Abstract
Background
Preventive measures need to be implemented to lower the incidence of osteoporotic fractures. Osteoporotic fractures increase morbidity and mortality as well as impose a socioeconomic burden; however, current research is limited to the administration rates of osteoporosis drugs for Korean postmenopausal females.
Methods
This study represents a nationwide, observational, and cross-sectional survey that investigates the administration rates of osteoporosis drugs based upon a bone mineral density (BMD) test performed on Korean postmenopausal patients who visited outpatient orthopedic clinics. BMD test results were examined in postmenopausal female patients (50 to 80 years of age); subsequently, the patients were classified into an osteoporosis group, osteopenia group, and normal group. The administration rates of osteoporosis drugs and bisphosphonates were then analyzed. The osteoporosis group was subdivided into a T-score less than -3.0 group and a T-score between -3.0 and -2.5 group that were separately analyzed.
Results
Based on the lumbar spine BMD, the rate of administration of osteoporosis drugs in the osteoporosis group was 42.1%, which was significantly higher compared to the osteopenia group or normal group. A significantly low bone mineral density was observed in patients who were administered bisphosphonates. Based on the lumbar spine BMD, the administration rate of osteoporosis drugs in the group with a T-score between -3.0 and -2.5 (34.2%) was significantly lower than the group with a T-score less that -3.0 (46.2%). The bisphosphonate administration rate was also significantly low; however, the administration rate for osteoporosis drugs was significantly lower than that of the osteopenia group.
Osteoporosis increases the fracture risk due to the reduction of bone strengh and bone mineral density (BMD) as well as the deterioration of the microarchitecture.1) Osteoporosis is asymptomatic unless fractures occur, and patients with osteoporosis do not realize the necessity of treatment or the adverse effects of neglecting treatment if the BMD is not regularly monitored. Fractures affect patient morbility and mortality; in addition, the socioeconomic costs of treatment increase significantly.2,3) The number of patients in Korea with osteoporosis has increased due to an aging population with a concomitant increase in the rate of osteoporotic fractures. Active prevention and treatment are required to treat osteoporosis.
The most commonly prescribed medications for osteoporosis in Korea are bone resorption inhibitors (oral bisphosphonate/intravenous bisphosphonate, selective estrogen receptor modulator [SERM], and calcitonin); in addition, parathyroid hormone (a bone formation accelerator) is also prescribed. Calcium and vitamin D are also recommended as supplements. In Korea, insurance coverage is provided for bisphosphonates, SERM, and calcitonin prescriptions based upon the results of a BMD test using dual energy X-ray absorptiometry (DXA). Subsequently, the insurance benefit allowance criteria may influence the prescription of medications for osteoporosis.
Osteoporosis is defined by the World Health Organization (WHO) as a T-score -2.5 or lower based on the results of the DXA. Osteopenia is defined as a T-score over -2.5 and less than -1.0, and a T-score that exceeds -1.0 is considered normal. However, until 2011, the National Health Insurance Service (NHIS) criteria for osteoporosis drugs in Korea covered only osteoporosis patients with a T-score less than -3.0; subsequently, NHIS insurance benefits for osteoporosis drugs were unavailable to patients whose T-score exceeded -3.0 and was less than -2.5. Patients can not purchase the osteoprosis drug without the prescription of a medical doctor. For patients with osteoporosis whose T-score exceeds -3.0 and is less than -2.5, doctors prescribe the osteoprosis drug that is covered by insurance.
The objectives of this study were: (1) to investigate the administration rate and methods of osteoporosis drugs via nationwide, observational, and cross-sectional surveys based on a T-score computed from the DXA in patients who visited outpatient orthopedic clinics; and (2) to evaluate the differences in the administration of osteoporosis drugs between osteoporosis patients with a T-score under -3.0 who qualified for the insurance benefit criteria in 2011 and the patients with a T-score over -3.0 and under -2.5 who did not meet the insurance benefit criteria.
In this study, nationwide, observational, and cross-sectional surveys were conducted on Korean postmenopausal patients who visited the orthopedics outpatient clinics of 62 Korean general hospitals and clinics in 2011. The number of subjects was calculated assuming a 26% prevalence of osteoporotic compression vertebral fractures and 5% precision. The target subjects were 1,183 with a 95% confidence interval; subsequently, a total of 1,281 subjects were included in this study as final test subjects. To correct for regional differences among regions, the regional distribution of females older than 50 years old was confirmed utilizing the data provided by the Korea National Statistical Office in 2005. It was divided into a total of 4 regions that include the Seoul Metropolitan, Central, Youngnam, and Honam areas, with the same proportion of patients recruited from each region. The hospital obtained prior approval from the Institutional Review Boards based upon the Declaration of Helsinki for this study; subsequently, written informed consent was obtained from all participants.
Female patients (50 to 80 years old) diagnosed as menopausal were selected from the patients who visited the orthopedics outpatient clinics. The subjects excluded from this study included (1) subjects without a diagnosis of menopause; (2) subjects who had high-energy injuries (including car accidents and falls) within the previous 3 months; (3) subjects who experienced nonvertebral fractures within the previous 6 months; (4) subjects lacking sufficient cognitive ability (based on the discretion of researchers); (5) cases where a normal readout was not possible in more than 2 segments due to fractures between the 1st and 4th lumbar spine vertebrae or instrumentation; and (6) cases where a BMD test could not be performed on both sides of the femur because of femoral fractures or instrumentation.
The DXA was used to measure the BMD of the lumbar spine, femoral neck, and total hip. If available, the data was replaced with the measurements from three months prior. Each patient was scanned under the examination guidelines from the manufacturer of the bone mineral densitometer. The lumbar spine (between the 1st and 4th vertebrae) was measured and cases with fractures or instrumentation present in that range were excluded; subsequently, the remaining measurements were averaged to calculate the lumbar spine averages. The data of the non-surgical side was applied if there was a surgical history in the femoral neck and total hip.
The administration rate of osteoporosis drugs was evaluated based on the normal group, osteopenia group, osteoporosis group (T-score ≥ -1.0, -2.5 < T-score < -1.0, and T-score ≤ -2.5), and combined group (T-score < -1.0). Then, the BMD of the patients (with and without bisphosphonate prescriptions) was compared regarding the lumbar spine, femoral neck, and total hip. The administration rates of osteoporosis drugs and bisphosphonates in the T-score ≤ -3.0 group and the -3.0 < T-score ≤ -2.5 group were evaluated after subdividing the current insurance benefit criteria for the osteoporosis group (T-score -3.0). The administration rates of osteoporosis drugs and bisphosphonates in the -3.0 < T-score ≤ -2.5 group and -2.5 < T-score < -1 group were investigated as well.
The statistical analysis of the administration rate of osteoporosis drugs among the groups utilized the Cochran-Armitage trend test. Student's t-test analyzed the BMD of patients with and without bisphosphonate administration. The chi-square test compared the administration rates of osteoporosis drugs and bisphosphonates between the T-score ≤ -3.0 group and the -3.0 < T-score ≤ 2.5 group as well as between the -3.0 < T-score ≤ -2.5 group and the -2.5 < T-score < -1 group.
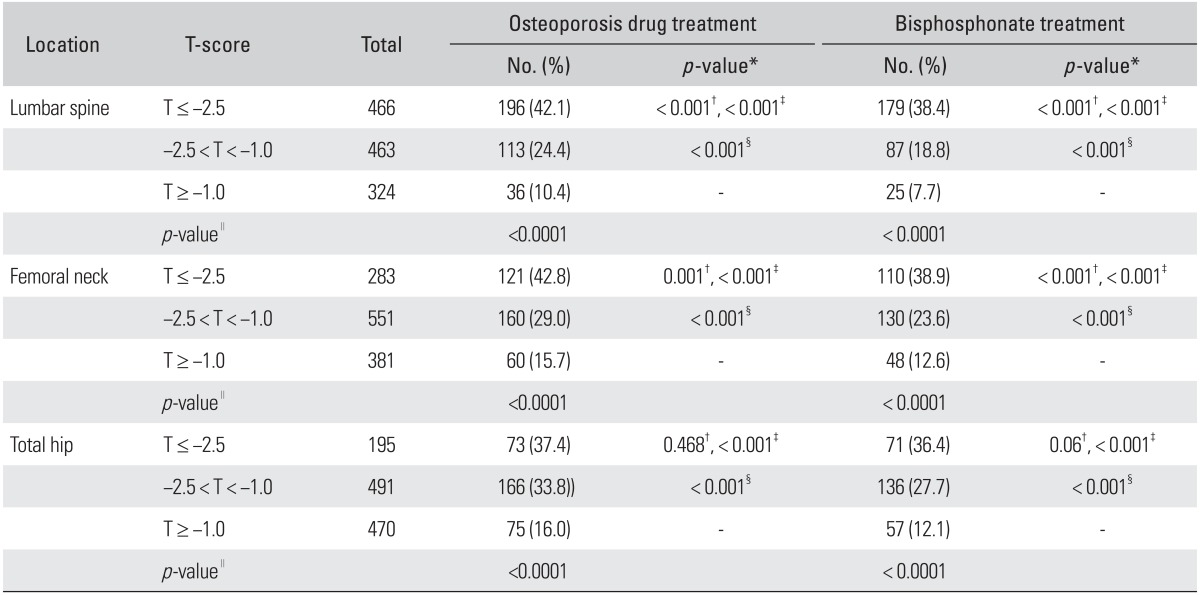
Of 1,225 patients, the number of patients who were administered bisphosphonates was 292 subjects (SERM dose, 11 subjects; calcitonin, 1 subject; and parathyroid hormone, 1 subject). Based on the lumbar spine T-score, the administration rate of osteoporosis drugs was 42.1% in the osteoporosis group, 24.4% in the osteopenia group, and 10.4% in the normal group. The administration rate for bisphosphonates was 38.4% in the osteoporosis group, 18.8% in the osteopenia group, and 7.7% in the normal group, showing significant differences among the groups (p < 0.0001). The administration rate of osteoporosis drugs as well as bisphosphonates was significantly higher in the osteoporosis group compared to the osteopenia group and normal group (p < 0.001). The prescription rate for osteoporosis drugs and bisphosphonates was significantly higher for the osteopenia group versus the normal group (p < 0.001) (Table 1). Based on the femoral neck T-score, the administration rate of osteoporosis drugs and bisphosphonates in the osteoporosis group was 42.8% and 38.9%, respectively. Based on the total hip T-score, the administration rate for osteoporosis drugs and bisphosphonates in the osteoporosis group was 37.4% and 36.4%, respectively. The administration rate for osteoporosis drugs (p < 0.001) and bisphosphonates (p < 0.001) in the osteoporosis group was significantly higher compared to the osteopenia group and normal group according to the T-scores for the femoral neck and total hip. The osteopenia group was administered osteoporosis drugs (p < 0.001) and bisphosphonates (p < 0.001) at a significantly higher rate than the normal group.
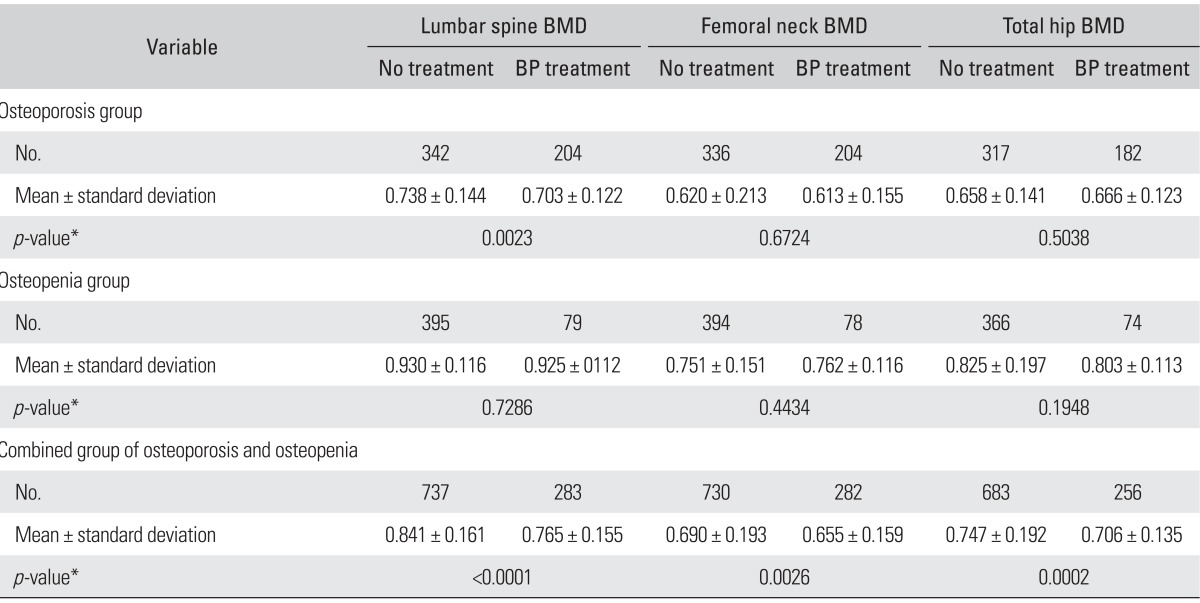
Based on the lumbar spine T-score, the osteoporosis patients who were administered bisphosphonates had a significantly lower BMD (0.703 g/cm2) than patients not administered bisphosphonates (0.738 g/cm2; p = 0.0023). The BMD of the femoral neck and total hip was lower in patients with bisphosphonate administration compared to patients without prescriptions; however, there was no statistically significant difference observed (Table 2). In the osteopenia group, statistically significant differences were not found in the BMD of the lumbar spine, femoral neck, and total hip between the patients with and without bisphosphonate administration. In the analysis that combined the osteoporosis group and osteopenia group, the BMD of the lumbar spine was 0.765 g/cm2, that of the femoral neck 0.655 g/cm2, and that of the total hip 0.706 g/cm2 in patients with bisphosphonate administration. These were significantly lower than the BMD in patients without bisphosphonate administration, who had a lumbar spine BMD of 0.841 g/cm2, femoral neck BMD of 0.690 g/cm2, and a total hip BMD of 0.747 g/cm2 (p < 0.0001, 0.0026, and 0.0002, respectively).
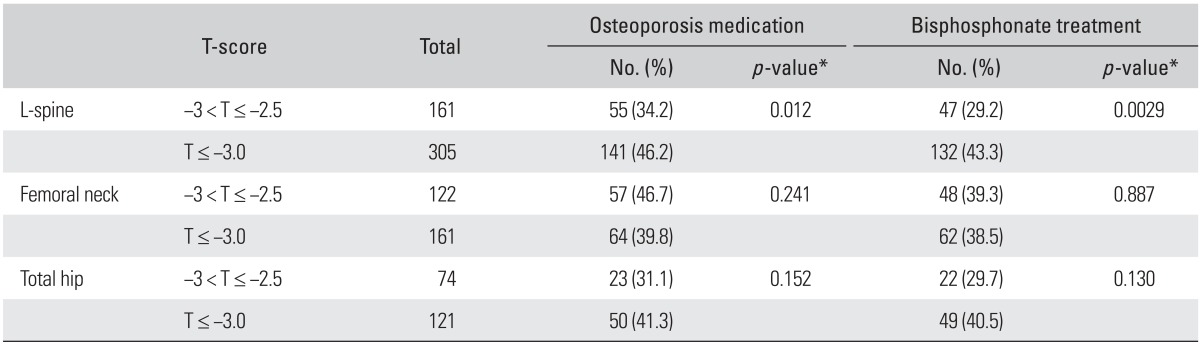
Regarding the lumbar spine, 46.2% of the osteoporosis drugs and 43.3% of bisphosphonates were administered in the T-score ≤ -3.0 group; these administration rates were significantly higher compared to the -3.0 < T-score ≤ -2.5 group that showed an administration rate of 34.2% for osteoporosis drugs and 29.2% for bisphosphonates (p-values equal to 0.012 and 0.0029, respectively) (Table 3). However, based on the femoral neck and total hip, there was no statistically significant difference observed in the administration rate for osteoporosis drugs and bisphosphonate between the T-score ≤ -3.0 group and -3.0 < T-score ≤ -2.5 group.
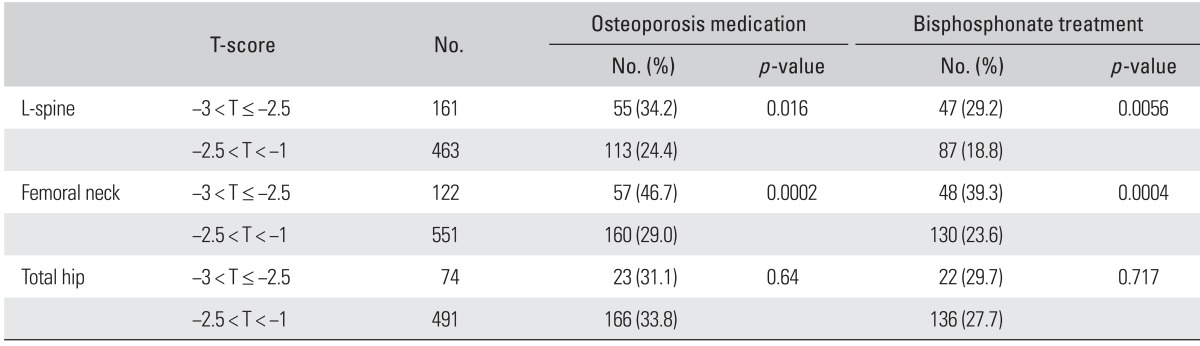
With regards to the lumbar spine and femoral neck, the -3.0 < T-score ≤ -2.5 group was administered osteoporosis drugs (p-values equal to 0.0016 and 0.0002, respectively) and bisphosphonates (p-values equal to 0.0056 and 0.0004, respectively) at a significantly higher rate compared to the -2.5 < T-score < -1 group (Table 4). However, regarding the total hip, significant differences were not present in the administration rate of osteoporosis drugs and bisphosphonates between the -3.0 < T-score ≤ -2.5 group and -2.5 < T-score < -1 group.
The progressive loss of bone mass remains asymptomatic until fractures occur; therefore, many patients with osteoporosis do not realize the need for treatment or the serious consequences. In the case of vertebral fractures, the risk of further fractures increases dramatically after an initial fracture;4,5) in addition, there is an increase in associated kyphotic deformity of the spine, pain, respiratory complications, and mortality.2,6,7) The 1 year mortality rate for hip fractures is around 20%;8,9) subsequently, the prevention of hip fractures is very important. The mortality and significance of osteoporotic vertebral fractures is generally underestimated because the mortality rate after vertebral fractures is reported to be higher than that of hip fractures.10) Therefore, the active prevention of osteoporotic vertebral fractures (especially in relatively high-risk groups) is an excellent way to lower the opportunity costs of morbidity due to fractures as well as reduce mortality rates.
This study shows that the administration rate of osteoporosis drugs in the osteoporosis group was higher than that of the osteopenia group or normal group; in addition, the administration rate of osteoporosis drugs in the osteopenia group was higher compared to the normal group. The administration rate increased as the BMD decreased; however, the administration rate of osteoporosis drugs in the osteoporosis group with a T-score between -2.5 and -3.0 was significantly lower than patients with a T-score less than -3.0. This may be because prescriptions were focused on patients with severe osteoporosis and the NHIS insurance benefits regarding osteoporosis drugs were applied from a T-score less than -3.0 when this study was performed in 2011. Therefore, relatively fewer osteoporosis drug prescriptions were administered to osteoporosis patients with a T-score greater than -3.0. The results imply that a lack of rationale (in terms of medical perspectives) was arbitrarily changed for administrative convenience and applied to the NHIS insurance application criteria; subsequently, medical prescription patterns were significantly altered. Cases with prolonged prescription patterns are expected to increase the fracture risk for high-risk patients who require measures to prevent osteoporosis related fractures. The prevalence of osteoporotic fractures in Asia has rapidly increased.11,12) The percentage of the elderly in the population has increased in Korea along with the prevalence of osteoporotic fractures and the subsequently increased socioeconomic burden. More active treatment is required to prevent osteoporotic fractures.
It was observed in the present study that bisphosphonates were most frequently administered to postmenopausal females who visited outpatient orthopedic clinics; however, SERM was rarely prescribed and this may be because SERM is unfamiliar to orthopedists (even though it is not a hormone). The administration rate for bisphosphonates in the group with a T-score between -2.5 and -3.0 was significantly lower than the group with a T-score under -3.0; this indicated that it was influenced by the NHIS insurance benefit application criteria.
The approximate administration rate of 40% for osteoporosis drugs was exhibited in postmenopausal patients with osteoporosis who visited orthopedic outpatient clinics. Bisphosphonates were the most widely administered osteoporosis drug. The administration rate increased with a decrease in the BMD; however, patients with a T-score between -3.0 and -2.5 showed a significantly lower administration rate compared to patients with a T-score less than -3.0. In conclusion, active treatment is recommended for osteoporosis patients with a high-risk of osteoporotic fractures.
Notes
This work was supported by GlaxoSmithKline Korea. However, no benefits in any form have been or will be received from a commercial party related directly or indirectly to the subject of this manuscript. Yil-Seob Lee was responsible for oversight of this study as an employee of GlaxoSmithKline Korea.
References
1. van der Klift M, de Laet CD, Pols HA. Assessment of fracture risk: who should be treated for osteoporosis? Best Pract Res Clin Rheumatol. 2005; 19(6):937–950. PMID: 16301188.

2. Center JR, Nguyen TV, Schneider D, Sambrook PN, Eisman JA. Mortality after all major types of osteoporotic fracture in men and women: an observational study. Lancet. 1999; 353(9156):878–882. PMID: 10093980.

3. Gold DT. The clinical impact of vertebral fractures: quality of life in women with osteoporosis. Bone. 1996; 18(3 Suppl):185S–189S. PMID: 8777086.

4. Lindsay R, Silverman SL, Cooper C, et al. Risk of new vertebral fracture in the year following a fracture. JAMA. 2001; 285(3):320–323. PMID: 11176842.

5. Wustrack R, Seeman E, Bucci-Rechtweg C, Burch S, Palermo L, Black DM. Predictors of new and severe vertebral fractures: results from the HORIZON Pivotal Fracture Trial. Osteoporos Int. 2012; 23(1):53–58. PMID: 21691843.

6. Kado DM, Browner WS, Palermo L, Nevitt MC, Genant HK, Cummings SR. Vertebral fractures and mortality in older women: a prospective study. Study of Osteoporotic Fractures Research Group. Arch Intern Med. 1999; 159(11):1215–1220. PMID: 10371229.
7. Lau E, Ong K, Kurtz S, Schmier J, Edidin A. Mortality following the diagnosis of a vertebral compression fracture in the Medicare population. J Bone Joint Surg Am. 2008; 90(7):1479–1486. PMID: 18594096.

8. Stavrou ZP, Erginousakis DA, Loizides AA, Tzevelekos SA, Papagiannakos KJ. Mortality and rehabilitation following hip fracture: a study of 202 elderly patients. Acta Orthop Scand Suppl. 1997; 275:89–91. PMID: 9385276.
9. Wolinsky FD, Fitzgerald JF, Stump TE. The effect of hip fracture on mortality, hospitalization, and functional status: a prospective study. Am J Public Health. 1997; 87(3):398–403. PMID: 9096540.

10. Johnell O, Kanis JA, Oden A, et al. Mortality after osteoporotic fractures. Osteoporos Int. 2004; 15(1):38–42. PMID: 14593451.

11. Lau EM. Osteoporosis: a worldwide problem and the implications in Asia. Ann Acad Med Singapore. 2002; 31(1):67–68. PMID: 11885498.
12. Dhanwal DK, Cooper C, Dennison EM. Geographic variation in osteoporotic hip fracture incidence: the growing importance of asian influences in coming decades. J Osteoporos. 2010; 2010:757102. PMID: 20981334.





 PDF
PDF ePub
ePub Citation
Citation Print
Print


 XML Download
XML Download