References
1. Ha KY, Na KH, Shin JH, Kim KW. Comparison of posterolateral fusion with and without additional posterior lumbar interbody fusion for degenerative lumbar spondylolisthesis. J Spinal Disord Tech. 2008; 21(4):229–234.

2. Musluman AM, Yilmaz A, Cansever T, et al. Posterior lumbar interbody fusion versus posterolateral fusion with instrumentation in the treatment of low-grade isthmic spondylolisthesis: midterm clinical outcomes. J Neurosurg Spine. 2011; 14(4):488–496.

3. Farrokhi MR, Rahmanian A, Masoudi MS. Posterolateral versus posterior interbody fusion in isthmic spondylolisthesis. J Neurotrauma. 2012; 29(8):1567–1573.

4. Liu X, Wang Y, Qiu G, Weng X, Yu B. A systematic review with meta-analysis of posterior interbody fusion versus posterolateral fusion in lumbar spondylolisthesis. Eur Spine J. 2014; 23(1):43–56.

5. Ye YP, Xu H, Chen D. Comparison between posterior lumbar interbody fusion and posterolateral fusion with transpedicular screw fixation for isthmic spondylolithesis: a meta-analysis. Arch Orthop Trauma Surg. 2013; 133(12):1649–1655.

6. Okuyama K, Abe E, Suzuki T, Tamura Y, Chiba M, Sato K. Posterior lumbar interbody fusion: a retrospective study of complications after facet joint excision and pedicle screw fixation in 148 cases. Acta Orthop Scand. 1999; 70(4):329–334.

7. Pappou IP, Papadopoulos EC, Sama AA, Girardi FP, Cammisa FP. Postoperative infections in interbody fusion for degenerative spinal disease. Clin Orthop Relat Res. 2006; 444:120–128.

8. Ahn DK, Park HS, Choi DJ, et al. The difference of surgical site infection according to the methods of lumbar fusion surgery. J Spinal Disord Tech. 2012; 25(8):E230–E234.

9. Yashiro K, Homma T, Hokari Y, Katsumi Y, Okumura H, Hirano A. The Steffee variable screw placement system using different methods of bone grafting. Spine (Phila Pa 1976). 1991; 16(11):1329–1334.

10. Mirovsky Y, Floman Y, Smorgick Y, et al. Management of deep wound infection after posterior lumbar interbody fusion with cages. J Spinal Disord Tech. 2007; 20(2):127–131.

11. Ahn DK, Choi DJ, Park HS, Kim TW, Chun TH, Yang JH. Precautions against infection following posterior spinal fusion based on types of infection and risk factors. J Korean Soc Spine Surg. 2009; 16(4):274–284.

12. Mangram AJ, Horan TC, Pearson ML, Silver LC, Jarvis WR. Guideline for prevention of surgical site infection, 1999. Centers for Disease Control and Prevention (CDC) Hospital Infection Control Practices Advisory Committee. Am J Infect Control. 1999; 27(2):97–132.
13. Richards BS. Delayed infections following posterior spinal instrumentation for the treatment of idiopathic scoliosis. J Bone Joint Surg Am. 1995; 77(4):524–529.

14. Clark CE, Shufflebarger HL. Late-developing infection in instrumented idiopathic scoliosis. Spine (Phila Pa 1976). 1999; 24(18):1909–1912.

15. Richards BR, Emara KM. Delayed infections after posterior TSRH spinal instrumentation for idiopathic scoliosis: revisited. Spine (Phila Pa 1976). 2001; 26(18):1990–1996.
16. Albert HB, Sorensen JS, Christensen BS, Manniche C. Antibiotic treatment in patients with chronic low back pain and vertebral bone edema (Modic type 1 changes): a double-blind randomized clinical controlled trial of efficacy. Eur Spine J. 2013; 22(4):697–707.

17. Albert HB, Lambert P, Rollason J, et al. Does nuclear tissue infected with bacteria following disc herniations lead to Modic changes in the adjacent vertebrae? Eur Spine J. 2013; 22(4):690–696.

18. Carricajo A, Nuti C, Aubert E, et al. Propionibacterium acnes contamination in lumbar disc surgery. J Hosp Infect. 2007; 66(3):275–277.

19. Stirling A, Worthington T, Rafiq M, Lambert PA, Elliott TS. Association between sciatica and Propionibacterium acnes. Lancet. 2001; 357(9273):2024–2025.

20. Dietz FR, Koontz FP, Found EM, Marsh JL. The importance of positive bacterial cultures of specimens obtained during clean orthopaedic operations. J Bone Joint Surg Am. 1991; 73(8):1200–1207.

21. Ahn DK, Park HS, Kim TW, et al. The degree of bacterial contamination while performing spine surgery. Asian Spine J. 2013; 7(1):8–13.





 PDF
PDF ePub
ePub Citation
Citation Print
Print



 XML Download
XML Download