Abstract
Background
Approximately 10% of patients with osteoarthritis (OA) of the knee have unicompartmental OA confined to the patellofemoral joint (PFJ). The main surgical options are total knee replacement (TKR) and PFJ replacement (PFJR). PFJR has a number of advantages over TKR, including being less invasive, preserving the unaffected parts of the knee, allowing faster recovery and better range of motion and function. We report our prospective mid-term results of the Avon PFJR for established isolated PFJ arthritis in 61 consecutive procedures.
Methods
Sixty-one Avon PFJRs were performed in 57 patients. The outcome measures were the new Oxford knee score (OKS), Hungerford and Kenna score (HKS), and Crosby Insall knee scores. Only patients with severe isolated PFJ OA were included. The diagnosis was based on a combination of clinical, radiological and, where available, arthroscopic findings.
Results
Mean follow-up was 5.09 years (range, 12 to 124 years). There were 2 revisions in the first 5 years. The median HKS score was 80 (interquartile range, 70 to 95) and the mean OKS was 31.8 (± standard deviation, 8.7) at 5 years. These were significantly better (p < 0.001) than the preoperative scores.
Approximately 10% of patients with osteoarthritis (OA) of the knee have unicompartmental disease confined to the patellofemoral joint (PFJ). These patients are typically younger and predominantly female.1) Although the pathophysiology is multifactorial, the final common pathway is believed to be the result of abnormal load across the PFJ.2) Patients often complain of anterior knee pain particularly when going up or down stairs, standing from a seated position and on kneeling. In many cases there is no obvious cause, although in younger patients there may be specific risk factors such as recurrent patellar dislocation, trauma or trochlear dysplasia.3)
Initial treatment of patellofemoral OA (PFOA) may be conservative, but in more severe cases a number of operative strategies have been tried. These include arthroscopic procedures, such as chondroplasty, microfracture and lateral release; attempts at restoring the articular surface by autologous cartilage reimplantation; and tibial tubercle transfer/advancement. However, none of these has produced consistent results.4) The remaining options are total knee replacement (TKR) and PFJ replacement (PFJR). Many surgeons feel that TKR is excessive as it involves resurfacing a normal tibiofemoral joint. PFJR has a number of advantages over TKR, including preservation of the unaffected parts of the knee and maintenance of normal knee biomechanics, potentially allowing faster recovery and better range of motion and function.5)
The majority of literature pertaining to second generation PFJR relates to the Avon PFR (Stryker, Howmedica Osteonics, Allendale, NJ, USA). The patellar component is manufactured from ultra-high-molecular-weight polyethylene with a 3 mm medially offset dome to facilitate tracking and optimise patella stability. The femoral component has a broad, symmetrical trochlear flange that narrows distally, ensuring patellar engagement during flexion whilst allowing it to be relatively unconstrained in extension
There have been a number of published series, both from the Bristol Knee Group (originating centre) and from other authors. Ackroyd et al.6) described 95.8% survivorship at 5 years and significant improvements in pain and function with low complication rates in 83 consecutive PFRs. Odumenya et al.7) reported 50 knees with 100% survivorship at 5 years, and similarly favourable clinical outcomes. We present our independent experience of the Avon implant in 61 consecutive PFRs followed up to a maximum of 10 years.
A prospective series of 61 consecutive Avon PFRs were performed in 57 patients between November 2001 and April 2011. Patients with bilateral procedures had each replacement treated as a separate event for statistical purposes. There were 6 men and 51 women with a mean age of 66.1 years (± standard deviation [SD], 10.1 years). Only patients with severe isolated PFJ OA were deemed suitable for this procedure. The diagnosis was based on a combination of clinical, radiological and, where available, arthroscopic findings. Arthroscopy was performed primarily in younger patients to help determine whether to treat them with a PFR, tibial tubercle transfer or other less invasive procedure. Preoperatively, every patient underwent weight-bearing anteroposterior, lateral and skyline radiographs at 30° of flexion. Exclusion criteria were fixed flexion deformity of greater than 10°, localised chondral lesions greater than 10 mm in areas other than the PFJ surface, or general attrition of the articular cartilage at arthroscopy. These factors have been shown to be early signs of progressive disease.8) Generally speaking, any areas of grade 4 OA in areas other than the PFJ, according to the Outerbridge grading system, was considered a contraindication to PFR. Seventeen patients had had previous surgery (Table 1). All procedures were performed by, or under the direct supervision of, the senior author (PABM), using the medial parapatellar technique previously described by Ackroyd and Chir.5)
Patients were initially assessed preoperatively, and subsequently underwent postoperative follow-up at 6 weeks, 6 months, and then annually in a research clinic where they were seen by either an independent research physiotherapist or a doctor, who was not involved with the procedure. Data collected included prosthesis survivorship, using revision as the end point, and functional outcome as measured using the new Oxford knee score (OKS),9) the Hungerford and Kenna score (HKS),10) and the Crosby and Insall knee score (CIKS).11) Patient satisfaction with the outcome of surgery was also documented. The new OKS is a 48 point score with each question being scored from 0 to 4, with 4 representing the best outcome/least symptoms. Scores are added so the overall score is from 0 to 48 with 48 being the best outcome. The HKS includes assessment of pain, level of function, range of motion, and quadriceps strength. Subtractions from the score are due to patellar apprehension, effusions, and painful crepitus. Excellent results were regarded as being 90-100, good results 80-89, fair results 70-79, and poor results as less than 70. The CIKS is a scoring system exclusively for the PFJ and designed to assess the response of patients to patellar stabilisation surgery, although not specifically to assess PFR. It is a subjective score where knees are graded as excellent, good, fair or worse. Patients were also asked whether their symptoms were better, unchanged or worse following PFR, and if they felt the surgery had been worthwhile. The results were entered into a database and a Kaplan-Meier curve constructed.
The analysis was carried out using STATA ver. 12 (StataCorp LP, College Station, TX, USA) by an independent statistician. Kaplan Meier methods were used to estimate time to revision. HKS were summarised as medians and were compared using nonparametric tests (Mann-Whitney and Wilcoxan signed ranks) as the data did not follow a normal distribution. The new OKS data were normally distributed and therefore summarised using means with comparisons made using paired or unpaired t-tests.
Patients were followed up for a mean of 5.09 years (range, 12 to 124 years). Four patients (4 knees) underwent revision to a TKR. Four patients (4 knees) had died from unrelated causes, and two patients (2 knees) were lost to follow-up, giving a total of 90% of cases still under ongoing active follow-up.
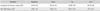
The functional outcome scores are shown in Figs. 1 and 2. They illustrate a substantial improvement in both the HKS and OKS over the follow-up period.Table 2 shows the mean HKS and OKS at baseline, 6 weeks, 1 year, and 5 years. When comparing the baseline data with the postoperative scores at 6 weeks, 1 year, and 5 years, there was a significant improvement in all cases (p < 0.001) using the Wilcoxon signed ranks test and the paired t-test. The results of CIKS demonstrate that the majority of patients subjectively had a good to excellent outcome following surgery, as well as a good range of motion. Eighty percent (49 patients) had a subjectively good/excellent outcome, 16% (10 patients) had a fair outcome, and 4% (2 patients) had a poor outcome subjectively.
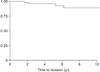
Of the 4 revisions that took place, 2 were in the first five years giving a survivorship of 96.3% (Fig. 3), with 30 knees at risk at five years (Table 3). Three of the revisions were undertaken for disease progression involving either the medial or lateral compartments. In the fourth, the indication was patellar maltracking not responsive to conservative measures. In addition, one patient had an arthroscopy for a degenerate meniscal tear. One had developed a lateral patellar osteophyte, which is being managed conservatively. Another patient had some heterotrophic ossification, which was excised from the superolateral aspect of the patella. There have been no cases of infection.
PFR was first performed by McKeever12) in 1955 using a vitallium prosthesis screwed onto the patella. However, it was not until the 1970s that a number of newer designs gave better short-term results.13,14) Although an improvement, there were still complications including progression of arthritis in the medial or lateral compartments requiring revision to TKR. In 2001, Tauro et al.15) reported such progression in 8% of patients at 8 years, and similar progression was found in 23% of patients at 15 years by Kooijman et al.16) However, Smith et al.17) have suggested this could be due to poor patient selection, reporting that 6 of 8 patients with preoperative medial compartment OA had unsatisfactory results or required early revision following a Lubinus PFR. Kooijman et al.16) also reported good or excellent functional results in 86% of residual cases at 15 years. These findings are similar to those of Cartier et al.8) who reported an excellent functional outcome in 77% of patients with a mean follow-up of 10 years. However, these results do not match those obtained following TKR.
Our results suggest that good medium-term functional outcome can be achieved with the Avon PFR, with 30 knees at risk in our series at 5 years. These results are comparable to previous studies, including the original designer study as well as several others.6,8,18) Our series is the largest to date from an independent centre.
The postoperative functional outcome scores showed substantial improvements at 5 years. The median HKS was 80 (interquartile range [IQR], 70 to 95). The new OKS was 33 (IQR, 26 to 37) compared with 39 (IQR, 24 to 45) achieved in the original study8) and 30.5 (IQR, 22.25 to 42.25) in a subsequent independent series.6) However, our new OKS was still satisfactory by the criteria of the original study, where a successful result was defined as an OKS > 25 points. There were only 2 cases of patellar maltracking and lateral subluxation in our series. The first patient underwent revision to a TKR after 2 years, and the second is still being managed conservatively 9 years postoperatively. Previous studies have similarly reported a low incidence of patellar maltracking and subluxation.6,8) This low incidence of subluxation is most likely due to the symmetrical trochlear flange that narrows distally ensuring the patella engages during flexion but remains relatively unconstrained in extension.5)
Although our survivorship at 5 years was 96.3%, compared with 95.8% in the initial series8) and 100% in the series by Odumenya et al.,7) there have been a total of 4 revisions to date. The revisions occurred at 1.7, 2.2, 5.3, and 6.2 years after the initial replacement. The first revision was for progression to medial compartment OA and the second was for patellar maltracking. The subsequent revisions were for progression to lateral compartment and medial compartment OA, respectively. Looking at the National Joint Registry of England and Wales,19) PFR still accounts for only 1% of all knee replacements. The Avon remains the market leader, accounting for 40% of all PFRs, with a 5-year revision rate of 7.76% compared with 9.51% when looking at the overall revision rate in all PFRs. These revision data are also comparable with the 7.24% rates seen at 5 years following unicondylar tibiofemoral replacement.
In the past, TKR was the gold standard for isolated PFJ OA, as demonstrated by numerous studies. In 2007, Meding et al.20) reported on a series of 33 TKRs performed for isolated PFJ OA in patients with a mean age of 52. There were no revisions or reoperations at a mean follow up of 6.2 years, with a mean Knee Society Score (KSS) of 88. In 2002, Mont et al.21) reported on a series of 30 TKRs in 27 patients with a mean age of 73. There were no reported revisions or reoperations and all but one case had good or excellent results with a KSS over 80. However, these studies did not look at the consequences of TKR in the younger patient nor the problems associated with subsequent revisions. PFR does have a number of advantages over TKR, making it an attractive procedure for patients with isolated PFOA in whom other treatments have failed. The kinematic profile more closely resembles the normal knee with the preservation of both cruciate ligaments as opposed to TKR where at least one cruciate ligament is sacrificed.22) Furthermore, the normal tibio-femoral joint and bone stock are preserved. It is also a somewhat less invasive procedure than TKR with potentially less dissection and expected blood loss, which may contribute to a shorter length of stay and faster rehabilitation. If later required, conversion to a TKR is relatively straightforward23) and some authors have suggested that the overall outcome does not appear to be compromised as a consequence of the initial PFJR.24) This is particularly important in younger patients who present with isolated PFOA, where it is known that revision rates for TKR are higher.2)
It is acknowledged that there are some limitations to this study. The fact that more than one surgeon undertook the procedures, albeit under supervision from the senior author, reduces the homogeneity of the series, and we are also aware that some in our group have had relatively short follow-up. Additionally, we recognise that, as with all survivorship data, the decision to undertake revision surgery is a highly subjective one. Nevertheless, we believe that our results support the use of the Avon prosthesis in selected patients, with potentially favourable medium-term functional outcomes and survivorship data. Although there are 10 years of functional outcome survivorship data available, there are currently not enough patients in this cohort to draw meaningful conclusions. We continue to review this series prospectively and intend to report longer term results in the future.
Figures and Tables
Fig. 1
Box plot showing the distribution of the Hungerford and Kenna score (HKS) over time. This demonstrates an improvement in the HKSs over the first five years. Pre: presurgery.

Fig. 2
Distribution of the mean (95% confidence interval) Oxford knee score (OKS) with time. This demonstrates an improvement in the new OKS over the first five years. Pre: presurgery.
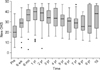
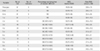
Table 1
Previous Surgery in the 61 Avon Patellofemoral Replacements

| Previous surgery | No. of knees (%) |
|---|---|
| Arthroscopy | 15 (25.0) |
| Partial medial menisectomy | 1 (1.5) |
| Tibial tubercle transfer, MUA and arthroscopy | 1 (1.5) |
| Nil | 44 (72.0) |
| Total | 67 (100) |
Table 2
Functional Outcome Scores Over Time
| Variable | Baseline | 6 wk | 1 yr | 5 yr |
|---|---|---|---|---|
| Hungerford and Kenna, median (IQR) | 40 (25-55) | 60 (45-75) | 95 (85-95) | 80 (70-95) |
| New OSK (mean±SD) | 20.8±7.9 | 28.6±7.9 | 36.4±10.3 | 31.8±8.7 |
Table 3
Life-Table of Survivorship at Ten Years for Revision Arthroplasty Data
References
1. Davies AP, Vince AS, Shepstone L, Donell ST, Glasgow MM. The radiologic prevalence of patellofemoral osteoarthritis. Clin Orthop Relat Res. 2002; (402):206–212.
2. Leadbetter WB. Patellofemoral arthroplasty in the treatment of patellofemoral arthritis: rationale and outcomes in younger patients. Orthop Clin North Am. 2008; 39(3):363–380.
3. Grelsamer RP, Dejour D, Gould J. The pathophysiology of patellofemoral arthritis. Orthop Clin North Am. 2008; 39(3):269–274.
4. Mihalko WM, Boachie-Adjei Y, Spang JT, Fulkerson JP, Arendt EA, Saleh KJ. Controversies and techniques in the surgical management of patellofemoral arthritis. Instr Course Lect. 2008; 57:365–380.
5. Ackroyd CE, Chir B. Development and early results of a new patellofemoral arthroplasty. Clin Orthop Relat Res. 2005; (436):7–13.
6. Ackroyd CE, Newman JH, Evans R, Eldridge JD, Joslin CC. The Avon patellofemoral arthroplasty: five-year survivorship and functional results. J Bone Joint Surg Br. 2007; 89(3):310–315.
7. Odumenya M, Costa ML, Parsons N, Achten J, Dhillon M, Krikler SJ. The Avon patellofemoral joint replacement: five-year results from an independent centre. J Bone Joint Surg Br. 2010; 92(1):56–60.
8. Cartier P, Sanouiller JL, Khefacha A. Long-term results with the first patellofemoral prosthesis. Clin Orthop Relat Res. 2005; (436):47–54.
9. Dawson J, Fitzpatrick R, Murray D, Carr A. Questionnaire on the perceptions of patients about total knee replacement. J Bone Joint Surg Br. 1998; 80(1):63–69.
10. Arciero RA, Toomey HE. Patellofemoral arthroplasty: a three- to nine-year follow-up study. Clin Orthop Relat Res. 1988; (236):60–71.
11. Crosby EB, Insall J. Recurrent dislocation of the patella: relation of treatment to osteoarthritis. J Bone Joint Surg Am. 1976; 58(1):9–13.
12. McKeever DC. Patellar prosthesis: 1955. Clin Orthop Relat Res. 2002; (404):3–6.
13. Blazina ME, Fox JM, Del Pizzo W, Broukhim B, Ivey FM. Patellofemoral replacement. Clin Orthop Relat Res. 1979; (144):98–102.
14. Lubinus HH. Patella glide bearing total replacement. Orthopedics. 1979; 2(2):119–127.
15. Tauro B, Ackroyd CE, Newman JH, Shah NA. The Lubinus patellofemoral arthroplasty: a five- to ten-year prospective study. J Bone Joint Surg Br. 2001; 83(5):696–701.
16. Kooijman HJ, Driessen AP, van Horn JR. Long-term results of patellofemoral arthroplasty: a report of 56 arthroplasties with 17 years of follow-up. J Bone Joint Surg Br. 2003; 85(6):836–840.
17. Smith AM, Peckett WR, Butler-Manuel PA, Venu KM, d'Arcy JC. Treatment of patello-femoral arthritis using the Lubinus patello-femoral arthroplasty: a retrospective review. Knee. 2002; 9(1):27–30.
18. Starks I, Roberts S, White SH. The Avon patellofemoral joint replacement: independent assessment of early functional outcomes. J Bone Joint Surg Br. 2009; 91(12):1579–1582.
19. National Joint Registry. National Joint Registry for England and Wales: 9th annual report 2012 [Internet]. Hemel Hempstead, UK: National Joint Registry;c2014. cited 2015 Jan 14. Available from: http://www.njrcentre.org.uk/njrcentre/Portals/0/Documents/England/Reports/9th_annual_report/NJR%209th%20Annual%20Report%202012.pdf.
20. Meding JB, Wing JT, Keating EM, Ritter MA. Total knee arthroplasty for isolated patellofemoral arthritis in younger patients. Clin Orthop Relat Res. 2007; 464:78–82.
21. Mont MA, Haas S, Mullick T, Hungerford DS. Total knee arthroplasty for patellofemoral arthritis. J Bone Joint Surg Am. 2002; 84(11):1977–1981.
22. Hollinghurst D, Stoney J, Ward T, Pandit H, Beard D, Murray DW. In vivo sagittal plane kinematics of the Avon patellofemoral arthroplasty. J Arthroplasty. 2007; 22(1):117–123.
23. Argenson JN, Guillaume JM, Aubaniac JM. Is there a place for patellofemoral arthroplasty? Clin Orthop Relat Res. 1995; (321):162–167.
24. Lonner JH, Jasko JG, Booth RE Jr. Revision of a failed patellofemoral arthroplasty to a total knee arthroplasty. J Bone Joint Surg Am. 2006; 88(11):2337–2342.




 PDF
PDF ePub
ePub Citation
Citation Print
Print


 XML Download
XML Download