Abstract
Background
In daily clinical practice, it is essential to properly evaluate the postoperative sliding distance of various femoral head fixation devices (HFD) for trochanteric fractures. Although it is necessary to develop an accurate and reproducible method that is unaffected by inconsistent postoperative limb position on radiography, few studies have examined which method is optimal. Therefore, the purpose of this study is to prospectively compare the accuracy and reproducibility of our four original methods in the measurement of sliding distance of the HFD.
Methods
Radiographs of plastic simulated bone implanted with Japanese proximal femoral nail antirotation were taken in five limb postures: neutral, flexion, minute internal rotation, greater external rotation, and flexion with external rotation. Orthopedic surgeons performed five measurements of the sliding distance of the HFD in each of the flowing four methods: nail axis reference (NAR), modified NAR, inner edge reference, and nail tip reference. We also assessed two clinical cases by using these methods and evaluated the intraclass correlation coefficients.
Results
The measured values were consistent in the NAR method regardless of limb posture, with an even smaller error when using the modified NAR method. The standard deviation (SD) was high in the nail tip reference method and extremely low in the modified NAR method. In the two clinical cases, the SD was the lowest in the modified NAR method, similar to the results using plastic simulated bone. The intraclass correlation coefficients showed the highest value in the modified NAR method.
The incidence of proximal femur fractures is increasing proportionally with the aging of the population, since it is a lesion typically found in the elderly.1,2) Since stable fixation between the femoral head and shaft is essential, a short intramedullary nail is preferred, owing to its biomechanical advantage; the nail is nearer to the weight-bearing axis through the femoral head, compared with a sliding hip screw.3,4) Intramedullary nailing has other technical advantages, including lesser invasion, shorter skin incision, and less blood loss.1,3,4) These advantages allow earlier mobilization, including immediate full weight-bearing and rehabilitation.1) Although intramedullary nailing has become popular for these reasons, some complications have been reported. Among them, the most common serious complication is the so-called cut-out of the lag screw through the femoral head.5,6,7,8)
To reduce the risk of cut-out, various types of implants, such as hip screws and blades for trochanteric fractures, have been developed for fixating the femoral head.8,9,10,11) In this report, we use the term "femoral head fixation device" (HFD) as a general term for these implants. It has been recognized that cut-out of the HFD generally occurs due to poor HFD positioning.12,13,14) We also believe that its occurrence may depend on fracture type; in a complicated fracture with insufficient contact between the bones, excessive sliding of the HFD can occur due to lack of bony support, leading to femoral head rotation and subsequent cut-out. Other researchers have also reported that when sliding is excessive, the intended impaction on the fracture site may not be properly achieved, resulting in unsatisfactory outcomes.15,16,17)
For the above reasons, it is essential to measure the sliding distance precisely to evaluate excessive sliding. In our busy clinical practice, it is most convenient to measure sliding distance reliably using radiography. However, the correct measurement is not necessarily easy due to the difficulty of taking radiographs with the same limb posture postoperatively. Because sliding distance is defined as the change in relative positional relationships of both the intramedullary nail and HFD, ideally, we should be able to set a reference point on the nail and measure its precise location on the HFD.
Therefore, based on these reasons, we have developed the nail axis reference (NAR) method at our hospital, which we have used since 2002. However, it seemed to be somewhat difficult to set the axis of the nail. For a more convenient and accurate measurement, we have improved this method with the modified NAR method.
Although these methods are expected to be accurate and reproducible, no studies have examined which method is optimal. Therefore, the purpose of this study is to prospectively compare the accuracy and reproducibility of the NAR and modified NAR methods with other our original methods for the measurement of the sliding distance of the HFD.
We used plastic simulated bone implanted with a Japanese proximal femoral nail antirotation (J-PFNA) implant (Synthes, Oberdorf, Switzerland) (Fig. 1). The basic concept of the J-PFNA is the same as the PFNA, but is modified for Japanese patients who tend to have a smaller physique. Radiographs were taken in five postures: neutral, flexion, minute internal rotation, greater external rotation, and flexion with external rotation (Fig. 2). These radiographs were printed onto paper and five orthopedic surgeons performed five measurements in each of the four methods described below. In each method, we identified the tip of the HFD as "A," the base of the HFD as "B," and the central axis of the HFD as "AB," and examined the relative value with respect to the position of the reference point on AB (Fig. 3).
(1) NAR: We defined the intersection of the proximal nail axis and AB as reference point "C." Then, the percentage of AC/AB was calculated (Fig. 4A).
(2) Modified NAR: We defined the intersection of the inner edge of the nail and the lower edge of the HFD as "P," the intersection of the outer edge of the nail and the upper edge of the HFD as "Q," and the intersection of PQ and AB as reference point "C'." Then, the percentage of AC'/AB was calculated. Unlike the central method, the axis of the nail does not have to be drawn. We believe "C'" should theoretically match "C" (Fig. 4B).
(3) Inner edge reference: We defined the intersection of the inner edge of the nail and AB as reference point "D." Then, the percentage of AD/AB was calculated (Fig. 4C).
(4) Nail tip reference: We defined the intersection of the proximal edge of the nail and AB as "E." Then, the percentage of AE/AB was calculated. If point "E" exists on AB, the tip of the HFD is more proximal than the upper edge of the nail (Fig. 4D).
When calculated using plastic simulated bone, AC (AC') / AB = 75% in the NAR and modified NAR methods, AD / AB = 63% in the inner edge reference method, and AE / AB = -12% in the nail tip reference method. We compared these values with the radiographic measurements in each posture and examined the accuracy.
We also assessed two clinical cases using these methods: one case without excessive sliding (case 1) and another case with excessive sliding, femoral head rotation, and cut-out (case 2). In both cases, we examined three radiographs taken immediately postoperatively and at different periods after surgery.
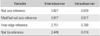
Intraclass correlation coefficients (ICCs) are known to be helpful for assessing the interobserver and intraobserver reliability of measurements by multiple observers.18) Their calculated values are classified by the following: slight agreement (0 to 0.20), fair agreement (0.21 to 0.40), moderate agreement (0.41 to 0.60), substantial agreement (0.61 to 0.80), and almost perfect agreement (0.81 to 1.00). In this study, we also evaluated the ICCs in the clinical case.
Results were analyzed using SPSS ver. 19J (IBM Japan, Tokyo, Japan). The Institutional Review Board of our institution approved the study.
Results using plastic simulated bone are shown in Table 1. Measured values using the inner edge reference and nail tip reference methods were significantly different depending on the limb posture on radiography. On the other hand, measured values were consistent in the NAR method regardless of limb posture, with an even smaller error when using the modified NAR method. Standard deviation (SD), used as an index of reproducibility, was high in the nail tip reference method and extremely low in the modified NAR method (1.4%). Results of the two clinical cases are shown in Table 2. The SD was also high in the nail tip reference method and low in the modified NAR method, similar to the results using plastic simulated bone. The result of the ICCs in the clinical cases are shown in Table 3. The modified NAR method showed the highest ICC value.
To reduce the risks of femoral head rotation and cut-out, and for early detection, it is essential to assess the sliding distance of the HFD on radiography from the early postoperative period. However, it is sometimes difficult to take radiographs with the same limb posture. Previously, Watanabe et al.19) reported a method for calculating sliding distance, described as total sliding (TS), of the Gamma Asia-Pacific nail (Howmedica, Rutherford, NJ, USA) and intramedullary hip screw (Smith & Nephew Richards, Memphis, TN, USA) using the following formulas: TS (L1 to L2) / cos 50° for a 130° nail or (L1 to L2) / cos 45° for a 135° nail, where L is the distance between the top of the nail and the tip of the lag screw. Their method resembles our nail tip reference method in terms of the relative relationships of the proximal edge of the nail and the tip of the HFD, but it seems to be too complicated to be practical in our busy clinical practice. Additionally, the ICC of nail tip reference method was the lowest value in our study (Table 3). Doppelt20) reported another method for evaluating radiographic changes, including femoral rotation, but was used for a sliding compression screw with a barrel.
In this way, few studies have investigated methods for measurement of sliding distance of the HFD in detail. In this study, we suggested four different methods. Based on our results, these methods would be very useful because certain measurements can be obtained even in different postures. On the other hand, in the inner edge reference method, if the cross section of the nail is not a perfect circle on the axial view, the length of AD will easily change in different limb postures. In the nail tip reference method, it is difficult to draw a line parallel from the nail tip through the center axis of the cross-section of the nail. Consequently, the length of AE will easily change depending on limb posture. In this study, we demonstrated that the NAR and modified NAR methods had better accuracy and reproducibility than other methods according to their ICCs. However, it can be somewhat difficult to set the axis of the nail in the NAR method; thus, the modified NAR method is recommended more strongly for measuring the sliding distance of the HFD based on its accuracy, reproducibility, and usefulness.
In this study, we examined the relative value (%) of the position of the intersection of the reference line for the entire length of the HFD. However, the absolute length of AC (AC') can be calculated from the actual length of the HFD used in surgery. The absolute value of the sliding distance also can be evaluated by comparing these lengths. The tip length of the HFD (TLH) was defined as AC/AB × real HFD length. Then, the sliding distance was calculated by subtracting TLH at follow-up from the immediate postoperative TLH. This method is easy and reliable, and very versatile regardless of screw or blade type. However, if the X-ray does not enter at a right angle to the long axis of the HFD, and oblique images are obtained, it is necessary to put A and B in its center, while considering the cross-section of the cylindrical (or rectangular) tip and base of the HFD. If we keep this in mind, it should be noted that some individual differences could be reduced and did not affect the overall accuracy based on this study. In summary, modified-NAR is one method for the precise estimation of the sliding distance after an operation of PFNA.
This study has certain limitations, including the small population, and the fracture type, which limited the levels of evidence. Another important limitation is that we analyzed the data using only one implant design and therefore cannot generalize these findings to all femoral HFD for trochanteric fractures. The comparison with other reported measurement methods of postoperative sliding distance will be more ideal. Therefore, multi-center and larger population clinical studies of unstable fracture types with several measurement methods seem to be required to further elucidate these types of problems in future.
We compared methods for measuring the sliding distance of the HFD in trochanteric fracture, the NAR and modified NAR, with other methods. We conclude that the modified NAR method should be most recommended, based on its accuracy, reproducibility, and usefulness.
Figures and Tables
Fig. 2
Radiographs showing five postures of intramedullary nailing: (A) neutral, (B) flexion, (C) minute internal rotation, (D) greater external rotation, and (E) flexion with external rotation.

Fig. 3
Methods for measurement of sliding distance. A: tip of head fixation device (HFD), B: base of HFD, C: intersection of proximal nail axis and AB, D: intersection of inner edge of nail and AB, E: intersection of proximal edge of nail and AB, P: intersection of inner edge of nail and lower edge of HFD, Q: intersection of outer edge of nail and upper edge of HFD, C': intersection of PQ and AB.
Fig. 4
Methods for measurement of sliding distance in detail. (A) Measurement of sliding distance by nail axis reference. Tip length of head fixation device (TLH) was defined as AC / AB × real head fixation device (HFD) length. (B) Measurement of sliding distance by modified nail axis reference. TLH was defined as AC' / AB × real HFD length. (C) Measurement of sliding distance by inner edge reference. TLH was defined as AD / AB × real HFD length. (D) Measurement of sliding distance by nail tip reference. TLH was defined as AE / AB × real HFD length.

Table 1
Comparison of the Results of Four Methods for Measurement of Sliding Distance Using Plastic Simulated Bone
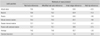
Table 2
Comparison of the Results of Four Methods for Measurement of Sliding Distance in Two Clinical Cases

ACKNOWLEDGEMENTS
The authors would like to thank Editage (www.editage.jp) for the English language review. And we also would like to thank the Japanese Society for Fracture Repair (JSFR) for the permission to publish our manuscript in CiOS. This manuscript is the revised edition of the journal Kossetsu (2011;33:652-654) in Japanese.
References
1. Fritz T, Weiss C, Krieglstein C, Quentmeier A. The classic nail in the therapy of trochanteric fractures: a prospective, controlled study. Arch Orthop Trauma Surg. 1999; 119(5-6):308–314.
2. Kannus P, Parkkari J, Sievanen H, Heinonen A, Vuori I, Jarvinen M. Epidemiology of hip fractures. Bone. 1996; 18:1 Suppl. 57S–63S.
3. Radford PJ, Needoff M, Webb JK. A prospective randomised comparison of the dynamic hip screw and the gamma locking nail. J Bone Joint Surg Br. 1993; 75(5):789–793.
4. Curtis MJ, Jinnah RH, Wilson V, Cunningham BW. Proximal femoral fractures: a biomechanical study to compare intramedullary and extramedullary fixation. Injury. 1994; 25(2):99–104.
5. Saudan M, Lubbeke A, Sadowski C, Riand N, Stern R, Hoffmeyer P. Pertrochanteric fractures: is there an advantage to an intramedullary nail?: a randomized, prospective study of 206 patients comparing the dynamic hip screw and proximal femoral nail. J Orthop Trauma. 2002; 16(6):386–393.
6. Sommers MB, Roth C, Hall H, et al. A laboratory model to evaluate cutout resistance of implants for pertrochanteric fracture fixation. J Orthop Trauma. 2004; 18(6):361–368.
7. Yoshimine F, Latta LL, Milne EL. Sliding characteristics of compression hip screws in the intertrochanteric fracture: a clinical study. J Orthop Trauma. 1993; 7(4):348–353.
8. Al-yassari G, Langstaff RJ, Jones JW, Al-Lami M. The AO/ASIF proximal femoral nail (PFN) for the treatment of unstable trochanteric femoral fracture. Injury. 2002; 33(5):395–399.
9. Halder SC. The Gamma nail for peritrochanteric fractures. J Bone Joint Surg Br. 1992; 74(3):340–344.
10. Zhou F, Zhang ZS, Yang H, et al. Less invasive stabilization system (LISS) versus proximal femoral nail anti-rotation (PFNA) in treating proximal femoral fractures: a prospective randomized study. J Orthop Trauma. 2012; 26(3):155–162.
11. Gehr J, Arnold T, Hilsenbeck F, Friedl W. The gliding nail, a universal implant in the treatment of proximal femur fractures. Eur J Trauma. 2006; 32(6):562–569.
12. Baumgaertner MR, Solberg BD. Awareness of tip-apex distance reduces failure of fixation of trochanteric fractures of the hip. J Bone Joint Surg Br. 1997; 79(6):969–971.
13. Park SY, Park J, Rhee DJ, Yoon HK, Yang KH. Anterior or posterior obliquity of the lag screw in the lateral view: does it affect the sliding characteristics on unstable trochanteric fractures? Injury. 2007; 38(7):785–791.
14. Johnson LJ, Cope MR, Shahrokhi S, Tamblyn P. Measuring tip-apex distance using a picture archiving and communication system (PACS). Injury. 2008; 39(7):786–790.
15. Tsukada S, Okumura G, Matsueda M. Postoperative stability on lateral radiographs in the surgical treatment of pertrochanteric hip fractures. Arch Orthop Trauma Surg. 2012; 132(6):839–846.
16. Buciuto R, Hammer R. RAB-plate versus sliding hip screw for unstable trochanteric hip fractures: stability of the fixation and modes of failure: radiographic analysis of 218 fractures. J Trauma. 2001; 50(3):545–550.
17. Parker MJ. Trochanteric hip fractures: fixation failure commoner with femoral medialization, a comparison of 101 cases. Acta Orthop Scand. 1996; 67(4):329–332.
18. Shrout PE, Fleiss JL. Intraclass correlations: uses in assessing rater reliability. Psychol Bull. 1979; 86(2):420–428.
19. Watanabe Y, Minami G, Takeshita H, Fujii T, Takai S, Hirasawa Y. Migration of the lag screw within the femoral head: a comparison of the intramedullary hip screw and the Gamma Asia-Pacific nail. J Orthop Trauma. 2002; 16(2):104–107.
20. Doppelt SH. The sliding compression screw: today's best answer for stabilization of intertrochanteric hip fractures. Orthop Clin North Am. 1980; 11(3):507–523.




 PDF
PDF ePub
ePub Citation
Citation Print
Print



 XML Download
XML Download