Abstract
Background
The purpose of the current study was to investigate the incidence of preoperative deep vein thrombosis (DVT) after hip fractures in Korea.
Methods
In this prospective study, we enrolled 152 Korean geriatric patients who had suffered hip fractures due to a simple fall and were hospitalized between January 2013 and December 2013. There were 52 male and 100 female patients, and their mean age was 78.2 years. There were 96 trochanteric fractures and 56 femoral neck fractures. All patients were examined for DVT: 26 by ultrasonography and 126 by computed tomography venography. The patients having DVT underwent inferior vena cava filter insertion before the surgical intervention.
Results
Preoperatively, none of the patients had any signs or symptoms of DVT; however, 4 patients were identified as having asymptomatic DVT. The overall incidence of DVT was 2.6% (4/152). The mean time to arrival at emergency room after injury was 32.6 hours. Mean time elapsed to undergo surgery after hospitalization was 24.9 hours. The average time to hospitalization after injury was 237 hours for patients with DVT versus 27.5 hours for patients without DVT. DVT developed within 72 hours in two of the 137 patients (1.4%) and after 72 hours in two of the remaining 15 patients (13.3%) hospitalized.
Conclusions
While the preoperative incidence of DVT after hip fractures was relatively low (2.6%) in the Korean geriatric population, we confirmed that getting no treatment within 72 hours after injury increased the incidence of DVT. Thus, we conclude from this study that a workup for DVT should be considered in cases where admission or surgery has been delayed for more than 72 hours after injury.
Deep vein thrombosis (DVT) and pulmonary embolism (PE) are the major causes of mortality and morbidity in elderly patients who have undergone a hip fracture surgery.1) Hip fracture patients exhibit all three risk factors associated with Virchow's triad because of the trauma itself, immobilization, advanced age, and comorbidity. Notably, surgery later than 24 hours after injury increased death due to complications of PE.1) Nowadays, several guidelines recommend mechanical and pharmaceutical prophylaxis for hip fracture patients, depending on the risk and benefits involved.234) Despite these efforts, preoperative DVT is known to occur in 9% to 62% of patients receiving prophylaxis.56) Till date, there was only one study in Korea to document the preoperative prevalence of DVT in hip fracture patients at the time of admission to the hospital.7)
The purpose of the present study was to establish the preoperative prevalence of DVT in patients who had a fracture around the hip, and to determine what factors might have influenced this prevalence. Specifically, we examined the correlation between the delay in admission from the time of injury to the development of DVT.
In this prospective study, 195 hip fractures were treated between January 2013 and December 2013. Exclusion criteria were as follow: less than 60 years of age (2 patients), high energy injuries (13 patients), pathologic fractures (2 patients), fractures around implant (7 patients), atypical femoral fractures (15 patients), patients who could not measure onset time of injury (4 patients). As a result, we finally enrolled 152 Korean geriatric patients who had been admitted to Daegu Fatima Hospital, after suffering from hip fractures due to a simple fall. There were 100 female and 52 male patients. The mean age was 78.2 years (range, 60 to 96 years). There were 96 trochanteric fractures and 56 femoral neck fractures. Closed reduction and intramedullary nail fixation was done for all 96 trochanteric fractures, cannulated screw fixation for 3 non-displaced and valgus impacted femoral neck fractures, and bipolar hemiarthroplasty for 53 displaced neck fractures.
The lower extremities were examined for signs and symptoms of DVT (i.e., tenderness, warmth, erythema, edema, and pain with sudden ankle dorsiflexion). Evaluation of the lower extremity venous status was done by ultrasonography (26 patients) and computed tomography (CT) venography (126 patients). After confirming the absence of DVT, intermittent pneumatic compression devices were applied for all patients to prevent the development of DVT. If a DVT was identified, patients underwent insertion of an inferior vena cava (IVC) filter, which was performed by an interventional radiologist.
Chi-square t-test was used for the analysis of categorical data in case of nonparametric techniques. For all tests, p < 0.05 was considered statistically significant. All analyses were performed using the IBM SPSS ver. 21.0 (IBM Co., Armonk, NY, USA).
The mean time to arrival at the emergency room after injury was 32.6 hours (range, 1 to 576 hours) for all patients, 237 hours (range, 4 to 576 hours) for DVT group, and 27.5 hours (range, 1 to 312 hours) for non-DVT group (p < 0.001). Mean time to undergo surgery after hospitalization was 24.9 hours (range, 4 to 254 hours) for all patients, 20.8 hours (range, 7 to 49 hours) for DVT group, and 27.1 hours (range, 4 to 254 hours) for non-DVT group (p > 0.05).
None of these patients had a previous history of DVT. Preoperative DVT was detected in 4/152 patients (2.6%). Mean age of DVT and non-DVT groups was 80.7 years (range, 74 to 91 years) and 77.4 years (range, 61 to 96 years), respectively (p > 0.05). The incidence of preoperative DVT was 0%, 2.6%, 2.6%, and 7.7%, respectively, in sexagenarian, septuagenarian, octogenarian, and nonagenarian patients. There were no statistically significant differences among age groups, though the incidence was slightly higher in nonagenarian patients. DVT developed in 1/52 (1.9%) in male patients, 3/100 (3%) in female patients, 1/56 (1.7%) in femoral neck fracture patients, and 3/96 (3.1%) in trochanteric fracture patients. Although the preoperative incidence of DVT was slightly higher in females and trochanteric fracture patients, we couldn't find any statistical significance between male and female, or neck and trochanter fractures, respectively (p > 0.05). Hence, there were no significant differences between the mean age, age group, sex distribution, fracture type, and previous history of thromboembolism, between the patients who had documented DVT on admission and those who did not (p > 0.05) (Table 1).
The incidence of preoperative DVT was calculated according to the time between the fracture and the time of admission to the hospital. Of the total 152 patients, 137 patients (90%) were seen at the hospital within 72 hours after hip fractures: 2/137 patients (1.4%) had documented DVT, diagnosed as popliteal thrombi in both cases. One patient had DVT on the ipsilateral side and the other patient had thrombi on both sides. Both these patients had a fracture of the trochanter and were treated with intramedullary nail. The remaining 15 patients (10%) arrived 72 hours after getting the fracture. DVT was confirmed in 2/15 patients (13.3%). One of these patients had femoral thrombus with trochanteric fracture, and the other had popliteal thrombus with a fracture of the neck (Table 2). Based on the time of admission, the difference in the prevalence of DVT was significant at 72 hours after injury (p < 0.05). Once the patients were optimized for surgery, all 4 patients who had a DVT underwent surgery without further delay, after an IVC filter was inserted by an interventional radiologist. These patients received warfarin for 3 months, aiming for international normalized ratio of 2 to 2.5.
Venous thromboembolism is a major problem after hip fracture. We can anticipate the development of DVT in the interval between the time of hip fracture and surgery, because hip fracture patients cannot move an injured extremity during this period, while patients undergoing total joint arthroplasty are mobile before the surgery.
There are many studies regarding the incidence and treatment of postoperative thromboembolism related to major orthopaedic surgeries.891011) The current study focused on the preoperative development of DVT. We took an interest in preoperative DVT in hip fractures, since this is caused due to time delay before surgery. Any delay in surgical treatment for a hip fracture can be caused by numerous factors, which range from the time required to stabilize a patient's medical condition to the availability of operating rooms. Regardless of the cause, surgical delay increases the preoperative immobilization, which is one of the most important factors in the development of DVT. It has been recommended that thromboprophylaxis with low-molecular-weight heparin or low-dose unfractionated heparin be initiated during the time between hospital admission and surgery. For patients undergoing hip fracture surgery who have a high risk of bleeding, the optimal use of mechanical thromboprophylaxis is recommended.3) In spite of these efforts, preoperative DVT is known to occur in as high as 9% to 62% of patients receiving prophylaxis.56) During mechanical prophylaxis and surgery, there is a risk of detachment and proximal propagation of thrombi that is already formed due to vigorous manipulation of the injured extremity.12) Such an event could lead to legal problems. Thus, it is imperative that we should know whether the patient has preoperative DVT or not.
In our study, the overall incidence of DVT was low (2.6%). Our data is similar to previous results of Asian countries.1314) However, patients for whom the admission was delayed by more than 72 hours after injury had a higher prevalence of DVT (2/15) than those who were seen within 72 hours after the fracture (2/137). This result is partially similar to that of Western countries.61516) We believe this could be due to an increased life expectancy, and the transitional process of eastern lifestyle getting westernized (such as a dietary shift towards animal proteins and fatty food). This transitional process is well documented in two multicenter Asian reports.1718)
Gender (females), nonagenarian patients, trochanteric fracture and time from injury to admission are proven risk factors for the development of preoperative DVT. Among these risk factors, we found only the time from injury to admission to be a statistically significant factor for development of DVT, in the current study.
We employed CT venography and ultrasonography to diagnose DVT. They showed similar results in diagnosing or excluding DVT.19) We used an ultrasonography in cases of patients where injection of contrast media is too troublesome due to high creatinine levels.
Insertion of IVC filter, for the treatment of DVT in a hip fracture patient, is controversial. The clear indications for venous interruption in patients with DVT are anticoagulant-induced bleeding, or anticipation of hemorrhagic complications in a patient with a predisposing lesion and failure of anticoagulation.20) Some people may think our treatment is excessive. But all 4 cases of our series were proximal DVT above the popliteal vein. Proximal DVT has more chances to cause fatal PE than distal DVT, especially during the operative procedure. Langan et al.21) reported that prophylactic IVC filters can be placed safely in trauma patients at high risk, with low morbidity and no attributable long-term disabilities. Smith et al.16) also used IVC filter for patients who had DVT preoperatively. All 4 patients who had a preoperative DVT underwent insertion of an IVC filter before surgery. None of these patients experienced complications related to the filter insertion and thromboembolism. Most orthopedic surgeons would want to operate on these patients immediately. In such situations, the surgeon does not wait for the resolution of the thrombi with medial therapy of anticoagulation. We thought an insertion of IVC filter is a safe and reasonable approach for hip fracture patients having DVT preoperatively; however, it needs to be confirmed by a well-designed, randomized, and controlled study.
In summary, though the incidence of preoperative DVT is low in patients with fracture about the hip in Korea, we should consider vascular evaluation for acute hip fractures to exclude the presence of asymptomatic DVT, especially in patients who arrive at the hospital more than 72 hours after the injury. Also, aggressive treatment like the insertion of IVC filter should be considered for patients presenting with preoperative DVT.
Figures and Tables
Table 1
Basic Demographic Data of Patients
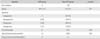
Table 2
Incidence of Preoperative Deep Vein Thrombosis according to the Time of Admission to the Hospital

| Variable | Time of admission (hr) | p-value | |
|---|---|---|---|
| Within 72 | After 72 | ||
| Total no. of patients | 137 | 15 | - |
| Popliteal thrombus | 2 | 1 | - |
| Femoral thrombus | 0 | 1 | - |
| Total no. of deep vein thromboses (%) | 2 (1.4) | 2 (13.3) | 0.01 |
References
1. Perez JV, Warwick DJ, Case CP, Bannister GC. Death after proximal femoral fracture: an autopsy study. Injury. 1995; 26(4):237–240.
2. Park YS. Guideline for the prophylaxis of venous thromboembolism in hip surgery patients. J Korean Orthop Assoc. 2011; 46(2):95–98.
3. Geerts WH, Bergqvist D, Pineo GF, et al. Prevention of venous thromboembolism: American College of Chest Physicians Evidence-Based Clinical Practice Guidelines (8th Edition). Chest. 2008; 133:6 Suppl. 381S–453S.
4. National Institute for Health and Clinical Excellence. Venous thromboembolism in adults admitted to hospital: reducing the risk [Internet]. London: National Institute for Health and Clinical Excellence;2015. cited 2015 Jun 14. Available from: http://www.nice.org.uk/guidance/cg92.
5. Salzman EW, Harris WH. Prevention of venous thromboembolism in orthopaedic patients. J Bone Joint Surg Am. 1976; 58(7):903–913.
6. Zahn HR, Skinner JA, Porteous MJ. The preoperative prevalence of deep vein thrombosis in patients with femoral neck fractures and delayed operation. Injury. 1999; 30(9):605–607.
7. Jung JH, Lee KJ, Min BW, Son ES, Koo TW. Incidence of deep vein thrombosis before hip fracture surgery diagnosed by color doppler sonography surveillance. J Korean Orthop Ultrasound Soc. 2014; 7(2):98–104.
8. Powers PJ, Gent M, Jay RM, et al. A randomized trial of less intense postoperative warfarin or aspirin therapy in the prevention of venous thromboembolism after surgery for fractured hip. Arch Intern Med. 1989; 149(4):771–774.
9. Calfon M, Seddighzadeh A, Piazza G, Goldhaber SZ. Deep vein thrombosis in orthopedic surgery. Clin Appl Thromb Hemost. 2009; 15(5):512–516.
10. Clayton RA, Gaston P, Watts AC, Howie CR. Thromboembolic disease after total knee replacement: experience of 5100 cases. Knee. 2009; 16(1):18–21.
11. Samama CM, Ravaud P, Parent F, Barre J, Mertl P, Mismetti P. Epidemiology of venous thromboembolism after lower limb arthroplasty: the FOTO study. J Thromb Haemost. 2007; 5(12):2360–2367.
12. Monreal M, Ruiz J, Olazabal A, Arias A, Roca J. Deep venous thrombosis and the risk of pulmonary embolism: a systematic study. Chest. 1992; 102(3):677–681.
13. Mitra AK, Khoo TK, Ngan CC. Deep-vein thrombosis following hip surgery for fracture of the proximal femur. Singapore Med J. 1989; 30(6):530–534.
14. Chan YK, Chiu KY, Cheng SW, Ho P. The incidence of deep vein thrombosis in elderly Chinese suffering hip fracture is low without prophylaxis: a prospective study using serial duplex ultrasound. J Orthop Surg (Hong Kong). 2004; 12(2):178–183.
15. Hefley FG Jr, Nelson CL, Puskarich-May CL. Effect of delayed admission to the hospital on the preoperative prevalence of deep-vein thrombosis associated with fractures about the hip. J Bone Joint Surg Am. 1996; 78(4):581–583.
16. Smith EB, Parvizi J, Purtill JJ. Delayed surgery for patients with femur and hip fractures-risk of deep venous thrombosis. J Trauma. 2011; 70(6):E113–E116.
17. Leizorovicz A, Turpie AG, Cohen AT, Wong L, Yoo MC, Dans A. Epidemiology of venous thromboembolism in Asian patients undergoing major orthopedic surgery without thromboprophylaxis: the SMART study. J Thromb Haemost. 2005; 3(1):28–34.
18. Piovella F, Wang CJ, Lu H, et al. Deep-vein thrombosis rates after major orthopedic surgery in Asia: an epidemiological study based on postoperative screening with centrally adjudicated bilateral venography. J Thromb Haemost. 2005; 3(12):2664–2670.
19. Goodman LR, Stein PD, Matta F, et al. CT venography and compression sonography are diagnostically equivalent: data from PIOPED II. AJR Am J Roentgenol. 2007; 189(5):1071–1076.
20. Hirsh J, Hoak J. Management of deep vein thrombosis and pulmonary embolism: a statement for healthcare professionals: Council on Thrombosis (in consultation with the Council on Cardiovascular Radiology), American Heart Association. Circulation. 1996; 93(12):2212–2245.
21. Langan EM 3rd, Miller RS, Casey WJ 3rd, Carsten CG 3rd, Graham RM, Taylor SM. Prophylactic inferior vena cava filters in trauma patients at high risk: follow-up examination and risk/benefit assessment. J Vasc Surg. 1999; 30(3):484–488.




 PDF
PDF ePub
ePub Citation
Citation Print
Print


 XML Download
XML Download