Abstract
Background
The treatment of simple bone cysts (SBC) in children varies significantly among physicians. This study examined which procedure is better for the treatment of SBC, using a decision analysis based on current published evidence.
Methods
A decision tree focused on five treatment modalities of SBC (observation, steroid injection, autologous bone marrow injection, decompression, and curettage with bone graft) were created. Each treatment modality was further branched, according to the presence and severity of complications. The probabilities of all cases were obtained by literature review. A roll back tool was utilized to determine the most preferred treatment modality. One-way sensitivity analysis was performed to determine the threshold value of the treatment modalities. Two-way sensitivity analysis was utilized to examine the joint impact of changes in probabilities of two parameters.
Results
The decision model favored autologous bone marrow injection. The expected value of autologous bone marrow injection was 0.9445, while those of observation, steroid injection, decompression, and curettage and bone graft were 0.9318, 0.9400, 0.9395, and 0.9342, respectively. One-way sensitivity analysis showed that autologous bone marrow injection was better than that of decompression for the expected value when the rate of pathologic fracture, or positive symptoms of SBC after autologous bone marrow injection, was lower than 20.4%.
Conclusions
In our study, autologous bone marrow injection was found to be the best choice of treatment of SBC. However, the results were sensitive to the rate of pathologic fracture after treatment of SBC. Physicians should consider the possibility of pathologic fracture when they determine a treatment method for SBC.
Simple bone cysts (SBC) or unicameral bone cysts are benign bone tumors in children and adolescents. They nearly always occur during the first two decades of life, and are located in the metaphysis of the long bones, predominantly in the proximal humerus and femur. In general, patients with SBC visit physicians because of pain. However, SBC can be asymptomatic and is diagnosed incidentally when patients take radiographs for other reasons.
The treatment of SBC in children varies significantly among physicians and institutions. Although SBC may resolve spontaneously as patients approach skeletal maturity,1) surgical intervention is often needed because SBC may lead to pathologic fractures. The widely used treatment modalities of SBC are observation, steroid injection, autologous bone marrow injection, decompression, and curettage with bone graft. Previous studies have reported variable outcomes in the literature. There is no consensus for how to treat SBC; therefore, physicians may be confused to choice from a wide variety of treatment modalities.
A randomized controlled trial (RCT), which eliminates selection bias, can help physicians to provide effective treatment objectively. However, RCT needs an excessive long-term follow-up period and is associated with high cost in some fields of orthopedic research. Alternatively, decision analysis using observational studies is a logical process for identification of the best option in the face of uncertainty.2) The decision analysis, which was originally used in the business field, has made it possible to obtain evidence-based knowledge without performing an RCT, and is a useful tool for formulating and generalizing the decision-making process.3) For example, Event A has a benefit of 0.7 with a probability of 0.6 and a loss of -0.3 with a probability of 0.4, and Event B has a benefit of 0.8 with a probability of 0.7 and a loss of -0.3 with a probability of 0.3. The final expected value of Event A is (0.7 × 0.6) - (0.3 × 0.4) for a final value of 0.3, and that of Event B is (0.8 × 0.7) - (0.3 × 0.3) for a final value of 0.47. In this case, the model favors Event B.
The purpose of this study was to examine which procedure is better for the treatment of SBC in children, using a decision analysis based on the current published evidence.
The present study was exempt from Institutional Review Board because it did not involve human subjects as its resources.
In this study, a decision analysis model focused on five treatment modalities of SBC: observation, steroid injection, autologous bone marrow injection, decompression, and curettage with bone graft. We conducted a Pubmed search using a Boolean operator (OR) to combine keywords (simple bone cyst [tiab] OR unicameral bone cyst [tiab]) from the abstracts. In addition, studies were identified by a manual search of the reference lists of reviews and retrieved studies. The present study included literature that (1) provided the treatment, which was noted above; (2) had identifiable cases without pathologic fracture before the treatment; and (3) had results regarding the first outcome of a series of procedures. Decompression included multiple drilling, intramedullary nailing, and screw insertion. In curettage with bone graft, the type of grafted bone included both autobone and allobone. Cases with pathologic fracture before treatment or with unconfirmed information were excluded. The methodological quality of the included studies was evaluated using the Strengthening the Reporting of Observational Studies in Epidemiology (STROBE) statement.4) The STROBE statement is a checklist of 22 items that we consider essential for good reporting of observational studies.
The search on the PubMed database and the manual search identified a total of 320 published articles. There was one study regarding observation, 13 for steroid injection, 15 for autologous bone marrow injection, 12 for decompression, and 18 for curettage and bone graft as treatment options of SBC. After implementation of inclusion and exclusion criteria, 10 studies were finally included in our decision analysis and the STROBE Statement of the studies ranged from 12 to 20 (Table 1).5-14)
TreeAge Pro 2012 (TreeAge Software Inc., Williamstown, MA, USA) was utilized to construct a decision tree (Fig. 1). The root node (quadrangle) of SBC was branched into five treatment modalities, as noted above. Chance nodes (round) followed each treatment modality. Clinical outcomes of each treatment modality were categorized into three groups: (1) healed, (2) no change or progression or recurrence, and (3) pathologic fracture or positive symptoms. Each treatment modality was branched according to the presence of complications of general anesthesia and the surgical procedure, and all of branches reached the 3 clinical outcomes. The terminal node (triangle) at an endpoint is "utility," which means a clinical outcome in the decision tree. Each utility was estimated by the first procedure of each surgical intervention. Within an expected utility analysis, the value of any treatment modality is the weighted average of the outcomes, which may result from choosing that option; that is, the expected value is the sum of the utility values of each possible outcome, multiplied by the likelihood that the given outcome will be achieved.2)
As follow-up without an intervention, SBC could be healed. Previous studies showed that 9.1% of the observed were 'healed.'5) The remainder of the observed SBC were divided into 2 branches: 'no change or progression or recurrence,' and 'pathologic fracture or positive symptoms.' We divided the results of SBC treatment of into three clinical outcomes, as mentioned above, because each of the clinical outcomes needed a different treatment plan. 'Healed' meant there was no necessity for further treatment. However, a patient with 'pathologic fracture or positive symptoms' needed the intervention repeated or a more extensive procedure. A patient with 'no change or progression or recurrence' might be treated with observation, a repetition of the intervention, or other procedure depending on the physician's decision.
We assumed a baseline rate for pathologic fracture or positive symptoms of the observed SBC to be 45.5%. And the baseline rate for no change or progression or recurrence of the observed SBC would be 45.4% (Fig. 1).
The surgical intervention branches of SBC were comprised of 4 procedures: seroid injection, autologous bone marrow injection, decompression, and curettage with bone graft. Each of the interventions need general anesthesia, and may cause surgical wound infection. First, each of the surgical interventions branched into 2 branches, 'complications' and 'no complications.' Complications branched into 'minor complications' and 'major complications.' The minor complications category was comprised of surgical wound infection and anesthesia-related minor complications, such as sore throat, nausea, vomiting, and thrombophlebitis. Again, the minor complications group was divided into 'surgical wound infection' and others. In steroid injection and autologous bone marrow injection, the chance nodes of surgical wound infection and no surgical wound infection were divided into 2 branches, the presence of complications caused by the injected material or no complications. The major complication was death caused by anesthesia-related complications. Each end of the branches was categorized into 3 clinical outcomes: 'healed,' 'no change or progression or recurrence,' and 'pathologic fracture or positive symptoms.' A previous study showed that mortality in anesthesia ranges from 0 to 0.033% (Table 2).15-23) The baseline mortality of the surgical intervention was 0.0165%. A literature review revealed that the minor complications rate related to anesthesia ranges from 19% to 68%16-18) and the surgical wound infection rate ranges from 0.7% to 11.6%.19-23) Therefore, we assumed that the rate of complications for decompression and curettage with bone graft ranged from 19 to 80.1%. The baseline complication rate for them was 50%. A previous study showed that the incidence of complications with locally injected steroids was approximately 1%.24) Complications with locally injected autologous bone marrow have been reported only occasionally. However, there was a lack of studies regarding the incidence of autologous bone marrow injection related complications. We assumed that the rate of complications, with locally injected autologous bone marrow, was 1%. Therefore, the overall rate of complications by steroid injection and autologous bone marrow injection ranged from 19% to 81.1% and the baseline complication rate for them was 50.5%. Because of the absence of skin incisions, the rate of wound infection from steroid injection and autologous bone marrow injection was believed to be lower than that for decompression and curettage with bone graft. It was assumed that the baseline wound infection rate, after steroid injection and autologous bone marrow injection, would be 1% and that for decompression and curettage with bone graft would be 3%. Three categorized clinical outcomes, after surgical interventions, were positioned at the ends of the branches (Table 3).5-14)
Final clinical outcomes were assessed, using 'utility' as a percentage (Table 4). Five orthopedic surgeons with 28, 12, 10, 8, and 7 years of orthopedic experience, respectively, held consensus building sessions for utility assessment. The utility, the final clinical outcome score for each treatment modality which takes into account the severity of complications, was defined with a factor of 100% representing perfect health, and a factor of 0 representing death. In cases of needing general anesthesia or skin incisions, we assumed that utility was decreased by 1% and 3%, respectively. Minor complications of surgical intervention were assumed to cause a 3% decrease in the utility score, and surgical wound infections to cause an additional 5% decrease. Complications caused by the injected materials, steroids and autologous bone marrow, were assumed to cause a 1% decrease in the utility score. In cases of no change or progression or recurrence, we assumed that utility was decreased by 5%. If there were pathologic fractures or positive symptoms, utility was decreased by 10%.
The uncertainty and stability of the decision tree model were assessed, using a sensitivity analysis tool. The sensitivity analysis, which provides the threshold probabilities for each event, compensates the uncertainty of the decision tree model. One-way sensitivity analysis was used to assess the impact of alterations in the probability of one parameter on the conclusion. The overall rates of pathologic fracture or positive symptoms for steroid injection and autologous bone marrow injection ranged from 0% to 19.2%6,11,12) and from 0% to 21.0%,7,8,11,12,14) respectively. The rate of pathologic fracture or positive symptoms for decompression and curettage with bone graft was 0%.6,9-14) However, the entire possible range of each event, which was between 0% and 100%, was included. One-way sensitivity analysis was performed to determine the threshold value of the treatment modalities. The threshold value is the point at which intersection occurs with each variable. Two-way sensitivity analysis was also utilized to examine the joint impact of changes in the probabilities of two parameters.
The results of the decision model showed that autologous bone marrow injection was the most preferred treatment modality among the five. The expected value for autologous bone marrow injection was 0.9456 while those for observation, steroid injection, decompression, and curettage and bone graft were 0.9318, 0.9411, 0.9406, and 0.9352, respectively.
One-way sensitivity analysis showed that autologous bone marrow injection was better than decompression for the expected value when the rate of pathologic fracture or positive symptoms of SBC after autologous bone marrow injection was lower than 20.4% (Fig. 2). Whereas, steroid injection was better than decompression, when the rate of pathologic fracture or positive symptoms of SBC after steroid injection was lower than 10.5% (Fig. 3).
Two-way sensitivity analysis examined the proportion of the rates of pathologic fracture or positive symptoms of autologous bone marrow injection and decompression. The results suggested that autologous bone marrow injection was better than decompression by the expected value (Fig. 4).
We evaluated 5 treatment modalities, which were the most widely used treatments of SBC. According to the decision analysis, based on current evidence, autologous bone marrow injection is the best choice of treatment of SBC in terms of utility score, and observation was the least preferred treatment modality among the five.
Before discussing the results of the study, some limitations need to be addressed. First, most of the baseline values in this study were derived from previous studies. The quality of some of the studies might be weak. The credibility of the decision analysis model depends on the valid estimates of the probabilities of the events included in the model.3) Therefore, to increase credibility, we utilized a sensitivity test. Second, the anatomical location of SBC was not considered because there was a lack of studies that reported the clinical outcomes of SBC treatment associated with the location of the lesion. Treatment options can be changed depending on the location of SBC; because SBC, located on a weight bearing area, can be vulnerable to the pathologic fracture. Therefore, sensitivity analysis on the rate of pathologic fracture or positive symptoms after the treatment of SBC was performed to provide threshold probabilities of the rate for each event. The threshold probabilities help physicians determine the best treatment of SBC, according to the location of the lesion. Third, studies that we had reviewed had a different treatment algorithm in similar cases. For example, if there had been no response after steroid injection, subsequent treatments varied with the study: observation, repeat steroid injection, or curettage with bone graft, etc. Therefore, we designed a tree model with only the first outcome of a series of the procedures. Fourth, all procedures needing anesthesia were assumed to use general anesthesia. However, there might be cases that used a regional or local anesthesia. There were no studies that mentioned the method of anesthesia during the procedure. Fifth, to eliminate unexpected factors affecting the prognosis of SBC, cases of previous pathologic fracture before treatment were excluded. As a result, the validity of this study may increase, but a large amount of studies were excluded. In decision analysis, sensitivity analysis could supplement the uncertainty of the decision including a small number of studies.
Although several studies have compared the treatment modalities of SBC,12,25,26) they could not suggest treatment guidelines for SBC due to a lack of uniform clinical measurements. In this study, all of the clinical outcomes of the treatment modalities of SBC were assessed using utility scores. Furthermore, because preoperative pathologic fracture might affect the clinical outcomes of SBC treatment, we excluded cases of patients with preoperative pathologic fracture in previous studies. This study considered the possible complications caused by the procedures.
According to the decision analysis model, autologous bone marrow injection is the best choice of treatment of SBC in terms of utility score, followed by steroid injection. However, these injection procedures have systemic complications, even though they are thought to be rare. There was a report regarding the potential risk of fat embolus, following an autologous bone marrow injection for SBC. A fat embolism is able to cause transient bradycardia, decreased blood pressure, and a transient decrease in exhaled CO2 as systemic complications,27) and also death. A previous study showed that complete communication was discovered between the cyst and its venous drainage.28) Further research is needed to determine the systemic effects of locally injected autologous bone marrow and steroids.
In cases of curettage with bone graft, we did not consider the type of bone, autobone or allobone. A previous study showed that there was a significant rate of persistent pain and morbidity from iliac crest bone grafts.29) The usage of an autologous bone graft might decrease the utility score.
Bone marrow injection was the best choice of treatment for SBC in our decision model. However, the model is sensitive to the possibility of pathologic fracture after treatment, which might be related to the size and location of the lesion. Therefore, the risk of pathologic fracture should be considered when determining a treatment method.
The decision analysis model can be changed over time, as new evidence is presented. Updating the probability and utility with new evidence could make a more confident decision model.
Figures and Tables
Fig. 1
Simplified decision analysis tree with probability and utility variables. The decision node branches into 'observation,' 'steroid injection,' 'autologous bone marrow injection,' 'decompression,' and 'curettage with bone graft.' Sx: symptoms.

Fig. 2
One-way sensitivity analysis on the rate of pathologic fracture or positive symptoms of simple bone cysts after autologous bone marrow injection shows the threshold probability. The threshold probability preferring autologous bone marrow injection is 20.4% of the rate of pathologic fracture or positive symptoms of the steroid injection. At higher than this rate, the decision analysis model prefers decompression. The possible range of this rate is between 0% and 21.0% based on previous studies (grey zone).
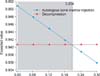
Fig. 3
One-way sensitivity analysis on the rate of pathologic fracture or positive symptoms of simple bone cysts after steroid injection shows the threshold probability. The threshold probability preferring steroid injection is 10.5% of the rate of pathologic fracture or positive symptoms of the steroid injection. At higher than this rate, the decision analysis model prefers decompression. The possible range of this rate is between 0% and 19.2% based on previous studies (grey zone).
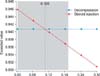
Fig. 4
Two-way sensitivity analysis on the rate of pathologic fracture or positive symptoms of simple bone cysts (SBC) after autologous bone marrow injection and steroid injection. This results show a preferred decision according to changes in the rate of pathologic fracture or positive symptoms of SBC after steroid injection and autologous bone marrow injection. Autologous bone marrow injection occupied a larger area than steroid injection. The results suggest that autologous bone marrow injection is better than steroid injection by the expected value.
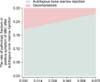
Table 1
Studies on the Results of the Treatment Modalities of Simple Bone Cyst

BG: bone graft, BM: bone marrow, STROBE: Strengthening the Reporting of Observational Studies in Epidemiology.
*Spontaneous healing was achieved in 5 cases. One patient had no fractures, whereas 4 patients had multiple fractures during observation. The study has no mention of cases in which spontaneous healing was not achieved.
References
1. Wilkins RM. Unicameral bone cysts. J Am Acad Orthop Surg. 2000; 8(4):217–224.
2. Bernstein J. Decision analysis. J Bone Joint Surg Am. 1997; 79(9):1404–1414.
3. Park MS, Chung CY, Kwon DG, Sung KH, Choi IH, Lee KM. Prophylactic femoral varization osteotomy for contralateral stable hips in non-ambulant individuals with cerebral palsy undergoing hip surgery: decision analysis. Dev Med Child Neurol. 2012; 54(3):231–239.
4. von Elm E, Altman DG, Egger M, et al. The Strengthening the Reporting of Observational Studies in Epidemiology (STROBE) statement: guidelines for reporting observational studies. Ann Intern Med. 2007; 147(8):573–577.
5. Kaelin AJ, MacEwen GD. Unicameral bone cysts: natural history and the risk of fracture. Int Orthop. 1989; 13(4):275–282.
6. Farber JM, Stanton RP. Treatment options in unicameral bone cysts. Orthopedics. 1990; 13(1):25–32.
7. Lokiec F, Ezra E, Khermosh O, Wientroub S. Simple bone cysts treated by percutaneous autologous marrow grafting: a preliminary report. J Bone Joint Surg Br. 1996; 78(6):934–937.
8. Docquier PL, Delloye C. Treatment of simple bone cysts with aspiration and a single bone marrow injection. J Pediatr Orthop. 2003; 23(6):766–773.
9. Abdel-Wanis ME, Tsuchiya H, Uehara K, Tomita K. Minimal curettage, multiple drilling, and continuous decompression through a cannulated screw for treatment of calcaneal simple bone cysts in children. J Pediatr Orthop. 2002; 22(4):540–543.
10. Roposch A, Saraph V, Linhart WE. Treatment of femoral neck and trochanteric simple bone cysts. Arch Orthop Trauma Surg. 2004; 124(7):437–442.
11. Kokavec M, Fristakova M, Polan P, Bialik GM. Surgical options for the treatment of simple bone cyst in children and adolescents. Isr Med Assoc J. 2010; 12(2):87–90.
12. Canavese F, Wright JG, Cole WG, Hopyan S. Unicameral bone cysts: comparison of percutaneous curettage, steroid, and autologous bone marrow injections. J Pediatr Orthop. 2011; 31(1):50–55.
13. Cha SM, Shin HD, Kim KC, Hwang JM, Kim BK. Outcomes from treatment of simple bone cyst in the long bones with flexible intramedullary nailing in children and adolescents: a retrospective cases series. J Korean Orthop Assoc. 2012; 47(3):178–184.
14. Baek SG, Oh CW, Jeon IH, Min WK, Park IH. Comparison of results by its location and treatment modality of the simple bone cyst. J Korean Musculoskelet Transplant Soc. 2006; 6(2):88–97.
15. Gonzalez LP, Pignaton W, Kusano PS, Modolo NS, Braz JR, Braz LG. Anesthesia-related mortality in pediatric patients: a systematic review. Clinics (Sao Paulo). 2012; 67(4):381–387.
16. Stadler M, Bardiau F, Seidel L, Albert A, Boogaerts JG. Difference in risk factors for postoperative nausea and vomiting. Anesthesiology. 2003; 98(1):46–52.
17. Hines R, Barash PG, Watrous G, O'Connor T. Complications occurring in the postanesthesia care unit: a survey. Anesth Analg. 1992; 74(4):503–509.
18. Apfel CC, Kranke P, Eberhart LH. Comparison of surgical site and patient's history with a simplified risk score for the prediction of postoperative nausea and vomiting. Anaesthesia. 2004; 59(11):1078–1082.
19. van Kasteren ME, Mannien J, Ott A, Kullberg BJ, de Boer AS, Gyssens IC. Antibiotic prophylaxis and the risk of surgical site infections following total hip arthroplasty: timely administration is the most important factor. Clin Infect Dis. 2007; 44(7):921–927.
20. Abu Hanifah Y. Post-operative surgical wound infection. Med J Malaysia. 1990; 45(4):293–297.
21. Dhillon KS, Kok CS. The incidence of post-operative wound infection in orthopaedic surgery. Med J Malaysia. 1995; 50(3):237–240.
22. Pittet D, Harbarth S, Ruef C, et al. Prevalence and risk factors for nosocomial infections in four university hospitals in Switzerland. Infect Control Hosp Epidemiol. 1999; 20(1):37–42.
23. National Nosocomial Infections Surveillance (NNIS) System report, data summary from October 1986-April 1998, issued June 1998. Am J Infect Control. 1998; 26(5):522–533.
24. Shrier I, Matheson GO, Kohl HW 3rd. Achilles tendonitis: are corticosteroid injections useful or harmful? Clin J Sport Med. 1996; 6(4):245–250.
25. Hagmann S, Eichhorn F, Moradi B, et al. Mid- and long-term clinical results of surgical therapy in unicameral bone cysts. BMC Musculoskelet Disord. 2011; 12:281.
26. Sung AD, Anderson ME, Zurakowski D, Hornicek FJ, Gebhardt MC. Unicameral bone cyst: a retrospective study of three surgical treatments. Clin Orthop Relat Res. 2008; 466(10):2519–2526.
27. Yandow SM, Marley LD, Fillman RR, Galloway KS. Precordial Doppler evaluation of simple bone cyst injection. J Pediatr Orthop. 2009; 29(2):196–200.
28. Abril JC, Queiruga JA, Casas J, Albinana J. Unusual finding after contrast injection of a solitary bone cyst: a case report. Acta Orthop Belg. 1999; 65(2):235–238.
29. Kim DH, Rhim R, Li L, et al. Prospective study of iliac crest bone graft harvest site pain and morbidity. Spine J. 2009; 9(11):886–892.




 PDF
PDF ePub
ePub Citation
Citation Print
Print





 XML Download
XML Download