Abstract
Background
We analyzed the extent of the comminution in the acetabular weight-bearing area, the clinical and radiographic results, and the complications after a minimum 2-year follow-up of the modified Stoppa approach for the treatment of acetabular fractures, and we attempted to evaluate the efficacy of the operative technique.
Methods
All of the 22 patients, who needed the anterior approach for the treatment of acetabular fractures at our hospital from November 2007 to November 2010, were subjected to surgery via the modified Stoppa approach. Fracture pattern, operative time, blood loss during the operation, quality of reduction, number of bony fragments in the acetabular weight-bearing area, and postoperative complications were assessed by retrospectively analyzing the medical records and the radiographic examinations. The results after the operation were analyzed based on the criteria of Matta.
Results
The clinical results were excellent in 3 cases, good in 13 cases, and poor in 4 cases, while the radiographic results were excellent in 5 cases, good in 13 cases, and poor in 2 cases. Although the quality of reduction and the clinical results according to the extent of comminution were statistically significant (p = 0.03 and p = 0.04, respectively), the radiographic results were not statistically significant (p = 0.74).
Acetabular fracture is an intra-articular fracture of the most important weight-bearing joint, the hip joint, and in order to obtain optimal results, accurate anatomic reduction, firm fixation, and early rehabilitation are essential.1,2,3) However, the treatment of acetabular fractures is quite difficult not only due to the associated major organ injuries but also due to the complicated fracture type and difficulties in the operative approach for reduction. Marked progress has been made after a systematic approach and treatment algorithm were proposed by Judet et al.4) and Letournel and Judet5) in the 1960s.
Until now, diverse surgical approaches have been used for the reduction of acetabular fractures and they are categorized into anterior, posterior, extensile, and combined approaches. The surgeon should become familiar with the technical tips and the advantages and disadvantages of each approach. Currently, the ilioinguinal approach1) or the modified Stoppa approach6,7) is used as the anterior approach, and the ilioinguinal approach is used more commonly and its outcomes have been reported more extensively among these two approaches. The modified Stoppa approach is an intrapelvic approach initially used for inguinal hernia surgery by Rives et al.8) and Stoppa et al.7) in the early 1990's, and was introduced as the method for approaching the anterior acetabulum and pelvic bone by Cole and Bolhofner9) and Hirvensalo et al.10) Short- and long-term results of acetabular fractures using the modified Stoppa approach have not been reported to any meaningful extent until now. Therefore, we aimed to evaluate the efficacy of the operative technique via the modified Stoppa approach by analyzing the results and the complications of acetabular fractures treated with the modified Stoppa approach. Moreover, we evaluated the effect of comminution of fractures on the final results, considering the recent increase in the frequency of comminuted acetabular fractures along with the increase in the cases of high-energy trauma.
A total of 55 patients were treated for acetabular fractures at our hospital from November 2007 to November 2010. Among them, 40 cases underwent the operation. The modified Stoppa approach to the anterior pelvis was used in 22 cases instead of the ilioinguinal approach, which is the most widely used anterior approach. This study retrospectively analyzed 20 patients with a minimum 2-year follow-up among the 22 patients with acetabular fractures who underwent operation via the modified Stoppa approach. The other two patients (1 case of transfer to another hospital in the patient's hometown and 1 case of death due to underlying liver cirrhosis) were excluded from the minimum 2-year analysis of clinical and radiographic results but were included in the analysis of operative time, blood loss, quality of reduction, and perioperative complications. The average follow-up was 2 years and 6 months (range, 2 years to 3 years and 7 months). The average age of the patients, including 16 men and 6 women, was 45 years (range, 20 to 74 years) (Table 1). Traffic accident, in 12 cases (54.5%), was the most frequent cause of injury. The average anesthesia time was 242 minutes (range, 118 to 405 minutes), and the average blood loss was 1,252 mL (range, 320 to 3,850 mL).
Seventeen patients (77.3%) suffered 63 accompanying injuries (Table 2). Among these injuries, fracture in other areas was the most common accompanying injury (28 injuries, 44.4%). Twenty-six other organ injuries (41.3%) were identified including 5 head injuries. Thirteen neurologic injuries were observed initially. Among them, 9 neurologic injuries were confirmed on the electromyogram test during the follow-up, which included 3 lumbosacral plexus injuries, 3 sciatic nerve injuries, and other injuries. Many neurologic injuries were resolved at the final follow-up, including all 3 lumbosacral plexus injuries and 2 out of the 3 sciatic nerve injuries.
Simple anteroposterior radiographs of the obturator foramen and iliac wing, inlet-outlet views of the pelvis, and computed tomography (CT) images were taken in the emergency room as long as the systemic status of the patients allowed their acquisition.
The fracture patterns were categorized into 5 "elementary" and 5 "associated" fracture patterns based on the criteria of Judet et al.11) There were 6 cases of elementary fractures, which were all anterior column fractures. The remaining 16 cases were associated fractures, including 6 cases of transverse and posterior wall fracture, 1 case of T-shaped fracture, 8 cases of anterior column and posterior hemitransverse fracture, and 1 case of both-column fractures (Table 3).
In addition, the fractures were further classified into non-comminuted or comminuted fracture. A comminuted acetabular fracture was defined when 3 or more fracture fragments were identified in the acetabular weight-bearing area on the midsagittal view of CT (Fig. 1).12) Nine cases were classified as comminuted fractures, and the other 13 cases were classified as non-comminuted fractures.
Low-molecular-weight heparin was administered to all of the patients at the time of hospitalization. Skeletal traction was applied prior to the operation in selected cases to reduce the pain or maintain the reduction. Surgical procedure was performed on the average seventh day after injury (range, 1 to 18 days). Preoperatively, systemic conditions and accompanying injuries in the patients were evaluated sufficiently. Surgical indication was displaced fractures through the weight-bearing dome. More specifically, the operation was performed in cases with free fragment(s) within the joint space, the roof arc angle2) less than 45°, and displacement more than 2 mm.3)
All of the surgical procedures were performed by one of the authors (HYK). In all events of application of the anterior approach in accordance with the fracture pattern (anterior wall, anterior column, anterior column and posterior hemitransverse fractures, some both-column fractures in which the anterior displacement was larger than the posterior displacement, and some transverse T-shaped fractures), surgery was performed via the modified Stoppa approach instead of the ilioinguinal approach. Some T-shaped and transverse fractures were included if the fracture in the posterior column was located high enough (close to the sciatic notch) in order to be addressed through the anterior approach and no posterior wall involvement was noted. Methods of reduction and fixation were determined and illustrated in the diagram by using CT images prior to the operation, and the diagram was printed out and pasted on the wall of the operating room prior to the operation.
The patient was positioned supine on the operating table and the reducibility of the fracture was checked with Carm. The entire lower limb and the lower abdomen were aseptically draped for the operation, and hip flexion was performed to relax the iliopsoas muscle, the external iliac/femoral neurovascular bundle, and the abdominal muscles by placing a large sandbag underneath the knee, and this also enabled multi-directional traction of the limbs for fracture reduction. The surgeon performed the operation on the contralateral side of the injured acetabulum. An arc-shaped skin incision of 12-15 cm was made 2 cm proximal to the superior pubic ramus. The incision was deepened to the abdominal fascia. The exposed rectus abdominis muscle was divided along the linea alba to approach the internal aspect of the pelvis.
On approaching the inside of the pelvis, corona mortis was identified and ligated first and subperiosteal dissection was performed along the pelvic brim to expose the fracture fragments. The obturator nerve and vessels that pass through the obturator foramen were usually identified easily and were protected during the further procedure (Fig. 2). Extreme precautions were taken to protect the external iliac artery and vein which lie just over the iliopsoas muscle which was retracted upwards. In some risky cases, the external iliac vein was damaged during the operation. These risky cases were of the patients with severe adhesions in this area due to previous surgeries such as repeated hernia operations or repeated cesarean sections, or of the patients in whom the operation was delayed by more than two weeks due to the other accompanying injuries. Once the fracture site was exposed, reduction was attempted and internal fixation was performed.
If the modified Stoppa approach alone was insufficient for reduction or internal fixation, a lateral window was made along the iliac crest to fix the high anterior column fracture (exiting the iliac crest) or to fix the posterior column with a lag screw. In addition, for fractures which could not be reduced using only the anterior approach such as those with an associated posterior wall fracture, the posterior approach (the Kocher-Langenbeck approach11)) was used concurrently or a week later. A screw, cable, and/or plate were used singly or in combination for fixation of the fracture.
Postoperatively, passive hip joint range of motion exercise using the continuous passvie motion device was encouraged as early as possible in the patients in whom solid fixation was achieved. Patients with severe comminution of the acetabulum were subjected to skeletal traction for 2-3 weeks. For determining the timing or extent of weight-bearing, the general condition of the patients, the severity of the accompanying injuries, the extent and quality of reduction, and stability of fixation were considered.
Only the modified Stoppa approach was used in 13 hips, while the Kocher-Langenbeck approach was additionally used in 9 hips (Table 3). In 2 cases (one with the anterior column and posterior hemitransverse fracture and the other with both-column fracture), a lateral window was made over the iliac crest simultaneously. A plate was applied in 20 cases. A pelvic reconstruction plate was used most frequently, and the other types of plates such as a hook plate were also used whenever necessary (Table 1).
The maximum displacement of the bony fragment was measured in the unit of mm by using PACS, Marosis mview ver. 5.4 (Marotech Inc., Seoul, Korea) on the simple radiographs and the CT images for evaluation of the fracture reduction quality based on the criteria of Matta2,13) and Matta et al.14,15) In this study, if the measured displacement was less than 0-1 mm, it was categorized as anatomical reduction, if it was in the range of 2-3 mm, it was categorized as imperfect reduction, and if it was > 3 mm, it was categorized as poor reduction. In addition, the radiographic and clinical results were categorized at the last follow-up as excellent, good, fair, and poor according to the criteria described by Matta2) and Matta et al.14) Finally, the accompanying injuries and complications were examined, and correlations between the clinical and radiographic results and between the fracture reduction quality and the extent of comminution were statistically analyzed. PASW ver. 18.0 (SPSS Inc., Chicago, IL, USA) was used for statistical analysis and Pearson correlation analysis was performed.
There were 17 cases of anatomical reduction, 4 cases of imperfect reduction, and 1 case of poor reduction. From these 17 cases, 2 cases categorized as anatomical reduction were excluded because of loss to follow-up.
Nine patients with comminuted fractures displaying more than 3 bony fragments in the acetabular weight-bearing area included 4 cases of anatomical reduction, 4 cases of imperfect reduction, and 1 case of poor reduction. In the case with comminution, it was difficult to achieve anatomical reduction (p = 0.03).
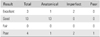
Among the 15 patients with anatomical reduction, 14 patients exhibited good and excellent results and only 1 patient exhibited a poor result. Two out of the 4 patients with imperfect reduction exhibited excellent results while the other 2 patients exhibited poor results. One patient with poor reduction exhibited a poor result (Table 4). The reduction quality correlated well with the clinical results (p = 0.03).
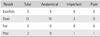
Fifteen out of the 18 patients who exhibited good and excellent results had anatomical reduction at the time of the operation. In the 3 patients without anatomical reduction (i.e., imperfect or poor reduction), good radiographic results were obtained (Table 5). In the cases with good anatomical reduction, the final radiographic results were also satisfactory (p = 0.01).
Poor reduction was observed in a patient with fracture-dislocation of the hip joint. The patient had a transverse and posterior wall fracture according to the classification of Judet et al.11) Reduction of the joint and the internal fixation of the fracture were performed in the operating room after 5 days without reduction of dislocation due to poor systemic state of the patient. Severe damage to the joint cartilage was observed during the operation. The patient showed poor clinical and radiographic results during the follow-up, and underwent hip joint fusion due to deep infection at 6 months after the operation, which resulted in successful control of the infection. In the third year after the operation, the fused hip joint underwent total hip replacement arthroplasty (THRA) and the patient regained mobility.
A total of 19 complications were observed in 13 patients (Table 6). Ten cases showed arthritic changes based on the criteria for radiographic arthritis described by Letournel et al.16) Most of them were graded as type I or II except for 2 patients who showed joint space narrowing and were graded as type III (which was surgically treated with THRA later). Deep infection and avascular necrosis were observed in one case. In this patient, the femoral head could not be reduced into the acetabular socket initially due to comminution and surgery was delayed by more than a week due to very poor general condition. THRA was performed in this patient.
The patients with ectopic bone formation (combined approach was used in all of these cases) did not complain of pain or limitation of motion. In one case, a screw was positioned intra-articularly, which was observed on the postoperative CT images. The screw was inserted via the posterior approach and was removed immediately. There was nonunion in the patient with a transverse and posterior wall fracture accompanied by dislocation. The patient exhibited poor radiographic and clinical results. Reoperation was performed to reduce the displaced fracture and to lay down the autogenous bone graft at 10 months after the initial operation.
Surgical approach to the acetabulum and accurate reduction and internal fixation are difficult because of its complicated anatomical structure and its deep location. Therefore, it is necessary to perform a thorough radiographic analysis and determine the preoperative plan including the order of reduction and method of fixation. Moreover, sufficient surgical field must be secured by deciding which approach is to be applied and in what order during the actual surgical procedure.
In general, better results are obtained with greater extent of radiographic results in the acetabular fracture.17) In particular, restoration of the upper weight-bearing dome14,18) of the acetabulum is the key to successful treatment. With the recent increase in high-energy injuries, there is a tendency for gradual increase in comminuted fractures of the acetabulum rather than a simple fracture with one or two bony fragments. The authors of this study, under the premise that greater extent of comminuted fracture would result in greater difficulty in achieving anatomical reduction with an ensuing poor result, examined the correlation between the number of bony fragments in the weight-bearing area (extent of comminution) on CT images, the reduction quality, and the clinical and radiographic results.
Although the quality of reduction (p = 0.03) and the clinical results (p = 0.04) were better in patients with a lesser number of bony fragments (extent of comminution), the radiographic results were not statistically significant (p = 0.74). However, it is deemed that a longer follow-up and an increasing number of cases would affect the radiographic results.
Letournel and Judet5) reported that anatomical reduction was achieved during the operation via the ilioinguinal approach in 73% of the 146 patients with acetabular fractures, and excellent radiographic results were obtained in 61% of the patients with both-column fractures, in 86% of the patients with anterior column fractures, and in 68% of the patients with anterior column and posterior hemitransverse fractures. Matta13) reported the results of application of ilioinguinal approach in a total 119 cases (with an average follow-up of 3 years). The results showed anatomical reduction in 74% of the cases, satisfactory reduction in 16% of the cases, and unsatisfactory reduction in 10% of the cases. The radiographic results during the follow-up were excellent in 63% of the cases, good in 21% of the cases, and fair in 14% of the cases, and the clinical results were excellent in 37% of the cases, good in 47% of the cases, fair in 14% of the cases, and poor in 2% of the cases. Hirvensalo et al.19) reported the results of operation through the modified Stoppa approach in a total 164 cases of acetabular fractures. A good result was obtained in 84% of the cases, a fair result was obtained in 9% of the cases, and a poor result was obtained in 7% of the cases, along with the clinical and the functional results of the Harris20) hip score of more than 75 points in 80% of the patients.
In our study, we were able to achieve anatomical reduction in 17 (77.3%) out of the 22 patients treated via the modified Stoppa approach, and the good and excellent clinical results were obtained in 16 cases (80%) and good and excellent radiographic results were obtained in 18 cases (90%) after the exclusion of 2 patients lost to follow-up. These results are similar or slightly better than the results obtained by the other researchers. This is considered to be the result of performing reduction through the lateral window in addition to the modified Stoppa approach or using the combined approach whenever necessary. In addition, we were able to confirm the correlation between reduction quality and results of the treatment as indicated by the finding that improved reduction leads to better radiographic and clinical results at the last follow-up (p < 0.05).
Numerous researchers reported that there is a close correlation between the radiographic results and the clinical results at the last follow-up.21,22) In this study, good and excellent radiographic results were obtained in 18 cases and good and excellent clinical results were obtained in 16 cases; thus, radiographic results were slightly better than the clinical results, and this enabled us to confirm the correlation between clinical and radiographic results (p < 0.05).
Marsh et al.23) stated that the most important factor that determines the clinical results was damage to the joint cartilage, which would induce degenerative changes in the joints even if anatomical reduction was achieved. This indicates that irreversible cartilage damage at the time of injury determines a substantial proportion of the clinical results. In this study, there was 1 case that showed a poor clinical result even after achieving anatomical reduction during the operation. In this patient, the femoral head showed severe slippage of the articular cartilage during the surgical procedure which was not visible on simple radiographs and CT images. We did not allow partial weight-bearing for a couple of weeks postoperatively. The patient started walking with crutches on the tenth day after the operation and complained of pain in the hip joint throughout the entire follow-up until THRA was performed. There was no nerve injury or other complications although the patient developed traumatic arthritis afterwards. The surgeon must make the decision regarding the timing of weight-bearing on the basis of reduction quality and stability of fixation.
Complications that can accompany acetabular fractures include ectopic bone formation, traumatic arthritis, nerve injury, infection, avascular necrosis of the femoral head, intra-articular screw placement, hip joint subluxation as well as non-union.3,24) With the use of the ilioinguinal approach, Letournel and Judet5) reported complications in 9% of the patients including 3 cases (2.1%) of infection, 8 cases (6%) of iliac nerve and sciatic nerve palsies, 2 cases (1.4%) of abdominal hernia requiring surgical repair, 3 cases (2.1%) of external iliac vein injuries, and 1 case of thrombosis of the internal and external iliac artery as well as ectopic bone formation. In the study by Matta,13) a complication rate of 13%, including 1 case of femoral artery injury, 1 case of femoral nerve palsy, and 3 cases of wound infection, was reported.
The occurrence of postoperative arthritis has been reported quite variably by the authors (17% by Letournel et al.16) to 57% by Pennal et al.25)). Letournel et al.16,26) reported that it took 10-25 years for 50% of the patients to develop traumatic arthritis after anatomical reduction, and it took less than 10 years for 80% of the patients who had an imperfect reduction to develop traumatic arthritis. In our study, 8 hips were graded as type I or II, and 2 hips were graded as type III. This is a relatively short-term follow-up study, and a long-term follow-up is necessary to accurately evaluate the occurrence of posttraumatic arthritis, especially in the cases graded as type I or II. As already mentioned above, 2 cases of type III arthritis showed avascular necrosis, poor reduction, or damage to the joint cartilage. They were surgically treated with THRA although the follow-up was relatively short.
In our study, there were 3 episodes of ectopic bone formation in the buttock area that were not approached posteriorly through the modified Stoppa approach in which the large muscles are not dissected in comparison to the classic ilioinguinal approach.1,13)
The lateral femoral cutaneous nerve is the most frequently injured nerve with the ilioinguinal approach.1,4) Nerve injury is thought to be due to excessive retraction or severing of the surgical window. The modified Stoppa approach avoids the middle window, which lessens the chances of injury to the inguinal canal, femoral nerve, and external iliac vessels. In this study, there was no episode of injury to these structures via the modified Stoppa approach.
The modified Stoppa approach provides the advantages of direct visualization of the entire pelvic brim from the pubic body to the anterior aspect of the sacral ala, direct visualization and access to the quadrilateral plate allowing for reduction and plating, and direct visualization and access to the posterior column from the greater sciatic notch to the ischial spine allowing for reduction and plating. In our study, the approach to these structures was easy and we were able to approach the upper section of the iliac bone and the iliac crest through an additional lateral window (Fig. 3). In addition, the modified Stoppa approach enabled to extend the surgical field inside the pelvis for performing operations for bilateral acetabular fractures and the accompanying ipsilateral or contralateral pelvic fractures.
However, the modified Stoppa approach needs much more delicate dissection in the cases with intrapelvic adhesions (such as revision surgery including implant removal, and previous surgery in the lower abdomen). Compared to the other pelvic approaches, it is much easier to perform the modified Stoppa approach in patients with a thin body type. Severe obesity and previous repeated pelvic surgery could be relative contraindications for the modified Stoppa approach.
Finally, this study has limitations since the follow-up period was short, the number of the subjects was less, and it was a retrospective study without a control group.
Excellent and good results could be achieved through the modified Stoppa approach for the treatment of acetabular fractures (p < 0.05). It can be concluded that the modified Stoppa approach could be used as an alternative to the classic ilioinguinal approach. In addition, comminution of the acetabular fracture was an important factor causing non-anatomic reduction (p = 0.03) and finally unsatisfactory clinical results (p = 0.04).
Figures and Tables
Fig. 1
(A) Acetabular weight-bearing area was divided into three 30° ranges on the midsagittal view according to Nishii et al.12) (B) Drawing of the weight-bearing area with 15° intervals at the center of the femoral head. (C) Comminuted fracture in the weight-bearing area.

Fig. 2
(A) A transverse skin incision 2 cm above the pubic symphysis. (B) Elevation of abdominal fascia over the rectus abdominis. (C) Midline split of the rectus abdominis. (D) Identification of the obturator nerve. (E) Elevation of rectus insertion on the pubis and ligation of corona mortis. (F) Subperiosteal dissection and open reduction and internal fixation.

Fig. 3
Preoperative (A) and postoperative (B) radiographs demonstrating placement of a double plate; one over the pelvic brim and the other over the quadrilateral plate. Preoperative (C) and postoperative (D) radiographs demonstrating fixation of a high anterior column fracture with a plate through the lateral window and another fixation over the entire pelvic brim from the pubic body to the anterior aspect of the sacroiliac joint.

Table 1
Patient Data
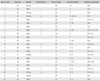
Table 2
Accompanying Injuries

Table 3
Operative Approach according to the Letournel and Judet Fracture Type
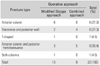
Table 4
Clinical Results Related according to the Quality of Reduction (p = 0.03)
| Result | Total | Anatomical | Imperfect | Poor |
|---|---|---|---|---|
| Excellent | 3 | 1 | 2 | 0 |
| Good | 13 | 13 | 0 | 0 |
| Fair | 0 | 0 | 0 | 0 |
| Poor | 4 | 1 | 2 | 1 |
Table 5
Radiographic Results Related according to the Quality of Reduction (p = 0.01)
| Result | Total | Anatomical | Imperfect | Poor |
|---|---|---|---|---|
| Excellent | 5 | 5 | 0 | 0 |
| Good | 13 | 10 | 3 | 0 |
| Fair | 0 | 0 | 0 | 0 |
| Poor | 2 | 0 | 1 | 1 |
Table 6
Complications

References
1. Letournel E. The treatment of acetabular fractures through the ilioinguinal approach. Clin Orthop Relat Res. 1993; (292):62–76.
2. Matta JM. Fractures of the acetabulum: accuracy of reduction and clinical results in patients managed operatively within three weeks after the injury. J Bone Joint Surg Am. 1996; 78(11):1632–1645.
3. Min BU, Nam SY, Kang CS. Complications of surgical treatment in patients with acetabular fractures. J Korean Hip Soc. 2000; 12(3):253–260.
4. Judet R, Judet J, Letournel E. Surgical treatment of recent fractures of the acetabulum: apropos of 46 operated cases. Mem Acad Chir (Paris). 1962; 88:369–377.
5. Letournel E, Judet R. Fractures of the acetabulum. Berlin: Springer-Verlag;1974.
6. Andersen RC, O'Toole RV, Nascone JW, Sciadini MF, Frisch HM, Turen CW. Modified stoppa approach for acetabular fractures with anterior and posterior column displacement: quantification of radiographic reduction and analysis of interobserver variability. J Orthop Trauma. 2010; 24(5):271–278.
7. Stoppa RE, Rives JL, Warlaumont CR, Palot JP, Verhaeghe PJ, Delattre JF. The use of Dacron in the repair of hernias of the groin. Surg Clin North Am. 1984; 64(2):269–285.
8. Rives J, Stoppa R, Fortesa L, Nicaise H. Dacron patches and their place in surgery of groin hernia: 65 cases collected from a complete series of 274 hernia operations. Ann Chir. 1968; 22(3):159–171.
9. Cole JD, Bolhofner BR. Acetabular fracture fixation via a modified Stoppa limited intrapelvic approach: description of operative technique and preliminary treatment results. Clin Orthop Relat Res. 1994; (305):112–123.
10. Hirvensalo E, Lindahl J, Bostman O. A new approach to the internal fixation of unstable pelvic fractures. Clin Orthop Relat Res. 1993; (297):28–32.
11. Judet R, Judet J, Letournel E. Fractures of the acetabulum: classification and surgical approaches for open reduction: preliminary report. J Bone Joint Surg Am. 1964; 46(8):1615–1646.
12. Nishii T, Tanaka H, Nakanishi K, Sugano N, Miki H, Yoshikawa H. Fat-suppressed 3D spoiled gradient-echo MRI and MDCT arthrography of articular cartilage in patients with hip dysplasia. AJR Am J Roentgenol. 2005; 185(2):379–385.
13. Matta JM. Operative treatment of acetabular fractures through the ilioinguinal approach: a 10-year perspective. Clin Orthop Relat Res. 1994; (305):10–19.
14. Matta JM, Anderson LM, Epstein HC, Hendricks P. Fractures of the acetabulum: a retrospective analysis. Clin Orthop Relat Res. 1986; (205):230–240.
15. Matta JM, Mehne DK, Roffi R. Fractures of the acetabulum: early results of a prospective study. Clin Orthop Relat Res. 1986; (205):241–250.
16. Letournel E, Judet R, Elson RA. Late complication of operative treatment within three weeks of injury. In : Letournel E, Judet R, Elson RA, editors. Fractures of the acetabulum. 2nd ed. Berlin: Springer-Verlag;1993. p. 541–563.
17. Borrelli J Jr, Goldfarb C, Ricci W, Wagner JM, Engsberg JR. Functional outcome after isolated acetabular fractures. J Orthop Trauma. 2002; 16(2):73–81.
18. Vrahas MS, Widding KK, Thomas KA. The effects of simulated transverse, anterior column, and posterior column fractures of the acetabulum on the stability of the hip joint. J Bone Joint Surg Am. 1999; 81(7):966–974.
19. Hirvensalo E, Lindahl J, Kiljunen V. Modified and new approaches for pelvic and acetabular surgery. Injury. 2007; 38(4):431–441.
20. Harris WH. Traumatic arthritis of the hip after dislocation and acetabular fractures: treatment by mold arthroplasty: an end-result study using a new method of result evaluation. J Bone Joint Surg Am. 1969; 51(4):737–755.
21. Matta JM, Merritt PO. Displaced acetabular fractures. Clin Orthop Relat Res. 1988; (230):83–97.
22. Pantazopoulos T, Mousafiris C. Surgical treatment of central acetabular fractures. Clin Orthop Relat Res. 1989; (246):57–64.
23. Marsh JL, Buckwalter J, Gelberman R, et al. Articular fractures: does an anatomic reduction really change the result. J Bone Joint Surg Am. 2002; 84(7):1259–1271.
24. Letournel E, Judet R. Fractures of the acetabulum. 2nd ed. Berlin: Springer-Verlag;1993.
25. Pennal GF, Davidson J, Garside H, Plewes J. Results of treatment of acetabular fractures. Clin Orthop Relat Res. 1980; (151):115–123.
26. Letournel E, Judet R, Elson RA. General principles of management of acetabular fractures. In : Letournel E, Judet R, Elson RA, editors. Fractures of the acetabulum. 2nd ed. Berlin: Springer-Verlag;1993. p. 347–361.




 PDF
PDF ePub
ePub Citation
Citation Print
Print


 XML Download
XML Download