Abstract
Background
We evaluated the factors that affect pain pattern after arthroscopic rotator cuff repair.
Methods
From June 2009 to October 2010, 210 patients underwent arthroscopic rotator cuff repair operations. Of them, 84 patients were enrolled as subjects of the present study. The evaluation of postoperative pain was conducted by visual analog scale (VAS) scores during postoperative outpatient interviews at 6 weeks, 3 months, 6 months, and 12 months. The factors that were thought to affect postoperative pain were evaluated by dividing into three categories: preoperative, operative, and postoperative.
Results
Pain after arthroscopic rotator cuff repair surgery showed a strictly decreasing pain pattern. In single analysis and multiple regression tests for factors influencing the strictly decreasing pain pattern, initial VAS and pain onset were shown to be statistically significant factors (p = 0.012, 0.012, 0.044 and 0.028, respectively). With regard to the factors influencing lower than average intensity pain pattern for each period, the stiffness of internal rotation at 3 months postoperatively was shown to be a statistically significant factor in single and multiple regression tests (p = 0.017 and p = 0.004, respectively).
Conclusions
High initial VAS scores and the acute onset of pain affected the strictly decreasing postoperative pain pattern. Additionally, stiffness of internal rotation at postoperative 3 months affected the higher than average intensity pain pattern for each period after arthroscopic rotator cuff repair.
Rotator cuff tear is a degenerative shoulder disease, causing pain and dysfunction in patients.1) It is also one of the most common reasons for shoulder operations.2) Arthroscopic rotator cuff repair often results in bone removal, extensive resection of bursal tissue, insertion of hardware, and soft tissue distension from irrigation fluid. Due to the development of technology and disease research in recent years, good clinical results have been reported following rotator cuff repair. However, arthroscopic surgery of the shoulder is still associated with severe postoperative pain, and postoperative pain can in turn affect a patient's rehabilitation and satisfaction, influencing long-term functional outcomes. Research on early postoperative pain control has been conducted, often showing good results.3,4,5,6,7,8,9,10,11,12) However, most literature has assessed early postoperative pain control methods and results only, while the degree of postoperative pain and change patterns during the follow-up period are widely unknown.
In addition, while there is extensive research on factors concerning postoperative function, the literature remains limited regarding factors that affect postoperative pain.13) The absence of long-term studies of postoperative pain and the factors behind postoperative pain make predicting postoperative pain difficult. Our hypothesis is that there are specific factors that definitively affect postoperative pain. The purposes of this study were 1) to evaluate the pattern changes in pain scales over time after a rotator cuff repair operation, 2) to evaluate the difference between groups according to their postoperative pain pattern, and 3) to evaluate the factors that affect the postoperative pain pattern.
From June 2009 to October 2010, 210 patients who had been diagnosed with rotator cuff tears and treated via arthroscopic rotator cuff repair were included as subjects. After obtaining Institutional Review Board approval (No. 12-005) by Inje University Busan Paik Hospital to review patients' charts, a retrospective study was initiated. Inclusion criteria were as follows: (1) posterior superior rotator cuff tear of the supraspinatus and infraspinatus tendons, but not the subscapularis tendon, (2) no concomitant biceps or acromioclavicular joint lesion, (3) 6 weeks, 3 months, 6 months, and 12 months postoperative follow-up was possible, (4) the patients had been treated with the same postoperative medical treatment and rehabilitation according to type of tear size, and (5) different preoperative and postoperative pain character. For patients with small to medium tears, we started a level 1 rehabilitation program for 4 weeks after surgery. After the operation, we supported the shoulder with a K-sling. One day after surgery, we started pendulum exercises and the passive forward flexion exercise. One week after surgery, we carried out active forward flexion exercises, extension exercises and active scapular exercises. On the third postoperative week, we conducted supportive active external rotation exercises from an abducted state. Between the fourth and sixth postoperative weeks, we allowed multidirectional stretching exercises and started internal rotation exercises and cross body adduction exercises as level 2 rehabilitation. From the sixth week to the twelfth week after surgery, we started the phase I strengthening exercises, including resistive scapular strengthening exercises and manual resistive exercises of the rotator cuff and deltoid muscle. Between the twelfth week and sixth month, we allowed sports and job activities. For patients with large to massive tears, the level 1 rehabilitation program lasted for the first six weeks. On the day after surgery, we started pendulum exercises. One week after surgery, we conducted passive forward flexion exercises, passive external rotation exercises, and active scapular exercises. Six weeks after the operation, we allowed multidirectional stretching exercises and started internal rotation exercises, cross body adduction exercises and extension exercises as part of the level 2 rehabilitation. In addition, we carried out isometric exercises of rotator cuff, phase I strengthening exercises, including active scapular exercise. Between the twelfth and sixteenth weeks, we started resistive scapular strengthening exercises, manual resistive exercise of the rotator cuff and deltoid muscle, which was level 3 rehabilitation. On the sixteenth week after surgery, we allowed the patient to resume sports activities and return to his or her job activities as part of the level 4 rehabilitation program.
Patients were excluded for the following reasons: (1) they had undergone operations on the same shoulder previously, (2) had degenerative arthritis and inflammatory arthritis, (3) had a cervical spine lesion, (4) had auto insurance or industrial accident compensation insurance, (5) were diagnosed with neuropsychiatric problems, or (6) an inconsistent change of pain pattern, for example, the patient developed preoperative pain characteristics during postoperative follow-up. Using these criteria, 84 patients among the initial 210 patients were selected as final subjects in the study.
The degree of pain was evaluated by a visual analog scales (VAS)14) score. However, pain is subjective in the sense that it could vary for each patient. Sometimes it could be meaningless itself, so we consider that the degree of pain change in an individual is a more valuable measurement. To evaluate the pain pattern, we took a VAS score at each period. The VAS scores from the first outpatient clinic department visit before surgery were used as the preoperative degree of pain. The evaluation of postoperative pain was conducted by VAS scores during the post-operative outpatient interviews at 6 weeks, 3 months, 6 months, and 12 months. Outpatients were asked to report VAS scores based on when they felt the most severe pain, one week prior to the outpatient interviews. Range of motion (ROM) was checked by a single examiner during outpatient visits both before the operation and then again at 3, 6, and 12 months after the operation. Radiologic evaluation was performed at the postoperative time frames of 3 and 12 months using ultrasonography, and at 6 months using computed tomography (CT) arthrography. The factors that were thought to affect postoperative pain were evaluated after dividing the factors into three groups: preoperative, operative, and postoperative. Age, gender, occupation, pain onset, trauma history, degree of pain, smoking history, synovitis of glenohumeral joint, and the size and degenerative change of the ruptured rotator cuff were evaluated as preoperative factors. The operational method and the number of anchors used were evaluated as operative factors. Stiffness and restoration of the repaired rotator cuff were evaluated as postoperative factors.
We evaluated mean pain during the outpatient follow-up period, and compared changes between visits in addition to determining the pain pattern following the operation. First, we classified the patients that displayed a strictly decreasing pain pattern over our set time points as group I, and the rest as group II. The differences of the preoperative, operative, and postoperative factors between each group were evaluated. We also evaluated the factors influencing the strictly decreasing pain pattern over time. Second, we devised another classification system to elucidate the factors behind low postoperative pain intensity. We defined group A as the group of patients showing lower pain intensity than average for each follow-up period, and we labeled the rest as group B. As we did with group I and group II, we examined the differences in the preoperative, operative, and postoperative factors between group A and group B. We then analyzed the factors behind the lower intensity pain pattern for each follow-up period. Also, the patients were divided into acute onset and chronic onset pain groups. The acute onset pain group consisted of patients who had their operations within 3 months of first noticing pain, while the chronic onset pain group was defined as patients who were operated on at least 3 months after the onset of pain.
Statistical differences for categorical variables between groups were analyzed by a chi-square test. Statistical differences for continuous variables between groups were analyzed by Student t-test. The relationship between variables and postoperative pain pattern was analyzed by a logistic regression test. The level of significance was set at 0.05 by use of SAS ver. 9.0 (SAS Institute, Cary, NC, USA). All statistical analyses were performed by a specialized biostatistician.
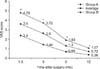
The average pain scores at 6 weeks, 3 months, 6 months, and 12 months after the operation were 4.04 ± 1.78, 3.01 ± 1.79, 1.54 ± 1.18, and 0.85 ± 0.84, respectively. Postoperative pain tended to decrease for every period, and the differences between each period were statistically significant (p = 0.001) (Fig. 1).
The changes in the mean VAS score between 1.5 months and 3 months postoperatively, between 3 months and 6 months postoperatively, and between 6 months and 12 months postoperatively in group I were 1.56 ± 0.96, 1.83 ± 1.24, and 0.7 ± 0.66, respectively. For group I, there were no statistically significant differences in the mean VAS score between any two successive time points. For group II, the changes in the mean VAS score between 1.5 months and 3 months, 3 months and 6 months, and 6 months and 12 months were 1.19 ± 1.10, 2.23 ± 2.08, and 1.01 ± 0.92, respectively. Unlike group I, group II's differences in mean VAS scores between any two successive periods were statistically significant (p = 0.001 and p = 0.001, respectively). The mean VAS score at postoperative 6 weeks, 3 months, 6 months, and 12 months was in 2.4 ± 1.06, 1.44 ± 0.58, 0.66 ± 0.24, and 0.36 ± 0.26, respectively, in group A and 4.79 ± 1.53, 3.72 ± 1.7, 1.93 ± 1.23, and 1.07 ± 0.84, respectively, in group B. There was a statistically significant difference between the groups in the follow-up period (p < 0.05) (Fig. 2).
With regard to continuous factors, initial VAS scores showed a significant difference between group I and group II (p = 0.0161). Other factors, such as age, tear size anterior to posterior (AP), tear size medial to lateral (ML), and number of anchors used were not found to have a statistically significant difference between groups (p = 0.9332, 0.6633, 0.5652, and 0.1561, respectively) (Table 1). Among categorical factors, combined medical disease, pain onset, and synovitis showed a statistically significant difference between group I and group II (p = 0.034, 0.042, and 0.003, respectively). Other factors showed no statistically significant difference between the two groups (Table 2).
With regard to continuous factors, tear size ML showed a significant difference between group A and group B (p = 0.041). Other factors such as age, tear size AP, number of anchors used, and initial VAS score did not show a statistically significant difference between the groups (p = 0.678, 0.147, 0.174, and 0.443, respectively) (Table 3). Among the categorical factors, stiffness of forward flexion, internal rotation and external rotation at 3 months postoperatively, and synovitis were shown to have statistically significant differences between group A and group B (p = 0.006, 0.013, 0.012, and 0.008, respectively). Other factors showed no statistically significant difference between the groups (Table 4).
The results of the continuous and catergorical variables in previous analysis were different from the results of the univariate analysis, so we conducted a multiple regression analysis using the results of univariate analysis.
In single analysis and multiple regression tests for factors influencing the group with the strictly decreasing pain pattern, initial VAS and onset of pain were shown to be statistically significant factors (Table 5). With regard to the factors influencing the lower intensity pain pattern for each period, stiffness of internal rotation at 3 months postoperatively was shown to be a statistically significant factor in both single and multiple regression tests (Table 6).
In the current literature, postoperative pain has been shown to have a strictly decreasing pattern at all given time intervals. In addition, the change in the decrease in pain was statistically significant at all the time intervals. Stiglitz et al.15) also evaluated postoperative pain patterns after arthroscopic shoulder surgery during a 1-year postoperative period. They found that postoperative pain decreases by 7 days after the operation, as compared with the preoperative pain. This result was similar to the results found in the current literature. However, the current literature did not evaluate postoperative pain changes compared with preoperative pain, only evaluating postoperative pain changes themselves. The follow-up time interval in the current study, different from the previous study, is thought to be more consistent for evaluating changes in postoperative pain. The reason for postoperative pain and the changing pattern at different time intervals could not be evaluated in this study. However, we selected subjects who had posterior superior rotator cuff tears and no combined biceps and acromioclavicular lesions among those who had a different character of pain after their operation. By adhering to these strict inclusion and exclusion criteria, the subjects in this study represent uncomplicated postoperative pain during healing periods after an operation. So, the strictly decreasing pain pattern may show an uncomplicated postoperative pain pattern during healing.
Initial VAS and pain onset affected the pattern of pain change during the follow-up period. The higher initial VAS score and acute pain onset affected the strictly decreasing postoperative pain pattern. On the contrary, the lower initial VAS score and chronic pain onset had an irregular effect in terms of decreasing postoperative pain patterns. Desai and Cheung16) assessed the pain of 39 elbow and 38 shoulder surgery patients preoperatively and postoperatively using the Short-Form McGill Pain Questionnaire. Each patient scored their pain both preoperatively and then 3 days and 6 weeks postoperatively. They then calculated changes and correlations at each interval. The researchers found that preoperative pain and the anticipated postoperative pain were both independent predictors of increased postoperative pain. Kuijpers et al.17) evaluated prognostic indicators of favorable outcomes and poor outcomes in narrative reviews from literature on shoulder disorders and suggested that an extended duration of pain is related to worse outcomes. In the current literature, preoperative pain intensity and onset affected the postoperative pain pattern. These results are similar to those of Desai and Cheung16) and Kuijpers et al.17) However, the current study examined patients who had arthroscopic rotator cuff repair and evaluated postoperative pain changes and the factors affecting postoperative pain patterns. This is different from Desai and Cheung's study,16) which evaluated pain changes between the preoperative and postoperative period among heterogeneous subjects, such as those with fracture reduction and nerve decompression. In addition, Kuijpers et al.17) studied prognosis factors for shoulder disorders after non-operative treatment, which is different from our study's inclusion of only arthroscopic rotator cuff repair patients. Further, our research evaluated the factors affecting postoperative pain patterns and is different from Kuijpers et al.,17) as their research showed only the prognostic factors for shoulder disorders. In the current literature, as the initial VAS increases, the pattern of postoperative pain decrease is regular. This study cannot define the pathomechanism of preoperative pain and its effect on the strictly decreasing postoperative pain pattern. In our opinion, these findings may result from continued decreasing pain and better satisfaction among patients who had high levels of pain before their operations. In addition, as the duration of preoperative pain increased, the decrease of postoperative pain was irregular. That may come from synaptic plasticity in chronic pain, which amplifies pain in the spinal cord. Improvement of the shoulder lesion could not be recognized as a pain-decreasing factor.
In the current study, we found that postoperative internal rotation stiffness 3 months after surgery affects the pain intensity for each period. As stiffness becomes worse, postoperative pain remained high, in contrast to the lower levels of postoperative pain in patients who had mild stiffness. Postoperative stiffness was related to a constantly low level of postoperative pain. Loss of motion is a well-recognized postoperative complication of rotator cuff repair.5,18,19,20,21) The risk factors of stiffness are known include calcific tendinitis, adhesive capsulitis, single tendon cuff repair, PASTA repair, age younger than 50, and those with workers' compensation insurance.22) Namdari and Green23) studied 345 patients who underwent rotator cuff repair and researched correlations between preoperative and postoperative variables and postoperative limitations of motion. They evaluated active forward elevation, active external rotation, and passive internal rotation after rotator cuff repair, and found that limitation of motion causes poor operative outcome and worse postoperative pain statistically. This study reached the same result as the study by Namdari and Green,23) which found that ROM loss at 3 months after surgery affects postoperative pain, especially in those with higher than average intensity pain during the follow-up period. However, unlike in this study, the study of Namdari and Green23) includes both open and arthroscopic surgery, and did not observe the pattern of change of postoperative pain during each period throughout follow-up. However, we could not define how the postoperative stiffness affects postoperative pain in our study. Franceschi et al.24) reported that substance P may play a role in the pathogenesis of shoulder pain and found a 3-fold increase in levels of substance P in patients in whom postoperative stiffness developed. In our opinion, this cytokine release in stiffness may be related to postoperative pain intensity.
There are some weaknesses in this study. First, an assessment of postoperative pain may be subjective. Even if the same degree of pain is felt, the VAS score, the digital assessment for pain, could vary for each patient. In this study, therefore, we decided the differences between each patient's VAS score were a weak point, and used the degree of change for pain in a person instead because it is more valuable for comparisons. Second, with regard to evaluating the ROM in order to measure postoperative stiffness, the variables were not presented as a continuous variable, but rather as interval variables. In this way, patients with stiffness could not be completely sorted out. Third, in this study, radiologic evaluations were not carried out in all patients. For instance, CT arthrography was conducted at 6-month postoperation in 80% of the study sample. This could affect bias about postoperative re-rupture and analysis of postoperative pain. Fourth, in this study, subtle differences of pain control medication, including the type, duration, and other therapeutic means, such as injection or physical therapy during the follow-up period were not analyzed. In the future, a study with a stricter control of variables is needed.
In conclusion, noncomplicated postoperative pain after arthroscopic rotator cuff repair surgery showed a strictly decreasing pain pattern at each time interval. As preoperative factors, higher initial VAS scores and a more acute onset of pain affected the strictly decreasing postoperative pain pattern. As a postoperative factor, the stiffness of internal rotation at postoperative 3 months affected the high intensity pain pattern for each period.
So, preoperative factors, such as initial VAS score and pain onset, are not correctable and we consider that these factors could be used to predict the pattern of postoperative pain for patients with these conditions. In addition, the postoperative factors, such as stiffness of internal rotation at postoperative 3 months, are correctable, and we consider that the method of reducing postoperative stiffness could be helpful to reducing postoperative pain intensity.
Figures and Tables
References
1. Iannotti JP. Full-thickness rotator cuff tears: factors affecting surgical outcome. J Am Acad Orthop Surg. 1994; 2(2):87–95.
2. Brislin KJ, Field LD, Savoie FH 3rd. Complications after arthroscopic rotator cuff repair. Arthroscopy. 2007; 23(2):124–128.
3. Bishop JY, Sprague M, Gelber J, et al. Interscalene regional anesthesia for shoulder surgery. J Bone Joint Surg Am. 2005; 87(5):974–979.
4. Boss AP, Maurer T, Seiler S, Aeschbach A, Hintermann B, Strebel S. Continuous subacromial bupivacaine infusion for postoperative analgesia after open acromioplasty and rotator cuff repair: preliminary results. J Shoulder Elbow Surg. 2004; 13(6):630–634.
5. Cho CH, Song KS, Min BW, et al. Multimodal approach to postoperative pain control in patients undergoing rotator cuff repair. Knee Surg Sports Traumatol Arthrosc. 2011; 19(10):1744–1748.
6. Cho NS, Ha JH, Rhee YG. Patient-controlled analgesia after arthroscopic rotator cuff repair: subacromial catheter versus intravenous injection. Am J Sports Med. 2007; 35(1):75–79.
7. Jaureguito JW, Wilcox JF, Cohn SJ, Thisted RA, Reider B. A comparison of intraarticular morphine and bupivacaine for pain control after outpatient knee arthroscopy: a prospective, randomized, double-blinded study. Am J Sports Med. 1995; 23(3):350–353.
8. Oh JH, Kim WS, Kim JY, Gong HS, Rhee KY. Continuous intralesional infusion combined with interscalene block was effective for postoperative analgesia after arthroscopic shoulder surgery. J Shoulder Elbow Surg. 2007; 16(3):295–299.
9. Ritchie ED, Tong D, Chung F, Norris AM, Miniaci A, Vairavanathan SD. Suprascapular nerve block for postoperative pain relief in arthroscopic shoulder surgery: a new modality? Anesth Analg. 1997; 84(6):1306–1312.
10. Scoggin JF 3rd, Mayfield G, Awaya DJ, Pi M, Prentiss J, Takahashi J. Subacromial and intra-articular morphine versus bupivacaine after shoulder arthroscopy. Arthroscopy. 2002; 18(5):464–468.
11. Takada M, Fukusaki M, Terao Y, et al. Postoperative analgesic effect of preoperative intravenous flurbiprofen in arthroscopic rotator cuff repair. J Anesth. 2009; 23(4):500–503.
12. Tetzlaff JE, Brems J, Dilger J. Intraarticular morphine and bupivacaine reduces postoperative pain after rotator cuff repair. Reg Anesth Pain Med. 2000; 25(6):611–614.
13. Burns JW, Hodsman NB, McLintock TT, Gillies GW, Kenny GN, McArdle CS. The influence of patient characteristics on the requirements for postoperative analgesia: a reassessment using patient-controlled analgesia. Anaesthesia. 1989; 44(1):2–6.
14. Scott J, Huskisson EC. Graphic representation of pain. Pain. 1976; 2(2):175–184.
15. Stiglitz Y, Gosselin O, Sedaghatian J, Sirveaux F, Mole D. Pain after shoulder arthroscopy: a prospective study on 231 cases. Orthop Traumatol Surg Res. 2011; 97(3):260–266.
16. Desai VN, Cheung EV. Postoperative pain associated with orthopedic shoulder and elbow surgery: a prospective study. J Shoulder Elbow Surg. 2012; 21(4):441–450.
17. Kuijpers T, van der Windt DA, van der Heijden GJ, Bouter LM. Systematic review of prognostic cohort studies on shoulder disorders. Pain. 2004; 109(3):420–431.
18. Koo SS, Parsley BK, Burkhart SS, Schoolfield JD. Reduction of postoperative stiffness after arthroscopic rotator cuff repair: results of a customized physical therapy regimen based on risk factors for stiffness. Arthroscopy. 2011; 27(2):155–160.
19. Oh JH, Kim SH, Lee HK, Jo KH, Bin SW, Gong HS. Moderate preoperative shoulder stiffness does not alter the clinical outcome of rotator cuff repair with arthroscopic release and manipulation. Arthroscopy. 2008; 24(9):983–991.
20. Papalia R, Franceschi F, Vasta S, Gallo A, Maffulli N, Denaro V. Shoulder stiffness and rotator cuff repair. Br Med Bull. 2012; 104(1):163–174.
21. Tauro JC. Stiffness and rotator cuff tears: incidence, arthroscopic findings, and treatment results. Arthroscopy. 2006; 22(6):581–586.
22. Huberty DP, Schoolfield JD, Brady PC, Vadala AP, Arrigoni P, Burkhart SS. Incidence and treatment of postoperative stiffness following arthroscopic rotator cuff repair. Arthroscopy. 2009; 25(8):880–890.
23. Namdari S, Green A. Range of motion limitation after rotator cuff repair. J Shoulder Elbow Surg. 2010; 19(2):290–296.
24. Franceschi F, Longo UG, Ruzzini L, et al. Circulating substance P levels and shoulder joint contracture after arthroscopic repair of the rotator cuff. Br J Sports Med. 2008; 42(9):742–745.




 PDF
PDF ePub
ePub Citation
Citation Print
Print







 XML Download
XML Download