Abstract
Background
Unstable simple elbow dislocation (USED) repair is challenged by the maintenance of joint reduction; hence, primary repair or reconstruction of disrupted ligaments is required to maintain the congruency and allow early motion of the elbow. We evaluated the effectiveness and the outcome of lateral collateral ligament (LCL) complex repair with additional medial collateral ligament (MCL) repair in cases of USED.
Methods
We retrospectively reviewed 21 cases of diagnosed USED without fractures around the elbow that were treated with primary ligament repair. In all cases, anatomical repair of LCL complex with or without common extensor origin was performed using suture anchor and the bone tunnel method. Next, the instability and congruency of elbow for a full range of motion were evaluated under the image intensifier. MCL was repaired only if unstable or incongruent elbow was observed. Clinical outcomes were evaluated using the Mayo elbow performance score (MEPS) and radiographic outcomes on last follow-up images.
Results
All cases achieved a stable elbow on radiographic and clinical results. LCL complex repair alone was sufficient to obtain the stable elbow in 17 of 21 cases. Four cases required additional MCL repair after restoration of the LCL complex. The overall mean MEPS was 91 (range, 70 to 100): excellent in 12 cases, good in 7 cases, and fair in 2 cases. All 17 cases with LCL complex repair only and 2 of 4 cases with additional MCL repair had excellent or good results by MEPS.
Elbow dislocation is divided into simple and complex dislocation. Simple dislocation occurs without a fracture around the elbow including the distal humerus, proximal ulna and proximal radius; whereas complex dislocation occurs with a concomitant fracture.1) Simple dislocation can be mostly treated with conservative management although the stability of joint needs to be assessed after reduction. According to some authors, surgical or non-surgically treatment of some simple dislocations more commonly leads to the complaint of decreased range of motion (ROM) than the instability of elbow joint.2,3) Initiation of early rehabilitation is helpful to reduce these complaints. Therefore, it is generally recommended to determine the treatment method of simple dislocation according to the stability on reduction of the elbow joint.1,4) If simple elbow dislocation requires an extension block of over 30° to 45° to maintain joint reduction, surgical treatment should be considered because early joint motion is impossible.4,5)
Surgical treatment of unstable simple elbow dislocation (USED) involves ligament suture or reconstruction, generally to restore both lateral collateral ligament (LCL) and medial collateral ligament (MCL).1,2,6,7) However, the repair of both LCL and MCL is not performed in all cases. Some authors reported satisfactory results of selective repair of LCL or MCL for USED.5,8) We surgically treated 21 patients diagnosed with USED. Repair of the LCL complex was first conducted in all the cases. MCL repair was performed additionally in cases of unstable elbows or lack of congruence in the full ROM. There are few previous reports on selective ligament repair in USED; hence, we have reported the findings of our study.
Twenty-one consecutive patients who were diagnosed with USED and treated by a single surgeon during the period between August 2007 and April 2013 were included in the study. In the same period, simple stable elbow dislocation occurred in 71 cases, which were treated with a closed reduction of the involved elbow and early mobilization using a hinged brace within 2 weeks after trauma. Cases with a radiographic subluxated or non-congruent joint after reduction of dislocation, or the elbows that required an extension limitation over 30° to 45° to maintain reduction was diagnosed as USED. The elbows accompanied by a small avulsion fragment of the origin of LCL complex or a small fracture of the tip of coronoid process (type I fracture by Regan-Morrey classification) on radiographs were included in this study. However, patients with associated fractures around the elbow joint such as distal humerus, olecranon, coronoid process and radial head were excluded. Also, dislocation with an open wound or delayed diagnosis over 3 weeks after injury was excluded. The subjects included 16 men and 5 women with an average age of 41.9 years (range, 19 to 77 years). The left elbow was involved in 15 cases and the right in 6 cases. The causes of injury were a fall from standing in 11 cases, sports injury in 5, a fall from a height in 3, and traffic accident in 2.
All dislocations were initially reduced in the emergency room without anesthesia and immobilized with a long arm splint. Radiographic examination was performed before and after the reduction of dislocation in all the cases. Subluxation or non-congruency of the reduced elbow was observed in 9 of the 21 cases, a small avulsion fragment of the origin of LCL complex in 5 cases, and type I fracture of the coronoid process in 3 cases. Magnetic resonance imaging was performed in 17 cases. Injury of the LCL complex was shown at the humeral attachment in all cases. The common extensor origin was involved in 16 cases, MCL in 10 cases, brachialis muscle in 5 cases, mobile wad in 4 cases, flexor-pronator muscles in 3 cases, and anconeus muscle in 1 case. Associated trauma of the ipsilateral upper limb was combined in 6 cases: 1 case with distal radioulnar fracture and dissociation of the distal radioulnar joint; 3 cases with distal radius fracture; 1 case with clavicle fracture and incomplete ulnar nerve injury; and 1 case with subluxation and incomplete injury of the ulnar nerve. No case was accompanied with vascular injury.
The average length of time from dislocation to surgery was 8 days (range, 1 to 20 days). Surgery was performed under general anesthesia or brachial plexus anesthesia. The elbow was evaluated for ROM and stability under fluoroscopy before skin incision (Fig. 1). The stability of the elbow was assessed through a full ROM with varying forearm rotation to determine the position of potential instability. And valgus and varus stress testing were performed in full extension and 15° to 30° flexion of the elbow. All the cases were surveyed for subluxation or non-congruency during the extension of the elbow joint. Skin incision was by a separated approach through the lateral and medial elbow. First of all, repair of the LCL complex using the modified Kocher approach was performed. In case of accompanying injury to the common extensor origin, the disrupted LCL and radio-capitellar joint were immediately exposed after dissection of subcutaneous tissue and fascia. Otherwise, the LCL complex was approached by separation between extensor carpi ulnaris and anconeus muscle. Disrupted LCL complex was repaired with an intraosseous suture anchor (DePuy Mitek, Johnson and Johnson, Raynham, MA, USA), and the torn common extensor origin was sutured with non-absorbable suture (2-0 Ethibond Excel, Ethicon, Johnson and Johnson) using the bone tunnel suture method. This repair was performed at a 90° flexed position of the elbow joint. Then, stability in the full ROM, especially extension, was evaluated under fluoroscopy. If full ROM was possible and subluxation or articular incongruity was not observed, the surgery was finished without the repair of medial structures. However, if the elbow was still unstable in extension, medial structures were repaired through the medial approach. Humeral detachment of MCL was repaired with an intraosseous suture anchor and midsubstance rupture of MCL was primarily repaired with non-absorbable material. However, the anterior capsule of the elbow was not repaired. The ulna nerve was protected for the operation without transposition. Anterior transposition was only performed in cases with instability of the ulnar nerve. The stability was reevaluated after repair of MCL and the anterior capsule. All the elbows were immobilized for 5 to 7 days in about 90° flexion postoperatively. At 5 to 7 days after surgery, a hinged elbow brace was installed and an active motion was initiated. Flexion was not restricted, whereas extension was restricted to 30° at this time. Full ROM was allowed after 3 weeks. Daily activities were allowed without the brace at 6 weeks and light sports activities were started at 3 months.
The mean follow-up period of the patients was 15.0 months (range, 6 to 39 months). Clinical outcomes were evaluated in terms of pain, ROM, joint stability, and elbow function using the Mayo elbow performance score (MEPS).9) The stability of the elbow was evaluated with valgus and varus stress testing. Additionally, the pivot shift maneuver or the chair test was used for posterolateral rotatory instability. Radiographic outcomes including posttraumatic changes such as subluxation, heterotopic ossification and traumatic arthritis were evaluated on the last follow-up images.
All cases achieved a stable elbow on radiographic and clinical results. None of the patients complained of instability or re-dislocation. Seventeen had repair of the LCL complex only and 4 had additional repair of MCL after repair of the LCL complex (Table 1). Incomplete ulnar nerve injury was seen in 2 cases. And 1 case with anterior subluxation of the ulnar nerve was treated with anterior subcutaneous transposition and MCL repair through the medial approach.
The mean MEPS was 91 (range, 70 to 100): excellent in 12 cases, good in 7 cases, and fair in 2 cases (Table 2). All 17 cases with LCL complex repair only obtained excellent or good results by MEPS. On the other hand, 2 of 4 cases with additional MCL repair had fair results. The average ROM was 121.0° (range, 75° to 140°), the average extension loss was 6.9° (range, -5° to 20°), and the average flexion was 127.9° (range, 90° to 140°). In cases with LCL repair only, the average ROM was 122.1° (range, 95° to 140°), the average extension loss was 6.5° (range, -5° to 20°), and the average flexion was 128.5° (range, 110° to 140°). In cases treated with MCL as well as LCL repair, they were 116.3° (range, 75° to 140°), 8.8° (range, 0° to 20°) and 125.0° (range, 90° to 140°), respectively. Among the 4 cases that had repair of both LCL and MCL, 3 cases (case number 9, 12, and 21) did not have discomfort in daily activities but complained of mild pain during heavy activities. The other case (case number 11) showed extension loss of 15° and flexion of 90° and complained of moderate or more severe pain.
In the radiographic examination, none of the cases showed joint subluxation, heterotopic ossification, or posttraumatic change on final images. Small calcifications around the epicondyle of distal humerus were found laterally in 1 case, medially in 3, and at both in 2 (Fig. 2).
Elbow dislocation comprises 11% to 28% of elbow injuries and occurs frequently in sports accidents.1,6,10) It occurs more commonly in men than in women, and in the youth than in the aged. Simple elbow dislocation is mainly treated with conservative management. Its clinical results are more satisfactory than those of complex elbow dislocation, and are better in children than in adults.11,12)
Many authors have reported favorable results after non-surgical treatment for simple dislocation of elbow.1,3,11,13,14) In addition, some authors have reported more satisfactory results after non-surgical treatment, as compared with surgical treatment.2,15) Josefsson et al.15) did not report better outcomes from repairing disrupted ligament in unstable dislocation without associated fracture. However, surgical repair is generally recommended in unstable elbow dislocation.4,5,7,16) Primary ligament repair combined with early postoperative exercise produced satisfactory outcomes in unstable elbow dislocation.7) It may occasionally be required to protect with a hinged external fixator despite ligament repair.16)
Simple elbow dislocation is usually stable and allows early full ROM. However, if the elbow joint subluxates, dislocates, or shows a non-congruent joint on X-ray after reduction of the dislocated elbow, the stability of joint should be reassessed. If the elbow requires an extension block of more than 30° to 45° or remains congruent, ligament repair should be considered as early exercise is impossible.1,4,5) In such cases, the full disruption of ligamentous and capsular structures may occur from lateral to medial.5,17) If the elbow is too unstable, injuries of muscles around the elbow need to be considered. It is not difficult to discriminate between stable dislocation and unstable dislocation if a non-congruent joint is observed on radiographs after the reduction of dislocation. We evaluated active ROM in patients with radiographic congruent joints at the outpatient clinic and 4 additional cases were diagnosed as USED. If the patient was unable to extend less than 30° to 45° during active extension of the elbow joint, we diagnosed USED and recommended ligament repair because early rehabilitation was impossible.
Treatment of USED is commonly performed by primary repair of both MCL and LCL complex.1,2,6,7) On the other hand, some authors reported selective ligament repair. Duckworth et al.16) described 8 of 15 elbows with LCL complex repair only and 7 with repair of both MCL and LCL complex. The former required a hinged external fixation in 2 elbows and had residual subluxation in 1 elbow. The latter required a hinged external fixation in 1 elbow and had residual subluxation or re-dislocation in 4 elbows. Therefore, they recommended protection with a hinged external fixation because ligament repair alone may not be sufficient. McKee et al.8) performed open operative repair on 62 elbows and found that, whereas all had rupture of the LCL complex, 41 of the 62 elbows had concomitant rupture of the common extensor origin, 28 of 50 elbows had disrupted MCL, and 9 of 50 elbows had concomitant rupture of flexor-pronator mass. They performed medial exploration or repair on instability after fracture fixation and/or LCL repair. Their results are helpful to decide operative methods such as surgical approach, ligament repair techniques, and rehabilitation protocols. Hobgood et al.5) first assessed the lateral followed by the medial side of the unstable elbow. Stability in extension was evaluated under an image intensifier after the LCL complex and the common extensor origin were repaired. If the elbow is unstable in extension, medial structures require repair. They reported that repair of lateral soft tissue was usually sufficient to restore stability although a high-energy injury in young patients may require additional repair of medial structures. We performed ligament repair using a method similar to the surgical protocol by Hobgood et al.5) In our study, 17 of the 21 elbows with repair of the LCL complex only showed excellent or good results. Also, the results showed no evidence of an age effect although statistical comparison was not conducted. Two of 4 cases with additional MCL repair were evaluated as fair in MEPS. One case (no. 9) complained of limited extension and another (no. 11) of decreased ROM and ulnar nerve symptoms. The spectrum of elbow instability initially disrupted the LCL complex and finally the MCL complex, resulting in complete dislocation.8,17) It is not always necessary to repair the MCL complex even if some valgus instability is shown on intraoperative image intensifier, because LCL complex repair alone offers sufficient stability for extension and flexion with varying forearm rotation. Therefore, additional medial soft tissue repair is necessary if the extent of soft tissue injuries around the elbow joint is too serious to maintain the stability with LCL complex repair alone.
Complications of simple elbow dislocation include contracture, pain, heterotopic ossification, neurovascular injuries and residual instability.1,13,18) Mehlhoff et al.13) studied 90 patients treated with closed reduction for simple elbow dislocation, of which 60% reported residual symptoms: 15% with flexion contracture over 30°, 45% with residual pain, and 35% with valgus instability. They advised early active exercise since prolonged immobilization after dislocation was strongly associated with unsatisfactory results. Protzman14) also recommended less than 3 weeks immobilization after reduction because loss of extension tended to occur more commonly than the loss of flexion and its severity was correlated with the duration of immobilization. Primary ligament repair in acute unstable elbow dislocation can achieve sufficient stability to allow early exercise.7) In this study, active and active-assisted exercise with a hinged brace was initiated in all elbows within a week of operation. However, instability or in-congruency was not observed in any case at the last follow-up.
Limitations of our study were as follows. First, this study was a retrospective study with selective hospital cases. Second, we used clinical results of a small series with a short follow-up period. Accordingly, the assessment of posttraumatic changes in the joint may be defective. Third, stability was evaluated by subjective complaints and physical examination. Objective examinations such as stress X-ray were not performed. Despite these limitations, the study has significance concerning treatment options for USED.
In conclusion, the disruption of both LCL complex and MCL is commonly detected in USED. However, surgical repair of both LCL complex and MCL is not always required for all elbows. If stability can be attained by one-sided ligament repair, i.e., LCL complex repair, and early rehabilitation is permissible, non-surgical treatment of the opposite ligament is possible.
Figures and Tables
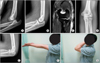 | Fig. 1Case 3: a 38-year-old man treated by repair of lateral collateral ligament (LCL) complex alone. (A) Initial radiograph showing dislocation on left elbow. (B) After closed reduction, the elbow was not congruent on lateral view. (C) Magnetic resonance imaging scan showing injuries of LCL complex and sprain of medial collateral ligament. (D, E) Radiographs at postoperative 3 months showing stable elbow. (F, G) Photographs at postoperative 3 months. |
 | Fig. 2Case 10: a 30-year-old injured by a fall from height. (A, B) Initial radiographs showing dislocation of the left elbow and associated fracture of the left wrist. (C) A lateral radiograph after closed reduction demonstrated a persistent subluxation of radio-capitellar and widening of ulno-humeral joint. (D) Magnetic resonance imaging scan showing injuries of lateral collateral ligament (LCL) complex and medial collateral ligament. (E) Intraoperative photograph showing complete detachment of LCL and common extensor origin from the lateral epicondyle. (F) At 18 months after repair of LCL only, the radiograph revealed small calcification around the lateral epicondyle. (G, H) Photographs at 18 months follow-up. |
Table 1
Summary of Patients with Unstable Simple Elbow Dislocation

References
1. Sheps DM, Hildebrand KA, Boorman RS. Simple dislocations of the elbow: evaluation and treatment. Hand Clin. 2004; 20(4):389–404.
2. Josefsson PO, Gentz CF, Johnell O, Wendeberg B. Surgical versus nonsurgical treatment of ligamentous injuries following dislocations of the elbow joint. Clin Orthop Relat Res. 1987; (214):165–169.
3. Josefsson PO, Johnell O, Gentz CF. Long-term sequelae of simple dislocation of the elbow. J Bone Joint Surg Am. 1984; 66(6):927–930.
4. O'Driscoll SW, Jupiter JB, King GJ, Hotchkiss RN, Morrey BF. The unstable elbow. Instr Course Lect. 2001; 50:89–102.
5. Hobgood ER, Khan SO, Field LD. Acute dislocations of the adult elbow. Hand Clin. 2008; 24(1):1–7.
6. Josefsson PO, Johnell O, Wendeberg B. Ligamentous injuries in dislocations of the elbow joint. Clin Orthop Relat Res. 1987; (221):221–225.
7. Micic I, Kim SY, Park IH, Kim PT, Jeon IH. Surgical management of unstable elbow dislocation without intra-articular fracture. Int Orthop. 2009; 33(4):1141–1147.
8. McKee MD, Schemitsch EH, Sala MJ, O'Driscoll SW. The pathoanatomy of lateral ligamentous disruption in complex elbow instability. J Shoulder Elbow Surg. 2003; 12(4):391–396.
9. Morrey BF, An KN. Functional evaluation of the elbow. In : Morrey BF, Sanchez-Sotelo J, editors. The elbow and its disorders. 4th ed. Philadelpia: Saunders;2009. p. 80–91.
10. Josefsson PO, Nilsson BE. Incidence of elbow dislocation. Acta Orthop Scand. 1986; 57(6):537–538.
11. Borris LC, Lassen MR, Christensen CS. Elbow dislocation in children and adults: a long-term follow-up of conservatively treated patients. Acta Orthop Scand. 1987; 58(6):649–651.
12. Mehta JA, Bain GI. Elbow dislocations in adults and children. Clin Sports Med. 2004; 23(4):609–627.
13. Mehlhoff TL, Noble PC, Bennett JB, Tullos HS. Simple dislocation of the elbow in the adult: results after closed treatment. J Bone Joint Surg Am. 1988; 70(2):244–249.
14. Protzman RR. Dislocation of the elbow joint. J Bone Joint Surg Am. 1978; 60(4):539–541.
15. Josefsson PO, Gentz CF, Johnell O, Wendeberg B. Surgical versus non-surgical treatment of ligamentous injuries following dislocation of the elbow joint: a prospective randomized study. J Bone Joint Surg Am. 1987; 69(4):605–608.
16. Duckworth AD, Ring D, Kulijdian A, McKee MD. Unstable elbow dislocations. J Shoulder Elbow Surg. 2008; 17(2):281–286.
17. O'Driscoll SW, Morrey BF, Korinek S, An KN. Elbow subluxation and dislocation: a spectrum of instability. Clin Orthop Relat Res. 1992; (280):186–197.
18. Martin BD, Johansen JA, Edwards SG. Complications related to simple dislocations of the elbow. Hand Clin. 2008; 24(1):9–25.




 PDF
PDF ePub
ePub Citation
Citation Print
Print


 XML Download
XML Download