Abstract
Background
The aim of this study was to describe the mini-open suture bridge technique with porcine dermal patch augmentation for massive rotator cuff tear and to assess preliminary clinical and radiological results.
Methods
Five patients with massive rotator cuff tear for which it was not possible to restore the anatomical footprint underwent mini-open suture bridge repair using a porcine dermal patch. The patients' average age was 53.4 years (range, 45 to 57 years), and the average duration of follow-up was 20.6 months (range, 14 to 26 months). Patients were evaluated with preoperative and postoperative outcome measures, including a visual analog scale (VAS) for pain, the University of California Los Angeles (UCLA) score, and the American Shoulder and Elbow Surgeons (ASES) score. The structural integrity of repaired rotator cuffs was assessed by magnetic resonance imaging 6 months postoperatively.
Results
The average VAS pain score, UCLA score, and ASES score improved from 6.8, 15.4, and 39.4 preoperatively to 0.8, 31.2, and 86.4 postoperatively (p = 0.041, 0.042, and 0.043, respectively). Magnetic resonance images obtained at an average of 8 months after surgery showed that four patients had intact repair integrity with graft incorporation. One patient had a re-tear with partial healing but still had a satisfactory clinical outcome. There was no intraoperative or postoperative complication in any patient.
Symptomatic massive rotator cuff tears pose a particularly complex and difficult challenge for the orthopedic surgeon. Surgical repair of these tears is technically difficult and is associated with a re-tear rate distinctly higher than that associated with the repair of smaller tears.1) Retear rates ranging from 41% to 94% have been reported, depending on factors including the patient's age, tear size, tendon quality, muscle atrophy and fatty infiltration, repair technique, and postoperative rehabilitation.2,3,4,5,6,7,8,9)
In massive rotator cuff tear, all attempts must be made to mobilize tendons so that they can be reattached to their anatomical insertion sites on the greater tuberosity in a tension-free manner.10) Unfortunately, the rotator cuff tear margin cannot always be reduced and repaired completely.11) Thus, there is a continuing need for repair strategies that can augment the repair by mechanically reinforcing it, while biologically enhancing the intrinsic healing potential of the tendon.8)
Scaffolds can provide mechanical support for the repaired rotator cuff and have biological properties that may favorably influence cell proliferation and differentiation, ideally improving tendon-to-bone healing.1) They have been used as a surgical option in active patients with irreparable tears, especially those involving the posterosuperior rotator cuff. Scaffolds derived from synthetic polymers and extracellular matrices of human, porcine, or bovine have been processed and marketed for augmentation in the repair of massive tears.12,13,14,15,16,17) Although animal studies have demonstrated that these various scaffolds may, in fact, enhance rotator cuff healing, clinical data to support their use are limited.15,17,18,19)
Permacol (Covidien, Mansfield, MA, USA) is a biological implant consisting of an acellular scaffold of collagen and elastin, derived from porcine dermal tissue.20) Cross-linking provides resistance to collagenase enzymes that are responsible for the breakdown and resorption of implanted collagen.21) After implantation, the patch supports fibroblast infiltration and revascularization so that it gradually becomes incorporated into the surrounding tissue.21) It has been used successfully for the reconstruction of human connective tissue involving general, urological, and gynecological procedures.20)
However, only four clinical studies of rotator cuff repair using a Permacol patch have been reported, two with satisfactory results and two with disappointing results.21,22,23,24) Furthermore, there are few articles describing the precise surgical technique, an important factor in tendon-to-bone healing, for massive rotator cuff repair with patch augmentation. Thus, this study was conducted to assess a mini-open suture bridge technique with porcine dermal patch augmentation for massive rotator cuff tear and to evaluate preliminary clinical and radiological results.
This study was approved by our Institutional Review Board. All study participants provided written informed consent. In total, 283 patients underwent rotator cuff surgery, performed by a single surgeon at our institution, between 2010 and 2011. Of 35 patients with massive rotator cuff tear, five consecutive patients who underwent a mini-open suture bridge repair using a porcine dermal patch were enrolled in this study. A massive rotator cuff tear was defined as a tear > 5 cm in diameter or as involvement of at least two entire tendons.25) The inclusion criteria were: (1) posterosuperior massive rotator cuff tear, confirmed by magnetic resonance imaging (MRI) and arthroscopic findings, (2) massive rotator cuff tear for which it is not possible to reattach tendons at the anatomical insertion sites despite full mobilization, (3) active individuals aged 60 years or younger, (4) failure of conservative treatment after > 3 months, and (5) no history of previous shoulder procedures. Exclusion criteria were: (1) anterosuperior massive rotator cuff tear, (2) irreparable massive rotator cuff tear that could be only partially repaired despite full mobilization, (3) static superior migration of the humeral head, (4) fatty infiltration affecting ≥ 50% of the rotator cuff musculature, based on the Goutallier classification,26) and (5) inability to comply with the postoperative rehabilitation program.
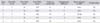
The average age of the patients was 53.4 years (range, 45 to 57 years). There were three men and two women. The average duration of symptoms before surgery was 34.4 months (range, 12 to 72 months), and four dominant arms and one non-dominant arm were affected. The average follow-up period after surgery was 20.6 months (range, 14 to 27 months) (Tables 1 and 2).
With the patient placed in the lateral decubitus position and given general anesthesia, a standard arthroscopic glenohumeral examination and arthroscopic subacromial decompression were performed. The size and location of the torn tendons were evaluated, and careful debridement of the margin of the rotator cuff tear and adhesive tissue was performed.
Then, the torn tendons were repaired with a mini-open technique, using an anterolateral approach.27) A 3- to 4-cm skin incision was made from the anterolateral edge of the acromion to the distal edge, and the raphe between the anterior and middle deltoid was dissected. As torn tendons were tagged with traction sutures, we confirmed the involvement and configuration of the torn tendons by rotating the arm and attempted reduction on the footprint of the greater tuberosity after full mobilization. In selected cases, massive tears could not be repaired to their anatomical insertion sites despite full mobilization, so we used Permacol patch augmentation.
To medialize the footprint of the rotator cuff and insert suture anchors for medial row fixation, we removed 3-4 mm of medial articular cartilage from the junction of the articular cartilage and the medial aspect of the footprint on the greater tuberosity using a ring curette and a burr. The footprint on the greater tuberosity was also debrided. A 6.0-mm Duet suture anchor (Linvatec, Largo, FL, USA) was inserted 3-4 mm medially of the junction of the articular cartilage and the medial aspect of the footprint on the greater tuberosity. Sutures were passed through approximately 7-10 mm of the medial portion of the torn tendons in a mattress manner and then tied with a sliding knot. Depending on the tear size and pattern, two or three suture anchors were used for medial row fixation (Fig. 1A).
To reinforce the repaired rotator cuff, a Permacol patch was created of an appropriate size and configuration. Medial suture limbs then were passed again through the patch and tied with two half-hitch knots. Tied suture limbs from the medial row were fixed at 1.5 cm distal to the lateral edge of the footprint using Footprint suture anchors (Smith & Nephew, London, UK). Additionally, 5-8 marginal sutures using No. 2 non-absorbable sutures (Ethicon, Cornelia, GA, USA) were placed at the medial, anterior, and posterior borders of the grafted patch (Fig. 1B).
Wearing an abduction brace, patients were immobilized until 6 weeks after surgery, and then they started passive range of motion exercises. They began active range of motion exercises at 10 weeks after surgery. Muscle-strengthening exercises were allowed at 4 months and sports and occupational activities at 6 months after surgery.
Patients were evaluated with preoperative and postoperative outcome measures, including a visual analog scale (VAS) for pain, the University of California, Los Angeles (UCLA) score, and the American Shoulder and Elbow Surgeons (ASES) score. The structural integrity of repaired rotator cuffs was evaluated by MRI at 6 months postoperatively. The diagnosis of a fullthickness retear was made when a fluid-equivalent signal or discontinuity of the rotator cuff was found in one or more of the standard T2-weighted images (3 mm intervals).3) Graft incorporation was defined as intermediate signal intensity around the graft with intact continuity on oblique coronal T2-weighted images.3)
Statistical analyses of preoperative and postoperative outcome measures were performed using the Wilcoxon signed-rank test. Statistical significance was set at a p-value of < 0.05.
All patients showed significant pain relief and functional improvement after surgery. The average VAS pain score decreased from 6.8 preoperatively to 0.8 at final follow-up (p = 0.041). The average UCLA score improved from 15.4 preoperatively to 31.2 at final follow-up (p = 0.042). The average ASES score improved from 39.4 preoperatively to 86.4 at final follow-up (p = 0.043).
MRI at an average of 8 months (range, 6 to 12 months) after surgery revealed intact repair integrity with graft incorporation in four patients (Fig. 2). One patient suffered a full-thickness re-tear of the repaired supraspinatus with partial healing of the posterior edge of the rotator cuff and graft incorporation at 8 months after surgery but still had a satisfactory clinical outcome (Fig. 3). No intraoperative or postoperative complication occurred.
The most important finding of this study was that mini-open suture bridge repair with porcine dermal patch augmentation can work well in young patients with high physical demands in whom it is not possible to restore the anatomical footprint of a massive rotator cuff tear. A meticulous repair technique is fundamental to reducing the mechanical forces on the repaired tendon.
The prevalence of massive rotator cuff tears reported in the literature ranges from 10% to 40% of all rotator cuff tears and the treatment of symptomatic massive tears is challenging.1,11) Recent studies of large case series have demonstrated a re-tear rate after repair of 41%-94% in patients with massive tears.2,3,4,5,6,7,8,9) Structural integrity of repaired rotator cuffs has been shown to correlate with clinical improvement, particularly in the recovery of muscle strength.3) Re-tears are believed to result primarily from tension overload, insufficient biological healing at the repair site, or both. Traditional methods for improving tendon-to-bone healing after rotator cuff repair have focused on improving mechanical factors, as with Mason-Allen sutures, suture anchors, and the double-row fixation technique. Recent interest in biological solutions has included the use of scaffolds, platelet-rich plasma, growth factors, and stem cells.
In massive rotator cuff tears, surgeons may find that torn tendons cannot always be reduced and repaired in a tension-free manner. At this point, although there is substantial controversy over the most successful strategy, surgeons have a few treatment options, including simple debridement, partial repair, biceps augmentation, patch grafting, and tendon transfer.1,11,28)
Recently, scaffolds for patch grafting have been derived from synthetic polymers and extracellular matrices of human (dermis), porcine (dermis, small intestine submucosa), or bovine (dermis) sources and used in the treatment of massive rotator cuff tears.12,13,14,15,16,17,21) The rationale for the use of such scaffold devices includes mechanical augmentation by off-loading the repair at time zero and for a period of postoperative healing, biological augmentation, by improving the rate and quality of healing, or both.8,29) Although the validity of scaffolds and the advantages their use have been demonstrated in animal studies, clinical data to support their use are limited.15,17,18,19) Furthermore, numerous questions related to their indication, safety, mechanism of action, and efficacy remain.29)
The Permacol patch, consisting of porcine dermal collagen, has been available since 1998. These patches have been used successfully for the reinforcement of several human body tissues and have been shown to act as durable, permanent tissue scaffolds that assist healing in abdominal, urological, and gynecological procedures.20) The material is purified and cross-linked through a process that makes it resistant to collagenase degradation. It has proven to be strong and to have good cell infiltration and rapid revascularization. The implant is provided in sheet form and may be ideal for the reinforcement of large tendon tears at the repair site.
However, few data are available on complications or limitations of the patch; only four clinical studies of rotator cuff repair using Permacol patch have been reported.21,22,23,24) Proper et al.23) reported that 10 patients had excellent pain relief using a porcine dermal patch with no graft-related adverse effects. However, they did not describe the structural integrity after the repair. Badhe et al.21) reported that grafts were intact in 8 of 10 patients (80.0%) at an average of 4.5 years after repair with porcine dermal patch augmentation. They concluded that the use of porcine dermal patches in the treatment of massive rotator cuff tears produced satisfactory clinical outcomes with regard to safety.
However, Soler et al.24) reported that in all four cases in which a porcine dermal patch was used as a bridging device, the patch failed after 3-6 months despite a promising early postoperative period. Kim and Kim22) reported that 4 of 6 cases (66.7%) had re-tears after rotator cuff repair in which porcine dermal patch was used as bridging devices. In present study, we used porcine dermal patch as augmentation devices. Although there were only five patients in our series, they had satisfactory clinical outcomes, and four patients showed intact repairs and graft incorporation. In view of our results and those reported by other researchers, we believe that use of scaffolds as bridging devices should not be recommended in the treatment of irreparable massive rotator cuff tears.
In the current study, one patient had a full-thickness re-tear but with partial healing of the posterior rotator cuff and graft incorporation. Additionally, that patient had an excellent clinical outcome. Burkhart30) defined a large rotator cuff tear that does not impair function as one involving the supraspinatus tendon and the superior half of the infraspinatus tendon, because balanced force couples are maintained in this setting. Partial healing of the posterior cuff may permit restoration of a stable fulcrum for the glenohumeral joint, maintaining a balanced force couple. This is likely the reason that our patient with a re-tear had an excellent clinical outcome.
It has been demonstrated that several factors are associated with re-tear after rotator cuff repair, including age, tear size, tendon quality, muscle atrophy and fatty infiltration of the rotator cuff, repair technique, and postoperative rehabilitation.1,3,6) One of the most important factors for tendon-to-bone healing in massive rotator cuff repair is the use of a technique that can avoid tension overload. In the case of a massive rotator cuff tear that cannot be adequately reduced and anatomically repaired in a tension-free manner, the most appropriate repair technique is still debatable. Proponents of the single-row technique for retracted tears argue that a single-row repair in a medialized position at the articular margin places the repair under less tension, allowing for biological healing in a reduced-tension environment.10) Advocates of the double-row technique cite superior biomechanical characteristics and an increased contact area for healing, even though it is a high-tension environment.1,10) The surgical technique may contribute to the success or failure of rotator cuff repair using patch grafts.19) To avoid tension overload and to obtain a superior biomechanical environment, we used a combined technique: (1) 3- to 4-mm medialization of the footprint, (2) augmentation with a porcine dermal patch, and (3) double-row suture bridge repair.
This study had several limitations, including the small number of participants, the absence of a control group, and the short follow-up period. However, we did introduce a new repair technique using a porcine dermal patch to reduce the mechanical forces on the repaired tendon and enhance tendon-to-bone healing in massive rotator cuff tears for which restoring the anatomical footprint is not possible. Also, our promising preliminary results, with no graft-related complication, allows the continued application of porcine dermal patch as augmentation devices in selected cases. Prospective randomized, controlled trials are required to assess any benefit over current standard surgical treatment regimens and to determine the correct indications for the use of the scaffold.
In conclusion, mini-open suture bridge repair with porcine dermal patch augmentation can be an option in young patients with high physical demands and massive rotator cuff tears in which it is not possible to restore the anatomical footprint.
Figures and Tables
 | Fig. 1Schematic illustrations of the mini-open suture bridge technique with porcine dermal patch augmentation. (A) Medialization of the footprint and medial row fixation using suture anchors. (B) Suture bridge fixation and marginal sutures with porcine dermal patch augmentation. |
 | Fig. 2Preoperative (A) and postoperative (B) magnetic resonance images. The image obtained 6 months after surgery shows an intact repair with graft incorporation. |
 | Fig. 3Preoperative (A) and postoperative (B, C) magnetic resonance images. Images obtained 8 months after surgery show a full-thickness re-tear of the repaired supraspinatus (B) but with partial healing of the posterior edge of the rotator cuff and graft incorporation (C). |
References
1. Bedi A, Dines J, Warren RF, Dines DM. Massive tears of the rotator cuff. J Bone Joint Surg Am. 2010; 92(9):1894–1908.
2. Galatz LM, Ball CM, Teefey SA, Middleton WD, Yamaguchi K. The outcome and repair integrity of completely arthroscopically repaired large and massive rotator cuff tears. J Bone Joint Surg Am. 2004; 86(2):219–224.
3. Kim JR, Cho YS, Ryu KJ, Kim JH. Clinical and radiographic outcomes after arthroscopic repair of massive rotator cuff tears using a suture bridge technique: assessment of repair integrity on magnetic resonance imaging. Am J Sports Med. 2012; 40(4):786–793.
4. Mellado JM, Calmet J, Olona M, et al. Surgically repaired massive rotator cuff tears: MRI of tendon integrity, muscle fatty degeneration, and muscle atrophy correlated with intraoperative and clinical findings. AJR Am J Roentgenol. 2005; 184(5):1456–1463.
5. Miller BS, Downie BK, Kohen RB, et al. When do rotator cuff repairs fail? Serial ultrasound examination after arthroscopic repair of large and massive rotator cuff tears. Am J Sports Med. 2011; 39(10):2064–2070.
6. Oh JH, Kim SH, Shin SH, et al. Outcome of rotator cuff repair in large-to-massive tear with pseudoparalysis: a comparative study with propensity score matching. Am J Sports Med. 2011; 39(7):1413–1420.
7. Papadopoulos P, Karataglis D, Boutsiadis A, Fotiadou A, Christoforidis J, Christodoulou A. Functional outcome and structural integrity following mini-open repair of large and massive rotator cuff tears: a 3-5 year follow-up study. J Shoulder Elbow Surg. 2011; 20(1):131–137.
8. Ricchetti ET, Aurora A, Iannotti JP, Derwin KA. Scaffold devices for rotator cuff repair. J Shoulder Elbow Surg. 2012; 21(2):251–265.
9. Rousseau T, Roussignol X, Bertiaux S, Duparc F, Dujardin F, Courage O. Arthroscopic repair of large and massive rotator cuff tears using the side-to-side suture technique: mid-term clinical and anatomic evaluation. Orthop Traumatol Surg Res. 2012; 98:4 Suppl. S1–S8.
10. Domb BG, Glousman RE, Brooks A, Hansen M, Lee TQ, ElAttrache NS. High-tension double-row footprint repair compared with reduced-tension single-row repair for massive rotator cuff tears. J Bone Joint Surg Am. 2008; 90:Suppl 4. 35–39.
11. Abrams JS, Song FS. Arthroscopic repair techniques for massive rotator cuff tears. Instr Course Lect. 2012; 61:121–130.
12. Agrawal V. Healing rates for challenging rotator cuff tears utilizing an acellular human dermal reinforcement graft. Int J Shoulder Surg. 2012; 6(2):36–44.
13. Bond JL, Dopirak RM, Higgins J, Burns J, Snyder SJ. Arthroscopic replacement of massive, irreparable rotator cuff tears using a GraftJacket allograft: technique and preliminary results. Arthroscopy. 2008; 24(4):403–409.e1.
14. Coons DA, Alan Barber F. Tendon graft substitutes-rotator cuff patches. Sports Med Arthrosc. 2006; 14(3):185–190.
15. Encalada-Diaz I, Cole BJ, Macgillivray JD, et al. Rotator cuff repair augmentation using a novel polycarbonate polyurethane patch: preliminary results at 12 months' follow-up. J Shoulder Elbow Surg. 2011; 20(5):788–794.
16. Malcarney HL, Bonar F, Murrell GA. Early inflammatory reaction after rotator cuff repair with a porcine small intestine submucosal implant: a report of 4 cases. Am J Sports Med. 2005; 33(6):907–911.
17. Xu H, Sandor M, Qi S, et al. Implantation of a porcine acellular dermal graft in a primate model of rotator cuff repair. J Shoulder Elbow Surg. 2012; 21(5):580–588.
18. Baker AR, McCarron JA, Tan CD, Iannotti JP, Derwin KA. Does augmentation with a reinforced fascia patch improve rotator cuff repair outcomes? Clin Orthop Relat Res. 2012; 470(9):2513–2521.
19. Ide J, Kikukawa K, Hirose J, Iyama K, Sakamoto H, Mizuta H. Reconstruction of large rotator-cuff tears with acellular dermal matrix grafts in rats. J Shoulder Elbow Surg. 2009; 18(2):288–295.
20. Harper C. Permacol: clinical experience with a new biomaterial. Hosp Med. 2001; 62(2):90–95.
21. Badhe SP, Lawrence TM, Smith FD, Lunn PG. An assessment of porcine dermal xenograft as an augmentation graft in the treatment of extensive rotator cuff tears. J Shoulder Elbow Surg. 2008; 17:1 Suppl. 35S–39S.
22. Kim IB, Kim DJ. Arthroscopic xenograft repair of massive, irreparable rotator cuff tears. Clin Should Elbow. 2011; 14(2):214–221.
23. Proper SI, Aladin A, Lam K, Lunn PG. Evaluation of a porcine dermal xenograft (PDX) in the treatment of chronic, massive rotator cuff defects. J Bone Joint Surg Br. 2003; 85:Suppl I. 69.
24. Soler JA, Gidwani S, Curtis MJ. Early complications from the use of porcine dermal collagen implants (Permacol) as bridging constructs in the repair of massive rotator cuff tears: a report of 4 cases. Acta Orthop Belg. 2007; 73(4):432–436.
25. Gerber C, Fuchs B, Hodler J. The results of repair of massive tears of the rotator cuff. J Bone Joint Surg Am. 2000; 82(4):505–515.
26. Goutallier D, Postel JM, Bernageau J, Lavau L, Voisin MC. Fatty muscle degeneration in cuff ruptures: pre- and postoperative evaluation by CT scan. Clin Orthop Relat Res. 1994; (304):78–83.
27. Cho CH, Song KS, Min BW, Jung GH, Lee YK, Sin HK. Anterolateral approach for mini-open rotator cuff repair. Int Orthop. 2012; 36(1):95–100.
28. Rhee YG, Cho NS, Lim CT, Yi JW, Vishvanathan T. Bridging the gap in immobile massive rotator cuff tears: augmentation using the tenotomized biceps. Am J Sports Med. 2008; 36(8):1511–1518.
29. Longo UG, Lamberti A, Rizzello G, Maffulli N, Denaro V. Synthetic augmentation in massive rotator cuff tears. Med Sport Sci. 2012; 57:168–177.
30. Burkhart SS. Arthroscopic treatment of massive rotator cuff tears: clinical results and biomechanical rationale. Clin Orthop Relat Res. 1991; (267):45–56.




 PDF
PDF ePub
ePub Citation
Citation Print
Print



 XML Download
XML Download