Abstract
Background
The literature does not provide consistent information on the impact of patients' gender on recovery after rotator cuff repair. The purpose of this study was to determine whether gender affects pain and functional recovery in the early postoperative period after rotator cuff repair.
Methods
Eighty patients (40 men and 40 women) were prospectively enrolled. Pain intensity and functional recovery were evaluated, using visual analog scale (VAS) pain score and range of motion on each of the first 5 postoperative days, at 2 and 6 weeks and at 3, 6, and 12 months after surgery. Perioperative medication-related adverse effects and postoperative complications were also assessed.
Results
The mean VAS pain score was significantly higher for women than men at 2 weeks after surgery (p = 0.035). For all other periods, there was no significant difference between men and women in VAS pain scores, although women had higher scores than men. Mean forward flexion in women was significantly lower than men at 6 weeks after surgery (p = 0.033) and the mean degree of external rotation in women was significantly lower than men at 6 weeks (p = 0.007) and at 3 months (p = 0.017) after surgery. There was no significant difference in medication-related adverse effects or postoperative complications.
Conclusions
Women had more pain and slower recovery of shoulder motion than men during the first 3 months after rotator cuff repair. These findings can serve as guidelines for pain management and rehabilitation after surgery and can help explain postoperative recovery patterns to patients with scheduled rotator cuff repair.
Arthroscopic rotator cuff repair is currently a popular and well-established technique with well documented satisfactory clinical outcomes.1,2,3) However, some patients report persistent pain and poor shoulder function after rotator cuff repair. Thus, identification of factors associated with poor clinical outcomes for the procedure is clinically important and has received increasing attention.3,4)
Age, gender, duration of symptoms, preoperative stiffness, working status, workers' compensation claims, tear size, and tendon quality are associated with clinical outcomes of rotator cuff repair.1,2,3,4,5,6,7,8) Despite numerous studies, factors related to pain and functional disability remain unclear.4)
Little attention has been paid to the impact of gender on clinical outcomes of rotator cuff repair. Recently, the impact of gender on postoperative pain in various surgeries has attracted interest.9,10,11,12) Many studies have documented gender-related differences in pain after experimental exposure to noxious stimuli, with lower pain thresholds or higher pain ratings for women than for men.11,13) Women and men may have different experiences, behaviors, and expectations related to clinical outcomes after surgery.11,13,14,15,16)
Only a limited number of studies have investigated the relationship between gender and clinical outcomes of rotator cuff repair.1,2,3,4,6,7,8,14,17,18) Although several studies have documented that female gender is a negative prognostic factor for clinical outcomes of rotator cuff repair,1,4,6,7,14) the information on the impact of patients' gender on recovery from the procedure has been inconsistent.8,17,18,19,20) Furthermore, few prospective studies have reported standardized serial evaluation of gender-related difference on clinical outcomes during the first year after rotator cuff repair. Identifying existing differences between men and women regarding pain and function recovery would be helpful in the search for better models of care and optimal clinical management after rotator cuff repair.14)
The primary objective of this study was to determine whether gender affects pain and functional recovery in the early postoperative period after arthroscopic rotator cuff repair. The study hypothesis was that women have more pain and slower recovery of range of motion (ROM) than men. The secondary objective was to compare the incidence of perioperative medication-related adverse effects and postoperative complications for men versus women.
Keimyung University Dongsan Medical Center Institution's Review Board approved all protocols and all patients provided written informed consent. Between January 2009 and September 2010, 80 consecutive patients who had undergone arthroscopic rotator cuff repair were prospectively enrolled; they were divided among 2 groups of 40 men and 40 women. Inclusion criteria included rotator cuff tear diagnosed by clinical findings and imaging studies, failure of conservative treatment of at least 3 months' duration, and complete restoration of anatomical footprint. Exclusion criteria included irreparable tear, workers' compensation claim, revision surgery, an additional procedure such as biceps tenodesis, repair of a superior labral tear from anterior to posterior, stabilization for instability, and distal clavicular resection. All operations were performed by the same surgeon, who used an arthroscopic technique for rotator cuff repair.
In both groups, perioperative and postoperative pain was controlled according to a standard multimodal protocol. All patients received preemptive oral medication preoperatively and an intraoperative injection of a cocktail of local analgesics. For postoperative pain control, immediate-release oxycodone HCl, acetaminophen, and cyclooxygenase-2 selective inhibitor were given orally after surgery and through postoperative day 2. A cyclooxygenase-2 selective inhibitor plus a tablet containing a combination of 37.5 mg of tramadol and 325 mg of acetaminophen was given on postoperative days 3 through 5. For patients who required subsequent pain control, oral analgesics (tablet containing a combination of 37.5 mg of tramadol and 325 mg of acetaminophen) were prescribed for use until 4 weeks after surgery.
The postoperative rehabilitation protocol was the same for both groups. All patients engaged in pendulum exercises and exercises using a continuous passive motion machine until postoperative day 5, followed by the initiation of passive ROM exercises. They began active ROM exercises at 6 weeks after surgery, muscle-strengthening exercises at 3 months, and occupational or sports activities at 6 months.
Pain intensity was assessed using visual analog scale (VAS) pain scores (0, no pain; 10, unbearable pain) on each of the first 5 postoperative days, at 2 and 6 weeks, and at 3, 6, and 12 months. ROM was evaluated in 2 directions i.e., forward flexion and external rotation at 2 and 6 weeks after surgery and at 3, 6, and 12 months. Perioperative medication-related adverse effects (nausea, vomiting, urinary retention, constipation, dizziness, urticaria, and headache) and postoperative complications (postoperative shoulder stiffness and infection) were also assessed. Stiffness was defined as passive forward flexion of < 120° and passive external rotation with the arm at the side of < 30° at 12 months after surgery.
We defined a statistically significant 1.2-point difference in VAS pain score between the 2 groups in a power analysis. A sample size of 36 patients per group was required for a power of 80% at a 5% significance level with a standard deviation of 1.8 points. Expected follow-up loss was about 10%.
Statistical analysis was performed using SPSS ver. 14.0 (SPSS Inc., Chicago, IL, USA). We used the independent t-test and the chi-square test to compare baseline demographics between the 2 groups. The independent t-test and repeated-measures analysis of variance were used to evaluate the changes in VAS pain scores and ROM. Two-tailed p-values of < 0.05 were considered significant.
No significant differences were found between the 2 groups with regard to age, involved side, body mass index, preoperative shoulder stiffness, duration of symptoms, tear size, duration of surgery, or repair technique (p > 0.05) (Table 1). Additionally, there were no significant differences between groups in mean preoperative VAS pain scores or ROM (p > 0.05).
All patients had significant improvement in VAS pain score and ROM at 12 months after surgery (P < 0.001). The mean VAS pain scores from postoperative days 0 to 5 were 6.2, 4.6, 3.6, 3.3, 2.8, and 2.4 for men and 6.4, 4.8, 4.0, 3.2, 3.2, and 2.7 for women. At 2 weeks, 6 weeks, 3 months, 6 months, and 12 months after surgery, the mean scores were 2.4, 2.2, 1.9, 1.5, and 0.8, respectively, for the men and 2.9, 2.7, 2.1, 1.3, and 1.3, respectively, for the women. The mean score for the women was significantly higher than the mean for the men at 2 weeks after surgery (p = 0.035). However, at all other time points, there was no significant difference between the groups (P > 0.05), even though the scores were higher in women than men (Table 2 and Fig. 1).
Mean forward flexion at 2 weeks, 6 weeks, 3 months, 6 months, and 12 months after surgery was 132.6°, 144.9°, 152.5°, 159.0°, and 160.8°, respectively, in the men and 132.8°, 138.5°, 145.9°, 156.0°, and 162.4°, respectively, in the women; it was significantly lower (p = 0.033) in the women than in the men at 6 weeks (Table 3 and Fig. 2). Mean external rotation at 2 weeks, 6 weeks, 3 months, 6 months, and 12 months after surgery was 34.8°, 37.4°, 46.4°, 52.8°, and 57.5°, respectively, in the men and 31.0°, 32.5°, 39.9°, 48.3°, and 55.0°, respectively, in the women; it was significantly lower in the women than the men at 6 weeks (p = 0.007) and at 3 months (p = 0.017) after surgery (Fig. 3).
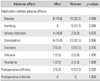
In evaluating medication-related adverse effects, we found no significant differences between the 2 groups with regard to nausea, vomiting, urinary retention, constipation, dizziness, urticaria, or headache (P > 0.05) (Table 4). Postoperative shoulder stiffness at 12 months after surgery was present in 2 men (5%) and in 5 women (12.5%), without statistical significance (P > 0.05). No local complications, including infection, were encountered in either group.
The current study showed that pain and functional recovery during the first 3 months after arthroscopic rotator cuff repair is associated with gender. The results were thus supportive of the hypothesis that women have more pain and slower recovery of ROM than men in the early postoperative period.
The goal of rotator cuff repair is to improve patients' quality of life by reducing pain and enhancing shoulder function.5) Numerous short-term to midterm follow-up studies have demonstrated excellent clinical outcomes after arthroscopic rotator cuff repair.1,2,3) Appropriate perioperative and postoperative pain management for patients undergoing rotator cuff repair is considered a major issue that can influence the effectiveness of treatment and rehabilitation in the early postoperative period.21,22) Furthermore, it is an important measure for judging postoperative satisfaction with rotator cuff repair.
Age, gender, duration of symptoms, preoperative stiffness, working status, workers' compensation claims, tear size, and tendon quality are reportedly associated with clinical outcomes after rotator cuff repair.1,2,3,4,5,6,7,8) Of these parameters, age and tear size are considered the most important prognostic factors influencing clinical and anatomical outcomes,4,5,18) whereas the effects of gender on clinical outcomes has received little attention. However, the impact of gender on pain perception and analgesic response is increasingly being studied.10,12) Women have a lower pain threshold and less tolerance for experimental and postoperative pain than men.11,13,15,16) Some evidence suggests that responses to treatment may differ between women and men.11,15,23)
Only a limited number of studies have investigated the relationship between gender and clinical outcomes of rotator cuff repair.1,2,3,4,6,7,8,14,17,18) Several authors have suggested that women have poorer clinical outcomes than men,1,2,3,4,6,7,14) but others have reported that gender does not influence clinical outcomes.17,20) Charousset et al.1) evaluated 104 patients (53 men and 61 women) with arthroscopic rotator cuff repair and reported that female gender is a negative predictive factor for clinical results at a minimum of 2 years after surgery. Oh et al.4) evaluated 78 patients (39 men and 39 women) with rotator cuff repair and reported that women had lower Simple Shoulder Test scores after a mean final follow-up period of 19.6 months, but they found no significant difference in the American Shoulder and Elbow Surgeons scores between men and women. Meanwhile, O'Holleran et al.20) reported that in 216 men and 95 women, gender was not a significant determinant of clinical outcomes and satisfaction after rotator cuff surgery. In addition, Feng et al.19) evaluated 1,120 shoulders (872 men and 248 women) after the procedure and reported that gender was not correlated with postoperative clinical outcome after a mean final follow-up period of 7.9 years. Surprisingly, Watson and Sonnabend8) reported that of the 667 patients who underwent open rotator cuff repair, men had less satisfactory clinical results than women after a mean final follow-up period of 3.8 years. Overall, previous studies did not produce consistent findings on the impact of gender on recovery from rotator cuff repair.
Razmjou et al.14) conducted a prospective longitudinal study to determine the overall gender-related differences in disability at 6 months after rotator cuff surgery. They documented that women have higher levels of postoperative disability than men, which is similar to the findings for our study. In the current study, women had higher VAS pain scores than men at 2 weeks after surgery, but although the women's scores were higher for all other periods, the difference was not statistically significant. Also, our study showed that compared with men, women had significantly less forward flexion at 6 weeks and significantly less external rotation at both 6 weeks and 3 months after surgery. These results indicated that the women in the current study had more pain or slower recovery of shoulder motion than men during the first 3 months.
Most previous studies comparing gender-related differences in clinical outcomes of rotator cuff repair were retrospective in nature. Furthermore, they focused on clinical outcome alone at final follow-up examination, and provided no evidence of gender-related differences in the early postoperative period. The main limitation of these investigations was that gender-related differences were not the primary outcome. The strengths of our study were its prospective design and primary research focus of gender-related differences. To our knowledge, this was the first study to compare gender-related differences with respect to pain intensity and functional recovery in the perioperative and short-term postoperative periods.
Several studies have shown that the incidence of medication-related adverse effects, including nausea and vomiting, for postoperative analgesia is higher in women than in men.11,12) Although such adverse events were not statistically significant, possibly due to the small study cohort, we observed gender differences with respect to nausea (15.0% men vs. 32.5% women), vomiting (0% vs. 12.5%), and constipation (15.0% vs. 32.5%). The reported incidence of postoperative shoulder stiffness after arthroscopic rotator cuff repair ranges from 3.3% to 16.7%.24-28) However, few studies have focused on gender differences with respect to postoperative stiffness. In the current study, postoperative shoulder stiffness was present at 12 months after surgery in 2 men (5%) and 5 women (12.5%), which did not represent a significant difference. Because the current study had a small sample size and a short follow-up period, the results of medication-related adverse effects and postoperative shoulder stiffness can only be extrapolated minimally. Hence, further study is needed to accurately evaluate the gender-related differences.
Our study had several limitations. First, sample size was relatively small. Second, only VAS pain scores and ROM were used as indicators of clinical outcome. Because the study focused on pain intensity and recovery of ROM in the early postoperative period, shoulder-specific outcome measures and recovery of muscle power were not evaluated. Third, the study did not account for potentially confounding variables such as racial or ethnic, cultural, political, or social factors, which prevents a more complete interpretation of the results. Fourth, we did not determine gender-related differences in anatomical outcome because the structural integrity of repaired rotator cuffs was not assessed by ultrasonography or magnetic resonance imaging. Thus, further prospective longitudinal research with a large cohort is necessary.
Our results indicated that surgeons should consider gender-related differences when planning rotator cuff repair, because women may need novel and individualized regimens for pain management and rehabilitation to improve their comfort after surgery. An approach that considers gender-related differences will enable more successful clinical outcomes after arthroscopic rotator cuff repair.
Figures and Tables
Fig. 1
Pain intensity was measured using visual analog scale (VAS) pain scores on each of the first 5 postoperative days and then at 2 weeks, 6 weeks, 3 months, 6 months, and 12 months after surgery. The mean VAS pain score was significantly higher for women than for men at 2 weeks after surgery (*P = 0.035).
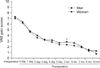
Fig. 2
Forward flexion was measured at 2 weeks, 6 weeks, 3 months, 6 months, and 12 months after surgery and was significantly lower for women than for men at 6 weeks (*P = 0.033).
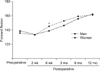
Fig. 3
External rotation was measured at 2 weeks, 6 weeks, 3 months, 6 months, and 12 months after surgery. Mean postoperative external rotation was significantly lower for women than for men at 6 weeks (*P = 0.007) and at 3 months (*P = 0.017).
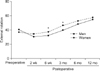
Table 1
Demographic Data

Table 2
Comparison of Visual Analog Scale Pain Scores

Table 3
Comparison of Shoulder Range of Motion

Table 4
Comparison of Medication-Related Adverse Effects and Postoperative Complications
References
1. Charousset C, Grimberg J, Duranthon LD, Bellaiche L, Petrover D, Kalra K. The time for functional recovery after arthroscopic rotator cuff repair: correlation with tendon healing controlled by computed tomography arthrography. Arthroscopy. 2008; 24(1):25–33.
2. Chung SW, Park JS, Kim SH, Shin SH, Oh JH. Quality of life after arthroscopic rotator cuff repair: evaluation using SF-36 and an analysis of affecting clinical factors. Am J Sports Med. 2012; 40(3):631–639.
3. Nho SJ, Shindle MK, Adler RS, Warren RF, Altchek DW, MacGillivray JD. Prospective analysis of arthroscopic rotator cuff repair: subgroup analysis. J Shoulder Elbow Surg. 2009; 18(5):697–704.
4. Oh JH, Kim SH, Ji HM, Jo KH, Bin SW, Gong HS. Prognostic factors affecting anatomic outcome of rotator cuff repair and correlation with functional outcome. Arthroscopy. 2009; 25(1):30–39.
5. Baysal D, Balyk R, Otto D, Luciak-Corea C, Beaupre L. Functional outcome and health-related quality of life after surgical repair of full-thickness rotator cuff tear using a mini-open technique. Am J Sports Med. 2005; 33(9):1346–1355.
6. Robinson PM, Wilson J, Dalal S, Parker RA, Norburn P, Roy BR. Rotator cuff repair in patients over 70 years of age: early outcomes and risk factors associated with re-tear. Bone Joint J. 2013; 95(2):199–205.
7. Romeo AA, Hang DW, Bach BR Jr, Shott S. Repair of full thickness rotator cuff tears: gender, age, and other factors affecting outcome. Clin Orthop Relat Res. 1999; (367):243–255.
8. Watson EM, Sonnabend DH. Outcome of rotator cuff repair. J Shoulder Elbow Surg. 2002; 11(3):201–211.
9. Aubrun F, Salvi N, Coriat P, Riou B. Sex- and age-related differences in morphine requirements for postoperative pain relief. Anesthesiology. 2005; 103(1):156–160.
10. Cepeda MS, Carr DB. Women experience more pain and require more morphine than men to achieve a similar degree of analgesia. Anesth Analg. 2003; 97(5):1464–1468.
11. Fillingim RB, King CD, Ribeiro-Dasilva MC, Rahim-Williams B, Riley JL 3rd. Sex, gender, and pain: a review of recent clinical and experimental findings. J Pain. 2009; 10(5):447–485.
12. Schnabel A, Poepping DM, Gerss J, Zahn PK, Pogatzki-Zahn EM. Sex-related differences of patient-controlled epidural analgesia for postoperative pain. Pain. 2012; 153(1):238–244.
13. Taenzer AH, Clark C, Curry CS. Gender affects report of pain and function after arthroscopic anterior cruciate ligament reconstruction. Anesthesiology. 2000; 93(3):670–675.
14. Razmjou H, Davis AM, Jaglal SB, Holtby R, Richards RR. Disability and satisfaction after rotator cuff decompression or repair: a sex and gender analysis. BMC Musculoskelet Disord. 2011; 12:66.
15. Ochroch EA, Gottschalk A, Troxel AB, Farrar JT. Women suffer more short and long-term pain than men after major thoracotomy. Clin J Pain. 2006; 22(5):491–498.
16. Rosseland LA, Stubhaug A. Gender is a confounding factor in pain trials: women report more pain than men after arthroscopic surgery. Pain. 2004; 112(3):248–253.
17. Bennett WF. Arthroscopic repair of full-thickness supraspinatus tears (small-to-medium): a prospective study with 2-to 4-year follow-up. Arthroscopy. 2003; 19(3):249–256.
18. Manaka T, Ito Y, Matsumoto I, Takaoka K, Nakamura H. Functional recovery period after arthroscopic rotator cuff repair: is it predictable before surgery? Clin Orthop Relat Res. 2011; 469(6):1660–1666.
19. Feng S, Guo S, Nobuhara K, Hashimoto J, Mimori K. Prognostic indicators for outcome following rotator cuff tear repair. J Orthop Surg (Hong Kong). 2003; 11(2):110–116.
20. O'Holleran JD, Kocher MS, Horan MP, Briggs KK, Hawkins RJ. Determinants of patient satisfaction with outcome after rotator cuff surgery. J Bone Joint Surg Am. 2005; 87(1):121–126.
21. Cho CH, Song KS, Min BW, et al. Multimodal approach to postoperative pain control in patients undergoing rotator cuff repair. Knee Surg Sports Traumatol Arthrosc. 2011; 19(10):1744–1748.
22. Oh JH, Rhee KY, Kim SH, Lee PB, Lee JW, Lee SJ. Comparison of analgesic efficacy between single interscalene block combined with a continuous intra-bursal infusion of ropivacaine and continuous interscalene block after arthroscopic rotator cuff repair. Clin Orthop Surg. 2009; 1(1):48–53.
23. Kamath AF, O'Connor MI. Breakout session: gender and ethnic disparities in pain management. Clin Orthop Relat Res. 2011; 469(7):1962–1966.
24. Cho CH, Song KS, Jung GH, Lee YK, Shin HK. Early postoperative outcomes between arthroscopic and mini-open repair for rotator cuff tears. Orthopedics. 2012; 35(9):e1347–e1352.
25. Chung SW, Huong CB, Kim SH, Oh JH. Shoulder stiffness after rotator cuff repair: risk factors and influence on outcome. Arthroscopy. 2013; 29(2):290–300.
26. Denard PJ, Ladermann A, Burkhart SS. Prevention and management of stiffness after arthroscopic rotator cuff repair: systematic review and implications for rotator cuff healing. Arthroscopy. 2011; 27(6):842–848.
27. Oh CH, Oh JH, Kim SH, Cho JH, Yoon JP, Kim JY. Effectiveness of subacromial anti-adhesive agent injection after arthroscopic rotator cuff repair: prospective randomized comparison study. Clin Orthop Surg. 2011; 3(1):55–61.
28. Oh JH, Kim SH, Lee HK, Jo KH, Bin SW, Gong HS. Moderate preoperative shoulder stiffness does not alter the clinical outcome of rotator cuff repair with arthroscopic release and manipulation. Arthroscopy. 2008; 24(9):983–991.




 PDF
PDF ePub
ePub Citation
Citation Print
Print


 XML Download
XML Download