Abstract
Background
The purpose of this study was to compare the results of Aescula and TomoFix plates used for biplanar open wedge high tibial osteotomy in medial osteoarthritis of the knee joint with varus deformity.
Methods
A consecutive series of 50 cases of biplanar open wedge high tibial osteotomy were evaluated retrospectively. Group A contained 25 cases treated by using the Aescula plate, and group T contained 25 cases treated by using the TomoFix plate. Full weight-bearing was permitted at 6 weeks after surgery in group A and at 2 weeks in group T. Clinical evaluations were performed at the final follow-up by using postoperative knee scores and functional scores. Radiographic analysis included postoperative mechanical femur-tibia angle, change in posterior tibial slope angle, and complications related to implants. The mean follow-up periods were 30 months in group A and 26 months in group T.
Results
The knee and functional scores were improved at the final follow-up in both groups (p < 0.05), but no differences were observed between the two groups (p > 0.05). An acceptable correction angle was obtained in 52% of group A and in 84% of group T (p = 0.015). Change in posterior tibial slope angle was larger in group A than in group T (p < 0.001), showing better maintenance of posterior tibial slope in group T. In group A, there were 3 cases of screw loosening and 4 cases of delayed union. In addition, there were residual varus deformities in 7 cases (6 in group A and 1 in group T).
High tibial osteotomy (HTO) is one of the treatments for unicompartmental osteoarthritis of the knee joint, and it can be performed by open wedge, closed wedge, or dome osteotomy. Open wedge HTO is now popular, because it offers accurate correction of angle, restoration of the knee joint stability, and preservation of the fibula.1,2) The fixation instruments used for medial open wedge HTO are as follows: a spacer plate such as the Puddu plate (Arthrex, Naples, FL, USA) or the Aescula plate (B. Braun Korea, Seoul, Korea); or a plate fixator like the TomoFix plate (Synthes, Solothan, Swiss) (Fig. 1).3) The former has the advantages of having a small, low profile and a limited incision of soft tissue; but, it has the disadvantages of having longer period of non-weight-bearing (six weeks after surgery),4,5) frequent complications due to difficult maintenance of correction angle during the bone healing period, non-union, fixator failure,6,7,8) and increased posterior tibial slope.9) On the other hand, the latter offer the advantages of having rigid fixation, early range of motion, early weight-bearing (two weeks after surgery),10) and maintenance of a normal preoperative posterior tibial slope;9,10,11,12) but, it has the disadvantage of having more extensive skin and soft tissue incisions.
This study was hypothesized that the clinical and radiological outcomes and complications after medial open wedge HTO for a spacer plate group and a plate fixator group would be similar, despite the above-mentioned advantages and disadvantages. Accordingly, the present study was undertaken to evaluate the clinical and radiologic outcomes and complications occuring after biplanar medial open wedge HTO by using the Aescula plate or the TomoFix plate in medial osteoarthritis of the knee joint with varus deformity.
Approval of the Ethics Committee of the Institutional Review Board (IRB) was obtained for this retrospective study (IRB number: 2013-08-008). A consecutive series of 50 cases of biplanar open wedge HTOs were evaluated in 48 patients who were treated from February 2006 to February 2011. Group A was composed of 25 cases (24 patients) treated by using the Aescula plate, and group T was composed of 25 cases (24 patients) treated by using the TomoFix plate. There was no guideline to decide which plate would be applied. In Kyungpook National University Hospital, Aescula plate was introduced earlier than the TomoFix plate. So, Aescula plate group was the earlier one, and TomoFix plate group was the later one. Inclusion criteria were symptomatic medial osteoarthritis of the knee joint, varus limb alignment, and an intact lateral joint compartment. Exclusion criteria were active infection on the knee joint, severe osteoarthritis of the patellofemoral joint, and flexion contracture of > 15° or flexion < 90°. Demographic features such as age, gender, preoperative varus deformity, and body mass index did not differ significantly between the two groups.
Preoperative mechanical femoral-tibial angles (mFTAs) were measured using anteroposterior full-leg length radiographs that were taken while the patients were standing on both legs and the knee joint were in full extension. Target correction angle was measured at the point where the mechanical axis of the lower limb passed through the Fugisawa point, which is 62.5% from the medial tibial articular margin. All cases underwent diagnostic arthroscopy and debridement of articular cartilage and/or partial meniscectomy.
A longitudinal skin incision was placed at the medial side (~5 cm) of the tibial tuberosity. The superficial medial collateral ligament (MCL) and the pes anserinus were completely released below the osteotomy site. Biplanar osteotomy, which is horizontal oblique osteotomy parallel to the tibial slope targeting the tip of the fibular head, and oblique coronal osteotomy at 130° to the horizontal oblique osteotomy was performed.6) After completing biplanar osteotomy, the osteotomy site was spread with a bone chisel and a laminar spreader until the cable line connecting the hip center to the ankle center passed through the Fugisawa point.13) Then, under fluoroscopic guidance, the osteotomy site was fixed to each plate. If the cable line, mechanical axis of the limb, passed through 62% to 66% of the tibial width from the medial tibial articular margin, the correction amount was accepted.14) The osteotomy gap was filled with allograft chip bone mixed with autologous bone marrow. The bone graft site was then covered with detached superficial MCL, and the pes anserinus was reattached to periosteum. Active range of motion was started 2 weeks after surgery in both groups, but full weight-bearing was started at 6 weeks in group A and at 2 weeks in group T.
Final evaluations were performed by using American Knee Society knee and function scores, mFTAs, and changes in posterior tibial slope angle (pTSA). The acceptable range of mFAT was valgus 3° to 6°, and under- and overcorrections were evaluated.15) Posterior tibial slope was measured between the medial tibial plateau and the posterior tibial cortex.16,17) Complications associated with the implants were also evaluated.
The statistical analysis was done using chi-square test to make comparison between the proportion of two groups in IBM SPSS ver. 19 (IBM Co., Armonk, NY, USA); and statistical significance was accepted for p-values < 0.05. To compare between the mean of two groups, we used Mann-Whitney U-test which is nonparametric test, as cases were small and could not satisfy normal.
Knee and function scores significantly improved after osteotomy (p = 0.001), but no significant difference was found between the A and T groups (p > 0.05) (Table 1). At the final follow-up, mean mFTAs during weight-bearing showed more valgus correction in the group T (3.4° vs. 1.7°). An acceptable correction angle was obtained in 52% of group A and in 84% of group T (p = 0.015). Undercorrection at the final follow-up was observed in 44% of group A and in 8% of group T, and overcorrection was observed in 4% of group A and in 8% of group T (Table 2). Residual varus deformity (mFTA < 0°) after osteotomy was present in 7 cases: 6 cases (3.5° varus) in group A and 1 case (1.7° varus) in group T. Preoperative varus deformity was 11.7° ± 2.3° in group A and 10° in group T. Four cases in group A and one case in group T with postoperative varus deformity showed severe deformation (mFTA > 10°).
pTSA was increased at the final follow-up in both groups: 72% in group A and 52% in group T (p = 0.244). The increase in pTSA was greater in group A than in group T (p = 0.016). Furthermore, the change of pTSA was larger in group A than in group T (p < 0.001), which indicates better posterior tibial slope maintenance in group T. A change in slope ≥ 5° was observed in 11 cases in group A and in a case in group T (p = 0.001) (Table 2).
In group A, there were three cases of screw loosening (Fig. 2) and 4 cases of delayed union at > 6 months after surgery (Fig. 3). The other 46 cases achieved bone union at 3 months after osteotomy. Finally, skin irritation attributed to the larger TomoFix plate, which occurred in one case in group T.
The present study shows that better and acceptable correction of the mFTA was achieved in the TomoFix plate group. Furthermore, pTSAs were better maintained, and the complication rate was lower in the TomoFix group.
Pape et al.3) reported of a 30-subject clinical trial, where the subjects underwent open wedge-HTO by using a spacer plate or plate fixator, and the fixation stability was assessed over a 2-year period by radiostereometric analysis (RSA). Postoperative RSA data showed significantly higher lateral translation of the distal tibia and significantly more subsidence, varus, and internal rotation of the tibial head in the spacer plate group than in the plate fixator group. Furthermore, weight-bearing following spacer plate fixation induced significant micro-motion at 6 weeks after surgery. The authors concluded that early weight-bearing is appropriate for plate fixator fixation, and that spacer plate fixation should be prolonged for up to 8-10 weeks to avoid pseudoarthrosis and/or the recurrence of varus angulation. Spahn8) reported that a Puddu spacer plate group showed higher incidence of hematoma, infection, and implant failure rates, and they needed longer rehabilitation period than the plate fixator group. Staubli and Jacob18) and Zaki and Rae19) reported of good bone healing without bone graft or substitute in a TomoFix plate group. Asada et al.9) reported of an increase in posterior tibial slope after open wedge-HTO and suggested that this increase was possibly caused by coronal correction loss when a spacer plate fixator was used. They found that it was necessary to fix anterior and posterior gaps separately. The correction angle in coronal plane had a trade-off relationship with the changes in posterior tibial slope. However, TomoFix plate was possible for rigid fixation, early range of motion, weight-bearing, and maintenance of posterior tibial slope.
In the present study, full weight-bearing was allowed at 6 weeks after surgery in group A, but at 2 weeks in group T. In group A, screw loosening occurred in 3 cases and delayed union occurred in 4 cases. In group T, skin irritation related to the plate occurred in 1 case, and no other complication related to bone union or the plate was observed; and bone union was obtained at 3 months after surgery. Furthermore, the under-correction rate of mFTA was greater in group A. The maximum space thickness of the Aescula plate was 13 mm, and it was difficult to achieve an acceptable angle in the cases with > 10° of varus deformity. When a mFTA of > 3° valgus was required, a posterior gap opening of > 13 mm was necessary, but no suitable larger Aescula plate was available. The TomoFix plate enabled the corrections of deformities exceeding 20°.20)
In a previous study on pTSA, changes in pTSA of < 5° were not clinically significant in the femoral-tibial position.21,22) In the present study, a change in slope of ≥ 5° was observed in 11 cases in group A and in 1 case in group T. pTSA was higher in group A at the final follow-up, which was presumed to be due to the Aescula plate or some technical issue. To adequately maintain the posterior tibial slope, the opening ratio of the anterior to posterior gap should be 1 to 2.14) In order to achieve this ratio, the knee joint should be at an extended position after osteotomy. The placement of an Aescula spacer plate in posterior aspect adequately prevented closure of the intended anterior gap, and posterior tibial slope was increased. Furthermore, we believe that under-correction in the coronal plane in the cases of severe varus deformity increased posterior tibial slope, as described by Asada et al.9) However, posterior tibial slope control in the sagittal plane was easier during TomoFix plate fixation. A single screw was fixed in the distal plate after fixing proximal screws, and the knee joint was then placed in the extended position to adjust posterior tibial slope under fluoroscopy guidance; and fixation was completed by inserting a screw in the remaining distal hole.
Screw loosening occurred in 3 cases in group A. We attribute this to postmenopausal osteoporosis, the low profile plate, and the non-locking nature of the Aescula plate, whereas the TomoFix plate is a locking plate. Thus, we suggest that the bone mineral density of the proximal tibial metaphysis can be determined preoperatively. Nevertheless, we would expect to see favorable results after open wedge HTO, when a plate fixator such as the TomoFix plate is used in the cases of severe varus deformity or with a weak tibial metaphysis.
Several limitations of the present study require consideration. In particular, this study is limited by its retrospective design, small cohort, and short follow-up period. Thus, we suggest that further larger-scale studies should be conducted with a longer follow-up period to explore further possible relations between these plate types and clinical results. In addition, we did not evaluate tibial bone density preoperatively, which could have reduced complications like screw loosening. This study shows that firm fixation using a TomoFix plate for open wedge HTO produces better radiologic results and a low complication rate, than the shorter Aescula spacer plate.
Figures and Tables
 | Fig. 3Delayed union was observed in the Aescula plate group: (A) immediately after surgery, (B) at 3 months postoperatively, (C) at 5 months postoperatively, (D) at 9 months postoperatively, (E) at 14 months postoperatively, and (F) at 20 months postoperatively. |
Table 1
American Knee Society Knee and Function Scores
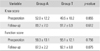
Table 2
Mechanical Axis and Tibial Slope Changes after Surgery

ACKNOWLEDGEMENTS
This research was supported by the Kyungpook National University Research Fund, 2012.
References
1. Hofmann AA, Kane KR. Total knee arthroplasty after high tibial osteotomy. Orthopedics. 1994; 17(9):887–890.
2. Keene JS, Dyreby JR Jr. High tibial osteotomy in the treatment of osteoarthritis of the knee: the role of preoperative arthroscopy. J Bone Joint Surg Am. 1983; 65(1):36–42.
3. Pape D, Kohn D, van Giffen N, Hoffmann A, Seil R, Lorbach O. Differences in fixation stability between spacer plate and plate fixator following high tibial osteotomy. Knee Surg Sports Traumatol Arthrosc. 2013; 21(1):82–89.
4. Brinkman JM, Lobenhoffer P, Agneskirchner JD, Staubli AE, Wymenga AB, van Heerwaarden RJ. Osteotomies around the knee: patient selection, stability of fixation and bone healing in high tibial osteotomies. J Bone Joint Surg Br. 2008; 90(12):1548–1557.
5. van den Bekerom MP, Patt TW, Kleinhout MY, van der Vis HM, Albers GH. Early complications after high tibial osteotomy: a comparison of two techniques. J Knee Surg. 2008; 21(1):68–74.
6. Lobenhoffer P, Agneskirchner JD. Improvements in surgical technique of valgus high tibial osteotomy. Knee Surg Sports Traumatol Arthrosc. 2003; 11(3):132–138.
7. Schroter S, Gonser CE, Konstantinidis L, Helwig P, Albrecht D. High complication rate after biplanar open wedge high tibial osteotomy stabilized with a new spacer plate (Position HTO plate) without bone substitute. Arthroscopy. 2011; 27(5):644–652.
8. Spahn G. Complications in high tibial (medial opening wedge) osteotomy. Arch Orthop Trauma Surg. 2004; 124(10):649–653.
9. Asada S, Akagi M, Mori S, Matsushita T, Hashimoto K, Hamanishi C. Increase in posterior tibial slope would result in correction loss in frontal plane after medial open-wedge high tibial osteotomy. Knee Surg Sports Traumatol Arthrosc. 2012; 20(3):571–578.
10. Brinkman JM, Luites JW, Wymenga AB, van Heerwaarden RJ. Early full weight bearing is safe in open-wedge high tibial osteotomy. Acta Orthop. 2010; 81(2):193–198.
11. Niemeyer P, Schmal H, Hauschild O, von Heyden J, Sudkamp NP, Kostler W. Open-wedge osteotomy using an internal plate fixator in patients with medial-compartment gonarthritis and varus malalignment: 3-year results with regard to preoperative arthroscopic and radiographic findings. Arthroscopy. 2010; 26(12):1607–1616.
12. Takeuchi R, Ishikawa H, Aratake M, et al. Medial opening wedge high tibial osteotomy with early full weight bearing. Arthroscopy. 2009; 25(1):46–53.
13. Fujisawa Y, Masuhara K, Shiomi S. The effect of high tibial osteotomy on osteoarthritis of the knee: an arthroscopic study of 54 knee joints. Orthop Clin North Am. 1979; 10(3):585–608.
14. Noyes FR, Barber SD, Simon R. High tibial osteotomy and ligament reconstruction in varus angulated, anterior cruciate ligament-deficient knees: a two- to seven-year follow-up study. Am J Sports Med. 1993; 21(1):2–12.
15. Hernigou P, Medevielle D, Debeyre J, Goutallier D. Proximal tibial osteotomy for osteoarthritis with varus deformity: a ten to thirteen-year follow-up study. J Bone Joint Surg Am. 1987; 69(3):332–354.
16. Matsuda S, Miura H, Nagamine R, et al. Posterior tibial slope in the normal and varus knee. Am J Knee Surg. 1999; 12(3):165–168.
17. Yoshioka Y, Siu DW, Scudamore RA, Cooke TD. Tibial anatomy and functional axes. J Orthop Res. 1989; 7(1):132–137.
18. Staubli AE, Jacob HA. Evolution of open-wedge high-tibial osteotomy: experience with a special angular stable device for internal fixation without interposition material. Int Orthop. 2010; 34(2):167–172.
19. Zaki SH, Rae PJ. High tibial valgus osteotomy using the Tomofix plate: medium-term results in young patients. Acta Orthop Belg. 2009; 75(3):360–367.
20. Staubli AE, De Simoni C, Babst R, Lobenhoffer P. TomoFix: a new LCP-concept for open wedge osteotomy of the medial proximal tibia: early results in 92 cases. Injury. 2003; 34:Suppl 2. B55–B62.
21. Dejour H, Walch G, Neyret P, Adeleine P. Dysplasia of the femoral trochlea. Rev Chir Orthop Reparatrice Appar Mot. 1990; 76(1):45–54.
22. Giffin JR, Vogrin TM, Zantop T, Woo SL, Harner CD. Effects of increasing tibial slope on the biomechanics of the knee. Am J Sports Med. 2004; 32(2):376–382.




 PDF
PDF ePub
ePub Citation
Citation Print
Print




 XML Download
XML Download