Abstract
Background
To report the radiological and clinical results after corrective osteotomy in ankylosing spondylitis patients. Furthermore, this study intended to classify the types of deformity and to suggest appropriate surgical treatment options.
Methods
We retrospectively analyzed ankylosing spondylitis patients who underwent corrective osteotomy between 1996 and 2009. The radiographic assessments included the sagittal vertical axis (SVA), spinopelvic alignment parameters, correction angle, correction loss, type of deformity related to the location of the apex, and the craniocervical range of motion (CCROM). The clinical outcomes were assessed by the Oswestry Disability Index (ODI) scores.
Results
A total of 292 corrective osteotomies were performed in 248 patients with a mean follow-up of 40.1 months (range, 24 to 78 months). There were 183 cases of single pedicle subtraction osteotomy (PSO), 19 cases of multiple Smith-Petersen osteotomy (SPO), 17 cases of PSO + SPO, 14 cases of single SPO, six cases of posterior vertebral column resection (PVCR), five cases of PSO + partial pedicle subtraction osteotomy (PPSO), and four cases of PPSO. The mean correction angles were 31.9° ± 11.7° with PSO, 14.3° ± 8.4° with SPO, 38.3° ± 12.7° with PVCR, and 19.3° ± 7.1° with PPSO. The thoracolumbar type was the most common. The outcome analysis showed a significant improvement in the ODI score (p < 0.05). Statistical analysis revealed that the ODI score improvements correlated significantly with the postoperative SVA and CCROM (p < 0.05). There was no correlation between the clinical outcomes and spinopelvic parameters. There were 38 surgery-related complications in 25 patients (10.1%).
Ankylosing spondylitis is a chronic inflammation that results in progressive ossification of the ligaments and joints of the spine. Pain and stiffness are the hallmarks of this disease especially in the axial skeleton and these symptoms progress upwards. Eventually, the spine becomes stiff and global kyphosis becomes fixed due to loss of lumbar lordosis and increased thoracic kyphosis. Back pain occurs due to the global positive balance and horizontal gaze becomes difficult as the disease progresses. Because of these combined reasons, normal social activities are affected. The major concerns are stiffness (90%), pain (83%), fatigue (62%), poor sleep (54%), and concerns about cosmetic appearance (50%).1) A corrective osteotomy is a widely accepted solution for fixed kyphotic deformity.23) The purpose of surgery is to correct the posture, reduce other discomforts caused by poor posture, increase social activities, and improve respiratory and digestive functions. Several reports have shown acceptable and good clinical outcomes after various types of corrective osteotomy.456) Hehne et al.7) reported good outcomes of corrective osteotomy applied in ankylosing spondylitis patient. To the best of our knowledge, there has been no report that has classified the types of deformity and analyzed the specific factors affecting clinical outcomes in ankylosing spondylitis patients.
In this study, the radiological and clinical outcomes for various types of osteotomy have been analyzed, followed by the analysis of specific factors associated with the clinical outcomes. Furthermore, the types of deformity have been classified and appropriate surgical treatment options based on our experiences have been suggested.
All selected patients had a fixed global sagittal imbalance on the lateral image of the whole spine (sagittal vertical axis [SVA] more than 70 mm) and they had symptoms such as a disturbed horizontal gaze and difficulty in daily activities. The indications for surgery in all cases were inability to stand upright in a balanced alignment, inability to maintain a horizontal gaze, compression of the viscera due to kyphosis, pain due to muscle strain, and poor cosmetic appearance.
Among a total of 279 patients who underwent corrective osteotomy from 1996 to 2009, follow-up data were available for 248 patients. The identification and examinations were performed based on the medical records, and radiographs of 248 patients who were followed up for more than 2 years postoperatively were obtained. All operations were performed by the first author.
Among the 248 patients, 227 were men and 21 were women, and their average age was 37.6 years (range, 24 to 65 years). The mean postoperative follow-up period was 34.2 months (range, 24 to 78 months).
The clinical results were obtained by reviewing the charts in a retrospective manner. The preoperative and final follow-up Oswestry Disability Index (ODI) scores were obtained and analyzed.
The radiographic assessment was performed with standing lateral radiography of the whole spine prior to the operation, immediately after the operation, and 2 years after the operation. The radiograms were standardized by full extension of hips and knees and both fists gently placed on the clavicles with elbow flexion.89)
The radiological apex was defined as the farthest vertebrae from the line between the C2 vertebral body center and the midpoint of the upper sacral endplate. Based on this definition, kyphosis was classified into cervicothoracic (C1-T3), midthoracic (T4-T9), thoracolumbar (T10-L2), and lumbar (below L3) types according to the location of the apex (Fig. 1). The correction angle was defined as the angle between the superior end plate of the level above the osteotomy and the inferior end plate of the level below the osteotomy before and after the osteotomy. Several spinopelvic parameters were checked: SVA-the distance between the posterosuperior corners of the sacrum (PSCS) after drawing a perpendicular line from the C7 vertebral body center to the ground, thoracic kyphosis (TK)-the Cobb angle from T4 to T12, lumbar lordosis (LL)-the Cobb angle from L1 to S1, pelvic incidence (PI), pelvic tilt (PT). The craniocervical range of motion (CCROM) was devised to measure visual ranges determined by the angle between the posterosuperior tip of the hard palate to the caudal base of the occiput (McGregor line) and the T1 upper end plate on the cervical lateral flexion-extension image (Fig. 2).
SPSS ver. 12.0 (SPSS Inc., Chicago, IL, USA) was used for the statistical analyses in this study. The correlations between clinical outcomes according to the SVA and CCROM were analyzed using analysis of variance and the paired t-test. Multivariate logistic regression analysis was performed to evaluate the correlation between several spinopelvic parameters and good clinical outcomes. A p-value less than 0.05 was considered to be statistically significant. The cut-off values of SVA, CCROM, and ODI were determined by the receiver operating characteristic curve.
A total of 292 corrective osteotomies were performed in 248 patients. Among the patients, 207 underwent a single corrective osteotomy: pedicle subtraction osteotomy (PSO, 183), Smith-Petersen osteotomy (SPO, 14), posterior vertebral column resection (PVCR, 6), and partial pedicle subtraction osteotomy (PPSO, 4). Forty-one patients had a combined osteotomy (multiple SPO, 19; SPO + PSO, 17; PSO + PPSO, 5) (Table 1).
On classifying the patients according to the location of the apex, there were 2 patients with the cervicothoracic type (1%), 52 patients with the midthoracic type (21%), 177 patients with the thoracolumbar type (71%), and 17 patients with the lumbar type (7%).
The average CCROM was 27.3° (range, 0° to 64°), and 76 patients (31%) showed no evidence of cervical spine ankylosis. In addition, 141 patients (56%) showed ankylosis in the subaxial area, and 31 patients (13%) showed ankylosis in the C0-1-2 area.
Overall, 207 single osteotomy cases were analyzed to assess the correction angles according to the type of osteotomy. The average correction angles for the various types of osteotomy are summarized in Table 2. The radiological assessment of sagittal balance parameters before and after surgery is summarized in Table 3. Twenty-two patients (9%) had negative SVA values, showing a negative sagittal balance. The average SVA at 2 years postsurgery was 84.2 mm (range, -32 to 189 mm). Among the 22 patients who showed a negative sagittal balance immediately after the surgery, 15 patients continued to have a negative sagittal balance even after 2 years.
The average ODI score prior to surgery was 44.5% ± 2.7%, and it was reduced to 20.8% ± 2.1% after surgery at the final follow-up. This difference was statistically significant (p = 0.01).
To evaluate the relationship between the postoperative SVA and clinical outcome, the patients were classified into the following 3 groups: A group (SVA less than 70 mm postsurgery, n = 165), B group (SVA greater than 70 mm, n = 61), and C group (negative sagittal balance, n = 22). The A group showed the best clinical outcomes, followed by the B and C groups in that order. The A group (mean ODI, 17.4 ± 8.2) showed a significant difference compared with the B (mean ODI, 23.7.4 ± 4.2) and C (mean ODI, 28.7 ± 3.4) groups (p = 0.01, p = 0.01), but there was no significant difference between the B and C groups (p = 0.42).
Additionally, the patients with CCROM greater than 30° (mean ODI, 21.7° ± 7.1°) showed better clinical outcomes compared with the patients with CCROM less than 30° (mean ODI, 26.7° ± 4.7°). There was also a significant difference between the two groups (p = 0.01).
To evaluate the relationship between the spinopelvic parameters and clinical outcome, the patients were classified into 2 groups: good clinical outcome group (ODI less than 20) and bad clinical outcome group (ODI more than 20). Based on the multivariate regression analysis, there were no significant correlations between the outcome and pelvic parameters such as PI and PT (p = 0.46, p = 0.62). Also, there were no significant correlations with spinal parameters such as LL and TK (p = 0.34, p = 0.42).
A total of 38 complications were reported in 25 patients (10.1%) (Table 4). Dural tear was the most commonly reported complication, occurring in 20 cases. Thirteen cases showed a dural defect that could not be repaired directly. Dural defects secondary to adhesive lesions between the dura and the ligamentum flavum, facet, or lamina were more prevalent in ankylosing spondylitis patients. These defects were managed by closure with patching or a localized fat graft. If there was continuous cerebrospinal fluid leakage or a pseudomeningocele, a lumbar drain was inserted. In 3 cases, the dural tear was not effectively managed and revision surgery was necessary.
There were 2 cases of transient myelopathy. One case showed abnormal reflex, increased deep tendon reflex, and reduced muscle strength of the left knee extensor after the T12 PSO. A bony fragment was found on a computed tomography scan, which was removed on the following day after the operation. The reduced muscle strength of the left knee extensor was restored and the patient was able to ambulate after 3 months. The other patient developed paraplegia post PVCR at L1. Neural exploration was attempted immediately, but definite neural compressive lesions were not identified. Despite the absence of lesions, decompression surgery was performed and the patient showed improvement on the following day. In this case, no definite cause was identified but cord ischemia or distraction was assumed to be the cause.10)
There were 6 cases of transient radiculopathy including 4 cases of unilateral hip flexor weakness and 2 cases of unilateral knee extensor weakness. All 6 cases recovered to better than motor grade IV after 6 months.
There was one case of permanent visual loss. This complication was thought to be caused by inappropriate eye protection and padding during the lengthy operation in the prone position. Ischemic optic neuropathy, retinal artery occlusion, and cerebral ischemia were also considered to be the possible causes.11) There was a case of transient visual loss, but the patient's vision returned to normal at 7 days postoperation.
A corrective osteotomy is the widely accepted solution for rigid and fixed kyphotic deformities in ankylosing spondylitis patients. Various types of osteotomy, such as SPO, PSO, PVCR, and PPSO, could be applied to correct the deformity.12) Each type of osteotomy has different features including the range of the correction angle, potential risks, and suitable indications. To determine the most appropriate osteotomy, the following factors should be considered: the amount of correction, type of deformity, location of the apex, fusion levels, surgical risks, predictable complications, and postoperative functional outcomes. It is difficult to suggest uniform guidelines because the type of deformity, the location of the apex, and the severity of kyphosis vary greatly among individuals.
Determining the amount of correction needed is the first step in a corrective osteotomy. There are several methods to calculate the correction angle. A correction angle can be determined by using a X-ray film of a broken bone, but this method is cumbersome and difficult to use for obtaining the accurate angle.13) The reproducibility and reliability of such practices has not been documented in the peer-reviewed literature. van Royen et al.14) devised ASKyphoplan computer program to determine the correction angle. However, this program can occasionally be difficult to use and researchers may be unfamiliar with its use. Ondra et al.15) reported that the tangent method can simply and accurately measure the correction angle.
Van Royen et al.16) reported that the ideal center of gravity of the trunk is located above the femoral head and postoperative SVA ranges from 50 to 100 mm, although the optimal SVA postsurgery is unknown. Kim et al.17) reported that outcomes in patients with fixed sagittal imbalance, after excluding ankylosing spondylitis patients who underwent PSO, were statistically significantly poor when the SVA was 80 mm or greater. Schwab et al.18) reported that postoperative SVA of more than 100 mm could be considered as failed realignment. In this study, the patients with an SVA of less than 70 mm postsurgery showed the best clinical outcome.
In addition, the location of the osteotomy is important. Theoretically, the more distal is the osteotomy, the more is the correction achieved in the C7 plumb line. However, instrumentation extension caudal to the osteotomy area in the lower lumbar spine can be insufficient. As far as the authors are concerned, the location of the osteotomy at the apex is best for effective SVA correction per correction angle and for improving the overall cosmetic alignment. In this study, the deformity types were classified according the location of the apex, and the thoracolumbar type was found to be the most common.
Another important consideration is determining the type of osteotomy. SPO can achieve correction by removing the posterior elements with an anterior opening, but it can be challenging if the anterior longitudinal ligament (ALL) is fully ossified. In addition, coronal imbalance correction is difficult, and there is a risk of devastating complications, such as great vessel injury. In contrast to SPO, PSO can be performed even if the ALL is fully ossified, and coronal imbalance correction can be achieved by the asymmetric posterior closing wedge. However, this method carries risks of neurologic injury at the thoracic level and more blood loss. PPSO is the procedure that could be a solution for the gray zone between SPO and PSO, and it is less invasive than PSO. PVCR can achieve a greater correction angle and coronal imbalance correction, but it can lead to instability due to the resection of all three columns and may cause vertebral column translation.
Another important consideration is the CCROM. While performing the correction, one of the most important things is the field of view in everyday life and preservation of a horizontal gaze. There was a significant correlation between a CCROM greater than 30° and improved clinical outcomes in this study. If there is any movement at the craniocervical portion despite the severe global kyphotic deformity, the required daily field of view can be obtained. In the cases with more than 30° of CCROM, the operators will have more flexibility in determining the amount of correction, but if not, the amount of correction must be mitigated. As mentioned above, overcorrection must be avoided if there is severe cervical ankylosis. But, the CCROM was not changed by the operation and it is solely a patient factor.
Recently, the concept of spinopelvic alignment has gained importance in sagittal balance.1718192021) Many studies have reported on pelvic parameters and postoperative outcomes as well as spinal alignment. To sum it up, amounts of pelvic incidence and changes in the pelvic tilt significantly influence the postoperative outcomes. In this study, the changes in pelvic parameters did not have a direct correlation with changes in postoperative outcomes. The patients with ankylosing spondylitis exhibited completely fixed spinopelvic alignment from the sacroiliac joint to the cranial direction (at least to the thoracic level). When correction was performed at the thoracic or lumbar level in these patients, the angles changed in the relevant segments and compensation did not occur at the spinal or pelvic level. Thoracic level osteotomy does not change the amount of lumbar lordosis, and lumbar osteotomy does not lead to thoracic compensation. Appropriate realignment means locating the head on the pelvis, recovering the gaze level, and making standing and walking ergonomically efficient. According to the results of the present study in patients with fully fixed kyphosis, postoperative SVA and CCROM were more important than spinopelvic alignment.
Naturally, there have been learning curves in surgical procedures and surgical technique modifications over the past 13 years. Nonetheless, there has been no great change in types of basic osteotomy (SPO, PSO, and PVCR). PPSO was introduced 5 years ago. Initially, we mainly performed SPO because of its low risk of neurologic deficits. However, in recent years, due to the characteristics of ankylosing spondylitis where the ALL is ossified, we have mostly performed posterior closing osteotomy such as PSO or PPSO. For fixation, we have used a pedicle screw. Basically, fixation was performed 3 levels above and 3 levels below. Manual reduction after osteotomy was performed after the table was hyperextended into a V shape or cranial and caudal parts were anchored with a towel clip. The reduction was performed slowly and sequentially on both sides using a compressor.
On the basis of our experience, in the midthoracic area, multiple SPO is ideal for global, round, homogenous kyphosis. Usually, SPO will accomplish approximately 10° of correction and PPSO can achieve up to 15° of correction at the thoracic level. PVCR is more appropriate if a correction angle of greater than 40° is required or if the coronal imbalance is severe. Special caution must be taken because the midthoracic area is associated with the highest risk of neurologic injury and it is safe to perform the osteotomy below the cord level even if the apex is located in the midthoracic area.
The thoracolumbar type is the most common type. It is relatively safe to perform an osteotomy at L2 (below the cauda equina level) and instrumentation can be extended through the upper and lower 3 levels. A PSO at L2 is the most appropriate if the correction angle is approximately 30°, and PVCR, PSO + SPO, or PSO + PPSO can be considered if the correction angle is approximately 40°-45°.
Summarizing the results of this study, correction can be achieved up to 15° by SPO, up to 30° by PSO, up to 40° by PVCR, and up to 20° by PPSO. The postsurgery clinical outcomes were significantly improved. The postoperative SVA and CCROM showed a significant correlation with the clinical outcomes. The deformity types were classified according to the location of the apex, and surgical treatment options can be suggested based on our experience (Table 5).
Corrective osteotomy is an effective method for treating a fixed kyphotic deformity occurring in ankylosing spondylitis, which can achieve satisfactory outcomes with acceptable complications. Treatment options according to the deformity type should be chosen after determining the optimal correction angle and after understanding the specific features of each osteotomy.
According to the results of this study, achieving a SVA of less than 70 mm postsurgery is the most basic condition and the CCROM could be an important patient factor for a good clinical outcome.
Figures and Tables
Table 1
Summary of 292 Corrective Osteotomies
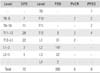
| Level | SPO | Level | PSO | PVCR | PPSO |
|---|---|---|---|---|---|
| - | - | T9 | - | 1 | |
| T8-9 | 7 | T10 | - | 2 | 2 |
| T9-10 | 11 | T11 | - | - | 2 |
| T11-12 | 28 | T12 | 3 | 2 | 4 |
| T12-L1 | 22 | L1 | 31 | 2 | - |
| L1-2 | 3 | L2 | 147 | - | - |
| L2-3 | 1 | L3 | 22 | - | - |
| - | - | L4 | 2 | - | - |
| Total | 72 | 205 | 6 | 9 |
Table 2
Changes in the Correction Angle with Each Single Osteotomy
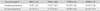
Table 3
Radiological Assessment of Sagittal Balance Parameters before and after Surgery
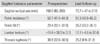
Table 4
Summary of Directly Surgery-Related Complications

| Type of complication | No. |
|---|---|
| Dural tear | 20 |
| Transient myelopathy | 2 |
| Transient radiculopathy | 6 |
| Infection | 5 |
| Permanent visual loss | 1 |
| Transient visual loss | 1 |
| Junctional kyphosis | 2 |
| Coronal imbalance | 1 |
References
1. Ward MM. Health-related quality of life in ankylosing spondylitis: a survey of 175 patients. Arthritis Care Res. 1999; 12(4):247–255.

2. Goel MK. Vertebral osteotomy for correction of fixed flexion deformity of the spine. J Bone Joint Surg Am. 1968; 50(2):287–294.

3. Thiranont N, Netrawichien P. Transpedicular decancellation closed wedge vertebral osteotomy for treatment of fixed flexion deformity of spine in ankylosing spondylitis. Spine (Phila Pa 1976). 1993; 18(16):2517–2522.

4. Berven SH, Deviren V, Smith JA, Emami A, Hu SS, Bradford DS. Management of fixed sagittal plane deformity: results of the transpedicular wedge resection osteotomy. Spine (Phila Pa 1976). 2001; 26(18):2036–2043.
5. Kim KT, Suk KS, Cho YJ, Hong GP, Park BJ. Clinical outcome results of pedicle subtraction osteotomy in ankylosing spondylitis with kyphotic deformity. Spine (Phila Pa 1976). 2002; 27(6):612–618.

6. Chang KW, Chen YY, Lin CC, Hsu HL, Pai KC. Closing wedge osteotomy versus opening wedge osteotomy in ankylosing spondylitis with thoracolumbar kyphotic deformity. Spine (Phila Pa 1976). 2005; 30(14):1584–1593.

7. Hehne HJ, Zielke K, Bohm H. Polysegmental lumbar osteotomies and transpedicled fixation for correction of long-curved kyphotic deformities in ankylosing spondylitis: report on 177 cases. Clin Orthop Relat Res. 1990; (258):49–55.
8. Kim WJ. Optimal Standing Radiographic Positioning in Patients with Sagittal Imbalance. J Korean Soc Spine Surg. 2010; 17(4):198–204.

9. O'Brien MF, Kuklo TR, Blanke KM, Lenke LG. Radiographic measurement manual. Memphis, TN: Medtronic Sofamor Danek;2008.
10. Kim KT, Lee SH, Kwack YH, Son ES. Is it real false negative finding in motor evoked potential monitoring during corrective surgery of ankylosing spondylitis? A case report. Asian Spine J. 2012; 6(1):50–54.

12. Kim KT, Park DH, Lee SH, Suk KS, Lee JH, Park KJ. Partial pedicle subtraction osteotomy as an alternative option for spinal sagittal deformity correction. Spine (Phila Pa 1976). 2013; 38(14):1238–1243.

13. Booth KC, Bridwell KH, Lenke LG, Baldus CR, Blanke KM. Complications and predictive factors for the successful treatment of flatback deformity (fixed sagittal imbalance). Spine (Phila Pa 1976). 1999; 24(16):1712–1720.

14. van Royen BJ, Scheerder FJ, Jansen E, Smit TH. ASKyphoplan: a program for deformity planning in ankylosing spondylitis. Eur Spine J. 2007; 16(9):1445–1449.

15. Ondra SL, Marzouk S, Koski T, Silva F, Salehi S. Mathematical calculation of pedicle subtraction osteotomy size to allow precision correction of fixed sagittal deformity. Spine (Phila Pa 1976). 2006; 31(25):E973–E979.

16. Van Royen BJ, De Gast A, Smit TH. Deformity planning for sagittal plane corrective osteotomies of the spine in ankylosing spondylitis. Eur Spine J. 2000; 9(6):492–498.

17. Kim YJ, Bridwell KH, Lenke LG, Cheh G, Baldus C. Results of lumbar pedicle subtraction osteotomies for fixed sagittal imbalance: a minimum 5-year follow-up study. Spine (Phila Pa 1976). 2007; 32(20):2189–2197.

18. Schwab FJ, Patel A, Shaffrey CI, et al. Sagittal realignment failures following pedicle subtraction osteotomy surgery: are we doing enough? Clinical article. J Neurosurg Spine. 2012; 16(6):539–546.

19. Schwab F, Lafage V, Patel A, Farcy JP. Sagittal plane considerations and the pelvis in the adult patient. Spine (Phila Pa 1976). 2009; 34(17):1828–1833.

20. Yang BP, Ondra SL, Chen LA, Jung HS, Koski TR, Salehi SA. Clinical and radiographic outcomes of thoracic and lumbar pedicle subtraction osteotomy for fixed sagittal imbalance. J Neurosurg Spine. 2006; 5(1):9–17.

21. Schwab F, Patel A, Ungar B, Farcy JP, Lafage V. Adult spinal deformity-postoperative standing imbalance: how much can you tolerate? An overview of key parameters in assessing alignment and planning corrective surgery. Spine (Phila Pa 1976). 2010; 35(25):2224–2231.




 PDF
PDF ePub
ePub Citation
Citation Print
Print





 XML Download
XML Download