Abstract
Background
Total knee arthroplasty (TKA) is associated with considerable blood loss. Computer-assisted surgery (CAS) is different from conventional TKA as it avoids opening the intramedullary canal. Hence, CAS should be associated with less blood loss.
Methods
Fifty-seven patients were randomized into two groups of CAS and conventional TKA. In conventional group intramedullary femoral and extramedullary tibial jigs were used whereas in CAS group imageless navigation system was used. All surgeries were done under tourniquet. Total and hidden blood loss was calculated in both groups and compared.
Results
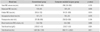
The mean total blood loss was 980 mL in conventional group and 970 mL in CAS group with median of 1,067 mL (range, 59 to 1,791 mL) in conventional group and 863 mL (range, 111 to 2,032 mL) in CAS group. There was no significant difference in total blood loss between the two groups (p = 0.811). We have found significant hidden blood loss in both techniques, which is 54.8% of the total loss in the conventional technique and 59.5% in the computer-assisted navigation technique.
Total knee replacement is associated with considerable blood loss.1) The safety of total knee arthroplasty (TKA) would be improved with a procedure that results in reduced blood loss. Some of the measures mentioned in literature to minimize the intraoperative blood loss are the use of tourniquet,2) minimally invasive surgery,3) use of anti-fibrinolytics4) and diathermy coagulation. Postoperative elevation of the leg at 35° from the hip with the knee extended has also been shown to reduce total blood loss by 25%.5) Significant hidden blood loss has been reported in total knee replacement probably due to bleeding into tissues and hemolysis.6,7) The breach of the medullary canal using intramedullary jigs during conventional total knee replacement is postulated to cause significant blood loss during conventional total knee replacement and can also lead to extravasation of blood leading to hidden blood loss.8) Computer-assisted surgery (CAS) requires the intraoperative registration of certain key anatomical points which determine the mechanical alignment of the tibia, the femur and the lower limb, and hence define the site of the bony cuts required for implant placement. Our hypothesis was that CAS would result in lesser blood loss as it prevents the violation of femoral and tibial canals. The aim of our study was to evaluate the total and hidden blood loss in CAS and conventional surgical technique of total knee replacement. The secondary objective was to find relation of blood loss with tourniquet time.
A prospective randomized study was conducted from June 2012 to November 2013 and patients undergoing unilateral total knee replacement were included. Institute ethical clearance was taken and 57 patients with primary osteoarthritis of knee planned for unilateral TKA were randomized by computer generated randomization sequence and were allocated into one of the two groups using sealed envelopes after determining eligibility (Fig. 1). After obtaining written informed consent, 28 patients were enrolled in the conventional group (group A) and 29 patients in the CAS group (group B). Both the groups were comparable with respect to preoperative range of motion and deformity. Patients with morbid obesity (body mass index > 40 kg/m2), requiring femoral/tibial stem, having bleeding diathesis, on anticoagulant treatment and those suffering from renal disease precluding the use of enoxaparin were excluded from the study.
All patients were given tranexamic acid (15 mg/kg, slow IV infusion) 10 minutes prior to deflation of tourniquet. All surgeries were done under tourniquet, which was inflated before skin incision and deflated after cement has cured. A single surgeon (RM) carried out surgery using a uniform approach (median para-patellar), similar implant (Cruciate retaining, Columbus, Aesculap, Tuttlingen, Germany), and cement fixation (Palacos, Heraeus Kulzer GmbH, Hanau, Germany). All patients underwent general anesthesia consisting of propofol induction, vacuronium bromide to facilitate intubation and oxygen/air/isoflurane for maintenance of anesthesia. All patients (with normal renal function) were given enoxaparin subcutaneously (40 mg/4,000 U) as thromboprophylaxis, started 12 hours after surgery and continued till patient was well mobilized. Mobilization was started from the evening of surgery as per the pain tolerance of the patient. Antibiotic prophylaxis was continued till fifth postoperative day. Suction drain was removed after 48 hours of surgery.
All the bony cuts were done using conventional jigs. An extramedullary tibial jig was used to make tibial cut. An entry hole was drilled into the distal femur to gain entrance to the intramedullary canal. The medullary canal was opened up with a 9 mm drill. All cuts in femur were made by the corresponding femoral jigs. The medullary canal was closed with a bone plug fashioned from distal femoral bone cut just before the implantation of definitive components.
Orthopilot Navigation system (OrthoPilot, Aesculap) was used in all the computer-assisted navigation cases. The system works on the mechanism of imageless navigation. Transmitters were attached to the femur and tibia with 4.5 mm cortical self tapping screws and a mounting sleeve. All the cuts in the tibia as well as the femur were performed using the navigation system. The intramedullary canals of tibia and femur were not violated.
The hemoglobin (Hb) and the haematocrit (Hct) levels were measured in all the patients prior to the surgery and on the second postoperative (PO2) day. Intraoperative blood loss was assessed by weighing sponges and measuring suction volume. Postoperative blood loss was noted by measuring blood in the drain. The patient's blood volume (PBV) was calculated using the formula of Nadler et al.9) i.e., PBV = k1 × height (m)3 + k2 × weight (kg) + k3, where k is constant, whose values are, k1 = 0.3669, k2 = 0.03219, k3 = 0.6041 for men; k1 = 0.3561, k2 = 0.03308, k3 = 0.1833 for women.
Multiplying the PBV by the hematocrit gave the total red cell volume. If a transfusion was performed, a unit of red cell concentrates containing the standard 250 mL of red blood cells (RBCs) was used.
Assuming 300 mL blood loss to be clinically significant and previous studies of blood loss in drain suggesting a standard deviation (SD) of approximately 400 mL,10) the required sample size per group was determined to be 28, with alpha and beta fixed at 5% and 20%, respectively.
Data was analyzed using IBM SPSS ver. 20 (IBM Co., Armonk, NY, USA). Data was represented in mean ± SD/median (range) and frequency (percentage). Wilcoxan Rank sum test was used for comparing two groups for postoperative drain, blood transfusion, total RBC volume loss, total blood volume loss, hidden blood loss and total hemoglobin loss. For the rest of continuous variables, two groups were compared using t-test. Correlation between the two continuous variables was seen by using Karl Pearson/Spearman correlation coefficient. Categorical variables were compared using chi-square/Fisher exact test. A p-value < 0.05 was taken as statistically significant.
The two groups were not different with respect to age, gender, weight, height, comorbidities, type of anesthesia, preoperative hemoglobin and preoperative range of motion of knee and deformity (Table 1). The mean tourniquet time was 42.9 minutes in conventional group and 60 minutes in CAS group, which was clinically significant (p < 0.001). Postoperative drain volume was not significantly different (p = 0.164) in the two techniques with median (range) of 297 mL (range, 80 to 850 mL) in conventional technique and 250 mL (range, 50 to 500 mL) in computer-assisted technique. The mean total blood loss was 980 mL in conventional group and 970 mL in CAS with median of 1,067 mL (range, 59 to 1,791 mL) in conventional and 863 mL (range, 111 to 2,032 mL) in CAS group. There was no significant difference in total blood loss between the two groups (p = 0.811). Mean hidden blood loss was 54.8% of total blood loss in conventional group and 59.5% of total blood loss in CAS group (Table 2). There was no relation of tourniquet time with, intraoperative, postoperative drain, total, measured or hidden blood loss (correlation coefficient: group A, 0.217, -0.0124, -0.348, 0.225, -0.103; group B, -0.0155, -0.1127, -0.2132, -0.157, -0.101) (p-value: group A, 0.266, 0.95, 0.0694, 0.25, 0.602; group B, 0.936, 0.561, 0.267, 0.416, 0.602).
We could not found any difference in intraoperative, postoperative drain; total or hidden blood loss in CAS as compared to conventional technique. However, we found significant hidden blood loss in both the techniques of TKA. Most of previous studies in literature evaluating the effect of computer navigation on blood loss have reported significantly less blood loss in CAS as compared to the conventional surgery.8,11,12,13) Chauhan et al.8) prospectively studied 70 patients in whom blood loss was measured by drain output, reported significantly reduced blood loss with the use of navigation equipment. Kalairajah et al.11) also evaluated blood loss in drains as a primary outcome measure in 60 patients and replicated the similar findings. They have used uncemented implants and inserted 3 drains in one knee as compared to cemented implants in our study and only one drain per knee. Millar et al.12) studied 60 morbidly obese patients and reported reduced blood loss in computer navigation group. None of these studies have taken hidden blood loss into account which according to Sehat et al.7) was reported to be 49% of total blood loss in conventional TKA. McConnell et al.13) in a retrospective study analysed the data of 136 sequential patients operated by 4 different surgeons, took hidden blood loss into account and found that blood loss was significantly lower in CAS in comparison to a method employing conventional TKA. Two other recent studies have reported results similar to our study. Thiengwittayaporn et al.14) in a study comparing blood loss in minimally invasive surgery with and without computer navigation in knee arthroplasty and Mohanlal et al.15) in a retrospective non randomized study of 73 patients found no significant difference in blood loss in CAS TKA and conventional TKA. Napier et al.16) have found decreased blood loss if knee was placed in flexion for 6 hours after total knee replacement as compared to flexion for 3 hours or knee position in full extension.
We have also taken hidden blood loss into account but our findings are contradictory to the previous studies. The previous studies have attributed the cause of reduced blood loss to the fact that CAS avoids the violation of the femoral intramedullary canal. However all the previous workers have closed the femoral canal opening with bone plug similar to our study so the bleeding from femoral canal should not be an important cause of blood loss anymore. In computer-assisted navigation two pins have to be inserted in shafts of femur and tibia along with extra dissection, which can also be the potential cause of blood loss. In computer-assisted navigation surgery tourniquet time was 15 to 20 minutes longer than conventional, which would have also contributed to blood loss as tourniquet deflation has been shown to be associated with thrombolytic activity.17) Also, anoxia is believed to promote activation of the antithrombin III and protein C pathways which could cause post tourniquet bleeding.18) Therefore, the blood loss avoided by not opening the canal might be compensated by greater post tourniquet bleeding due to greater tourniquet time. The relation of tourniquet use with blood loss is debated in literature. Tai et al.19) have found association of tourniquet use with less blood loss during total knee replacement and according to meta-analysis of level 1 studies done by Parvizi and Diaz-Ledezma20) use of tourniquet leads to significant reduction in blood loss. However, Li et al.,21) concluded from meta-analysis of 14 studies comparing TKA with and without tourniquet, that the use of tourniquet during TKA may be effective for reducing intraoperative blood loss, but not for reducing the postoperative blood loss and actual total blood loss. Similarly in a recent meta-analysis Zhang et al.22) have found no effect of tourniquet on actual blood loss. Tarwala et al.23) in a study comparing tourniquet use during cementation only and use during the entire operation of TKA have found no effect on blood loss. We have also not found any relation of tourniquet time with blood loss in both CAS and conventional TKA.
All our patients received tranexamic acid 10 minutes prior to tourniquet deflation, which is shown to reduce the postoperative blood loss.24) Kalairajah et al.11) have not mentioned about the administration of tranexamic acid before surgery, and the greater blood loss in their patients could be due to its non-administration; however, McConnell et al.13) have given tranexamic acid in all their patients at the time of induction. Kalairajah et al.11) and McConnell et al.13) have used oral aspirin 150 mg for thromboprophylaxis while we have used subcutaneous enoxaparin. The mean blood volume loss in our study was 1,067 mL in conventional and 863 mL in CAS which is less than reported by previous studies as Kalairajah et al.11) reported 1,351 mL in CAS and 1,747 mL in conventional and McConnell et al.13) has reported 1,362 mL in conventional and 1,137 mL in computer-assisted technique. The lesser blood loss in our patients can be due to shorter built of Indian patients as compared to western patients and administration of tranexamic acid at appropriate timing during surgery.
The limitation of our study was small sample size; however, its strength was study design of prospective randomized study and standard operative and anesthetic protocol.
In view of significant hidden blood loss in both the techniques we suggest not to rely on amount of drain for blood loss but to repeat hemoglobin count and hematocrit count on second postoperative day. Although the previous studies have shown significant lower blood loss in the computer-assisted knee replacement surgery as compared to conventional technique, we have not found any significant difference in blood loss in the two surgical techniques.
Figures and Tables
Table 1
Baseline Variables
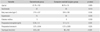
Table 2
Measurements of Blood Loss in the Two Groups
ACKNOWLEDGEMENTS
We would like to thank Mr Ashish, Department of Biostatistics, for the analysis of results.
References
1. Bierbaum BE, Callaghan JJ, Galante JO, Rubash HE, Tooms RE, Welch RB. An analysis of blood management in patients having a total hip or knee arthroplasty. J Bone Joint Surg Am. 1999; 81(1):2–10.
2. Vandenbussche E, Duranthon LD, Couturier M, Pidhorz L, Augereau B. The effect of tourniquet use in total knee arthroplasty. Int Orthop. 2002; 26(5):306–309.
3. Tria AJ Jr, Coon TM. Minimal incision total knee arthroplasty: early experience. Clin Orthop Relat Res. 2003; (416):185–190.
4. Samama CM. A direct antifibrinolytic agent in major orthopedic surgery. Orthopedics. 2004; 27:6 Suppl. s675–s680.
5. Ong SM, Taylor GJ. Can knee position save blood following total knee replacement? Knee. 2003; 10(1):81–85.
6. Sehat KR, Evans R, Newman JH. How much blood is really lost in total knee arthroplasty? Correct blood loss management should take hidden loss into account. Knee. 2000; 7(3):151–155.
7. Sehat KR, Evans RL, Newman JH. Hidden blood loss following hip and knee arthroplasty: correct management of blood loss should take hidden loss into account. J Bone Joint Surg Br. 2004; 86(4):561–565.
8. Chauhan SK, Scott RG, Breidahl W, Beaver RJ. Computer-assisted knee arthroplasty versus a conventional jig-based technique: a randomised, prospective trial. J Bone Joint Surg Br. 2004; 86(3):372–377.
9. Nadler SB, Hidalgo JH, Bloch T. Prediction of blood volume in normal human adults. Surgery. 1962; 51(2):224–232.
10. Levy O, Martinowitz U, Oran A, Tauber C, Horoszowski H. The use of fibrin tissue adhesive to reduce blood loss and the need for blood transfusion after total knee arthroplasty: a prospective, randomized, multicenter study. J Bone Joint Surg Am. 1999; 81(11):1580–1588.
11. Kalairajah Y, Simpson D, Cossey AJ, Verrall GM, Spriggins AJ. Blood loss after total knee replacement: effects of computer-assisted surgery. J Bone Joint Surg Br. 2005; 87(11):1480–1482.
12. Millar NL, Deakin AH, Millar LL, Kinnimonth AW, Picard F. Blood loss following total knee replacement in the morbidly obese: effects of computer navigation. Knee. 2011; 18(2):108–112.
13. McConnell J, Dillon J, Kinninmonth A, Sarungi M, Picard F. Blood loss following total knee replacement is reduced when using computer-assisted versus standard methods. Acta Orthop Belg. 2012; 78(1):75–79.
14. Thiengwittayaporn S, Junsee D, Tanavalee A. A comparison of blood loss in minimally invasive surgery with and without electromagnetic computer navigation in total knee arthroplasty. J Med Assoc Thai. 2009; 92:Suppl 6. S27–S32.
15. Mohanlal PK, Sandiford N, Skinner JA, Samsani S. Comparision of blood loss between computer assisted and conventional total knee arthroplasty. Indian J Orthop. 2013; 47(1):63–66.
16. Napier RJ, Bennett D, McConway J, et al. The influence of immediate knee flexion on blood loss and other parameters following total knee replacement. Bone Joint J. 2014; 96(2):201–209.
17. Murphy CG, Winter DC, Bouchier-Hayes DJ. Tourniquet injuries: pathogenesis and modalities for attenuation. Acta Orthop Belg. 2005; 71(6):635–645.
18. Petaja J, Myllynen P, Myllyla G, Vahtera E. Fibrinolysis after application of a pneumatic tourniquet. Acta Chir Scand. 1987; 153(11-12):647–651.
19. Tai TW, Chang CW, Lai KA, Lin CJ, Yang CY. Effects of tourniquet use on blood loss and soft-tissue damage in total knee arthroplasty: a randomized controlled trial. J Bone Joint Surg Am. 2012; 94(24):2209–2215.
20. Parvizi J, Diaz-Ledezma C. Total knee replacement with the use of a tourniquet: more pros than cons. Bone Joint J. 2013; 95:11 Suppl A. 133–134.
21. Li X, Yin L, Chen ZY, et al. The effect of tourniquet use in total knee arthroplasty: grading the evidence through an updated meta-analysis of randomized, controlled trials. Eur J Orthop Surg Traumatol. 2014; 24(6):973–986.
22. Zhang W, Li N, Chen S, Tan Y, Al-Aidaros M, Chen L. The effects of a tourniquet used in total knee arthroplasty: a meta-analysis. J Orthop Surg Res. 2014; 9(1):13.
23. Tarwala R, Dorr LD, Gilbert PK, Wan Z, Long WT. Tourniquet use during cementation only during total knee arthroplasty: a randomized trial. Clin Orthop Relat Res. 2014; 472(1):169–174.
24. Irisson E, Hemon Y, Pauly V, Parratte S, Argenson JN, Kerbaul F. Tranexamic acid reduces blood loss and financial cost in primary total hip and knee replacement surgery. Orthop Traumatol Surg Res. 2012; 98(5):477–483.




 PDF
PDF ePub
ePub Citation
Citation Print
Print



 XML Download
XML Download