Abstract
Background
Locking of metacarpophalangeal joint (MPJ) of the index finger occurs when volar radial osteophytes of the metacarpal head catch the accessory collateral ligament. We devised a ligament-preserving approach to quickly restore the MPJ motion while protecting the radial collateral ligament.
Methods
We retrospectively reviewed the results of nine patients treated for a locked MPJ of the index finger. In three patients, closed reduction was successful. In six cases, volar radial osteophytes were excised from the metacarpal head using a ligament-preserving technique through a longitudinal incision on the radial side. We analyzed osteophyte shape and height as demonstrated by X-ray and computed tomography (CT). Function was evaluated by examining the range of motion, recurrence, Disabilities of the Arm, Shoulder and Hand (DASH) score, and MPJ stability based on the key pinch strength. One male and eight female patients were followed for an average of 33 months (range, 12 to 65 months); the average age of patients was 41 years (range, 34 to 47 years). The average duration of locking of the MPJ was 23 days (range, 1 to 53 days).
Results
The sharp type of osteophytes was identified in six patients and the blunt type of osteophytes was indentified in three patients. The average height of radial osteophytes on the index finger metacarpal was 4.6 ± 0.4 mm in the axial CT image. At the final follow-up, the average extension limitation decreased from 26° (range, 10° to 45°) to 0°, and further flexion increased from 83° (range, 80° to 90°) to 86°. There was no recurrent locking after surgery. The DASH score improved from 24.3 to 7.2. Key pinch strength improved from 67.3% to 90.4%.
A locked the metacarpophalangeal joint (MPJ) of the index finger occurs when the osseous prominence on the radial condyle of the metacarpal head catches the accessory collateral ligament (ACL).1,2) When manual reduction fails, operative treatment may be required.1,3) However, the ACL or collateral ligament (CL) may be injured if the conventional operative approach is used for resection of the osseous prominence. Stability of the MPJ in the index finger, which depends on the CL and the ACL, is especially important for the key pinch function.1,2,4,5) Thus, preservation of the CL can improve postoperative rehabilitation following open reduction for a locked MPJ of the index finger.
A method to excise radial condyle osteophytes for treating MPJ locking has been reported.1,2,6) We believe that the CL preserving approach is feasible and effective for removal of radial condyle osteophytes and allows rapid recovery of the MPJ motion without instability or recurrence. The purpose of this study is to analyze the outcomes after resection of osteophytes using an approach that does not interrupt the CL or the ACL in a locked MPJ of the index finger.
We retrospectively reviewed the results of nine patients who were treated for a locked MPJ of the index finger at our hospital between November 2004 and December 2011. The inclusion criteria for this study were: (1) passive extension limitation of greater than 20° without a history of trauma; (2) catching of the ACL on the osseous prominence of the radial condyle of the metacarpal head; and (3) follow-up of more than 12 months. The exclusion criteria were: (1) history of previous surgery or trauma; (2) locked MPJ in other fingers; and (3) flexion limitation of the MPJ.
One male and eight female patients were followed for an average of 33 months (range, 12 to 65 months) and their average age was 41 years (range, 34 to 47 years).
The average duration from the onset of joint locking to visit to our clinic was 23 days (range, 1 to 53 days). Two patients had several episodes of self-reduction. Four cases occurred in the right hand and 5 cases occurred in the left hand. The average extension limitation of the MPJ was 26° (range, 10° to 45°) and further flexion was 83° (range, 80° to 90°). Underlying diseases included chronic renal failure, lymphoma, and rheumatoid arthritis, each of which occurred in one case without any overlap.
The point of maximum tenderness was on the radial aspect of the MPJ. Initially, gentle manual reduction as described by Yagi et al.,3) which includes MPJ flexion, radial deviation, and external rotation of the proximal phalanx followed by gradual extension, was attempted. When this method failed, we resorted to open reduction.
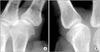
In three patients, closed reduction was successful. However, the remaining 6 patients required open reduction. A plain radiographic examination, including anteroposterior, oblique, and lateral X-rays, was performed in all of the patients to define the metacarpal head morphology based on the example by Yagi et al.3) (Fig. 1).
Four patients, in whom the metacarpal head had a sharp edge, were examined by computed tomography (CT). Osteophyte height, defined as the distance between the base of the condyle and the most prominent radial margin of the osteophyte, was measured on the metacarpal head and neck junction in the axial plane (Fig. 2). For evaluating the difference in the size of metacarpal bones between sexes and persons, we measured the diameter of the index finger metacarpal and the third metacarpal condyle radial osteophytes in the corresponding axial plane CT image. However, the difference in size was negligible.
In the six patients who underwent open reduction, function was evaluated by examining the range of motion, recurrences, Disabilities of the Arm, Shoulder and Hand (DASH) score, and MPJ stability using a key pinch gauge (B&L Engineering, Santa Fe Springs, CA, USA) (Fig. 3). If key pinch strength was more than 80% of that of the contralateral side, we considered that there was no instability of the MPJ. This study was approved by the Institutional Review Board of Soonchunhyang University Bucheon Hospital.
The operation was performed under general anesthesia. When the index MPJ was maximally flexed, a longitudinal ~2-cm incision was made on the radial aspect of the MPJ centered around the MPJ space. The radial part of the sagittal band was then split transversely along its fibers, and the MPJ capsule was opened along the dorsal border of the radial CL. Exposure of the metacarpal head confirmed that a volar radial osteophyte was impinging on the CL (Fig. 4). As the MPJ was flexed further, the proximal portion of the volar radial condyle osteophyte between the metacarpal head and neck junction became more accessible (Fig. 5). After removing the osteophyte using a mini-osteotome, we checked whether the MPJ could be extended fully. If locking was not resolved completely, we excised more bone from the radial edge of the condyle while preserving as much articular cartilage as possible. Extension of the MPJ was re-examined, and upon resolution of locking, the radial capsule and sagittal band were repaired sequentially.
All of the patients had tenderness on the volar radial side of the metacarpal head, which resolved spontaneously after the operation. At the final follow-up, the average extension limitation of the MPJ decreased from 26° to 0°, and further flexion increased from a mean 83° to 86°.
A plain radiograph showed that the osteophyte on the index metacarpal head had a sharp edge in six patients and a blunt edge in three patients. All six patients with sharp-edged metacarpal head osteophytes required open reduction, while all three locked fingers with blunt edged metacarpal head osteophytes were reduced manually. One patient with a blunt-edged metacarpal head osteophyte had bony erosion due to rheumatoid arthritis (Table 1).
The average height of the radial osteophytes on the index finger metacarpal was 4.6 ± 0.4 mm in the axial CT image, and the average ulnar osteophyte height was 2.3 ± 0.3 mm. In contrast, the average height of the radial osteophytes on the third metacarpal was 2.3 ± 0.1 mm, approximately half the height of the radial osteophytes in the affected joint. The average index finger metacarpal diameter at the level of osteophytes was 11.5 ± 0.8 mm. In six patients who underwent osteophyte excision, postoperative oblique radiographs confirmed complete removal of the metacarpal head osteophytes (Fig. 4).
Following surgery, the DASH score decreased from 24.3 to 7.2 points and key pinch strength improved from 67.3% to 90.4% of that of the contralateral side. There were no complications such as recurrent locking and no MPJ instability after surgery.
Among our cohort of nine patients who underwent treatment for locked MPJ of the index finger, six patients required open reduction, for which we used a novel ligament-preserving approach. We obtained satisfactory results without recurrence or instability, allowing for rapid recovery of the MPJ motion.
We identified the radiological morphology of the metacarpal head that underlies failure of manual reduction. Operative treatment for the locked MPJ was required in all of the patients with sharp metacarpal osteophytes. Moreover in these patients, CT confirmed that the height of osteophytes on the index radial metacarpal head was twice that of osteophytes on the third metacarpal head.
MPJ locking usually occurs in the index finger.1,2) Although the reason for this preponderance is not clear, it is though that thumb-index finger pinching, which transmits repeated load to the index radial metacarpal head, may play a contributory role.
Many authors have suggested that the radial ACL is involved in locking caused by osseous prominences of the radial metacarpal.1,2) The radial ACL originates from the metacarpal fovea and inserts obliquely into the volar plate. When the MPJ is flexed maximally, the ACL is relaxed and clears the proximal surface of the condyle. As the MPJ starts to extend, tension of the ACL over the osseous prominence of the volar metacarpal head increases, and the dorsal border of the ACL gets caught at the volar radial condyle edge, limiting MPJ extension.
The principle of reduction is to make space adjacent to the metacarpal head by radial deviation and external rotation of the proximal phalanx to alleviate ligament tension.3,7,8) However, reduction is not always successful and locking recurs occasionally.1) If an additional force, such as contraction of the lumbrical muscle, which passes through the radial side of the MPJ, is applied during reduction, it may interfere with resolution by reducing the space between the ACL and metacarpal head. Compression of the radial aspect of the MPJ caused by tight lumbrical muscle is especially likely if the proximal phalangeal joint is flexed.
Surgeons should not apply excessive force during reduction maneuvers.3) Careless reduction maneuvers can cause fractures of the metacarpal condyle, especially under anesthesia because the surgeon cannot accurately perceive the resistance within the joint. Although the possibility of fractures depends on bone quality and careful technique, condylar fractures may eventually result in MPJ contracture. In this study, fracture did not occur during manipulation.
In the study by Yagi et al.3) on 12 patients, the condyle tip appeared to be blunt in nine patients and sharp in three patients on X-ray. Radiographic examination did not show any association between manual reduction failure and either the sharp or blunt type. In our study, we observed a definite tendency for manual reduction failure in patients with sharp condyle tips, although statistical analysis was not possible due to the small number of patients. Moreover, our cohort included a larger proportion of patients with sharp condyles than in the report by Yagi et al.3) This difference in the proportion of patients with sharp condyles explains why many of our patients required open reduction compared to those in the series by Yagi et al.3)
There were some limitations to this study. First, the study included a small number of patients and it had a retrospective design, because locked MPJ is not very common. Second, we excluded cases of locking due to causes other than radial metacarpal head osteophytes.9,10) The limited incisions made in our surgical approach might make it difficult to identify other causes of MPJ locking. However, we did not find any causes other than volar radial osteophytes on the metacarpal head. Third, our study did not include any comparison group.
Our surgical approach to resolve MPJ locking of the index finger avoid injury to the CL and the ACL. We confirmed that this approach is feasible and effective for removal of osteophytes of the index radial metacarpal head and allows rapid recovery of MPJ motion without recurrence of locking.
Figures and Tables
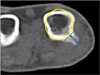 | Fig. 2Height of metacarpal head osteophytes of the index finger. The osteophyte height is defined as the distance between the base of the condyle and the most prominent radial margin of the osteophyte (arrow). Metacarpal diameter is measured from a circle template. Template of metacarpal head (yellow circle). |
 | Fig. 3A 46-year-old female patient (case 6) with a locked metacarpophalangeal joint (MPJ) of the index finger. (A) Oblique radiograph shows a sharp edge of the index metacarpal radial condyle. Axial (B) and three-dimensional (C) computed tomography images show radial osteophyte of the index metacarpal head. (D) Index MPJ extension was limited prior to surgery. |
 | Fig. 4A 34-year-old female patient (case 2) with a locked metacarpophalangeal joint (MPJ) of the index finger. (A) Intraoperative photograph during ligament-preserving surgery on the flexed index MPJ with a radial osteophyte on the metacarpal head. (B) Osteophyte fragment was removed from the radial metacarpal head using a mini-osteotome. (C) Postoperative photograph shows full extension of the MPJ. (D) Postoperative oblique radiograph does not show a visible sharp edge of the index metacarpal head. |
 | Fig. 5Diagram of our ligament-preserving surgical approach to remove condylar osteophytes. (A) When the metacarpophalangeal joint (MPJ) is flexed at 90°, the distal half of the radial osteophyte can be approached. (B) If the MPJ is hyperflexed beyond 90°, the more proximal portion of the radial osteophyte can be approached. |
Table 1
Details of the Nine Reviewed Patients

References
1. Inoue G, Miura T. Locked metacarpophalangeal joint of the finger. Orthop Rev. 1991; 20(2):149–153.
2. Thomsen L, Roulot E, Barbato B, Dumontier C. Locked metacarpophalangeal joint of long fingers: classification, definition and treatment based on 15 cases and literature review. Chir Main. 2011; 30(4):269–275.
3. Yagi M, Yamanaka K, Yoshida K, Sato N, Inoue A. Successful manual reduction of locked metacarpophalangeal joints in fingers. J Bone Joint Surg Am. 2000; 82(3):366–371.
4. Langenskiold A. Habitual locking of a meta-carpo-phalangeal joint by a collateral ligament, a rare cause of trigger finger. Acta Chir Scand. 1949; 99(1):73–78.
5. Lee S, Yum JK, Kim JY. Locking of the metacarpophalangeal joint of the thumb with the radial collateral ligament rupture after stress radiography. Arch Orthop Trauma Surg. 2010; 130(2):237–239.
6. Kim JK, Chung MS, Baek GH. Locked metacarpophalangeal joint of the index finger: consideration about the surgical approach. J Hand Surg Eur Vol. 2009; 34(2):278–280.
7. Guly HR, Azam MA. Locked finger treated by manipulation: a report of three cases. J Bone Joint Surg Br. 1982; 64(1):73–75.
8. Tajima K, Sato K, Sasaki T, Peimer CA. Vertical locking of the metacarpophalangeal joint in young adults. J Hand Surg Am. 2011; 36(9):1482–1485.
9. Aston JN. Locked middle finger. J Bone Joint Surg Br. 1960; 42-B:75–79.
10. Bloom MH, Bryan RS. Locked index finger caused by hyperflexion and entrapment of sesamoid bone. J Bone Joint Surg Am. 1965; 47(7):1383–1385.




 PDF
PDF ePub
ePub Citation
Citation Print
Print


 XML Download
XML Download