Abstract
Background
Anatomic footprint restoration of anterior cruciate ligament (ACL) is recommended during reconstruction surgery. The purpose of this study was to compare and analyze the femoral and tibial tunnel positions of transtibial single bundle (SB) and transportal double bundle (DB) ACL reconstruction using three-dimensional computed tomography (3D-CT).
Methods
In this study, 26 patients who underwent transtibial SB ACL reconstruction and 27 patients with transportal DB ACL reconstruction using hamstring autograft. 3D-CTs were taken within 1 week after the operation. The obtained digital images were then imported into the commercial package Geomagic Studio v10.0. The femoral tunnel positions were evaluated using the quadrant method. The mean, standard deviation, standard error, minimum, maximum, and 95% confidence interval values were determined for each measurement.
Results
The femoral tunnel for the SB technique was located 35.07% ± 5.33% in depth and 16.62% ± 4.99% in height. The anteromedial (AM) and posterolateral (PL) tunnel of DB technique was located 30.48% ± 5.02% in depth, 17.12% ± 5.84% in height and 34.76% ± 5.87% in depth, 45.55% ± 6.88% in height, respectively. The tibial tunnel with the SB technique was located 45.43% ± 4.81% from the anterior margin and 47.62% ± 2.51% from the medial tibial articular margin. The AM and PL tunnel of the DB technique was located 33.76% ± 7.83% from the anterior margin, 45.56% ± 2.71% from the medial tibial articular margin and 53.19% ± 3.74% from the anterior margin, 46.00% ± 2.48% from the medial tibial articular margin, respectively. The tibial tunnel position with the transtibial SB technique was located between the AM and PL tunnel positions formed with the transportal DB technique.
Anatomical anterior cruciate ligament (ACL) graft positioning is considered a key factor for proper postoperative knee function and restoration of the physiologic kinematics of the femorotibial joint in ACL reconstruction.1) Properly placed tibial and femoral tunnels are important because tunnel misplacement can cause graft impingement and changes in graft tension patterns, resulting in knee instability.2) Biomechanical tests on cadaveric reconstructions have demonstrated nearly normal knee kinematics when the tibial tunnel was located close to the center of the tibial footprint and the femoral tunnel was placed in the center of the femoral footprint of the ACL.2)
For decades, the reconstructive option for ACL deficiency has been single bundle (SB) reconstruction with 1 femoral and 1 tibial tunnel. With its simplified procedure, the transtibial tunnel drilling of femoral tunnels was the most widely performed reconstruction technique. However, it is known that the ACL consists of two different bundles, the anteromedial (AM) and posterolateral (PL) bundles, and the double bundle (DB) technique, which aims at restoring the original anatomy of the ACL has also recently gained popularity. 3)
Evaluating the tunnel position using postoperative radiographs after ACL reconstruction is known to be difficult. 4) With the recent advancement of imaging tools and their related programs, three-dimensional computed tomography (3D-CT) is known to provide good visualization of the bony structures with high accuracy.5) Measurement of the ACL tunnel location using 3D-CT has been shown to be reliable,6) and the locations of the tunnel positions of the SB and DB have previously been presented.7) The purpose of this study was to analyze and compare the femoral and tibial tunnel positions of transtibial SB and transportal DB ACL reconstruction using 3D-CT.
Between January 2010 and October 2010, 59 consecutive patients underwent ACL reconstruction using auto-hamstring tendon grafts. Of these 59 patients, six were excluded; four due to revisional ACL reconstruction and two due to combined posterior cruciate ligament reconstruction. Patients were divided into two groups according to the indication of surgery. Patients who had less than a 6-month interval from sustaining the injury to the date of operation were classified as group I. This group consisted of 26 patients who underwent transtibial SB ACL reconstruction using the remnant preservation technique. In ACL reconstruction, remnant preservation would be beneficial in terms of proprioception and rapid healing from remnant vascularity, and the status of remnant tissue may be related to the duration between the injury and surgery.8) Therefore, remnant preservation technique was used in more acute cases because more sufficient and healthier remnant tissue would be present. Patients who had more than a 6-month interval from the sustaining of injury to date of operation were classified as group II. This group consisted of 27 patients who underwent transportal DB ACL reconstruction. There was no statistical difference between the demographic characteristics of the two groups before surgery (p > 0.05) (Table 1). All procedures were performed by a single senior surgeon. The Institutional Review Board approved the study protocol, and all included patients provided written informed consent. To avoid the possible effect of tunnel widening after autograft reconstruction, where the majority (75%) of tunnel widening occurs during the first 3 to 6 months after operation, 9) the postoperative CTs in this study were taken within 1 week of the reconstructive operation. For the precautionary purpose of minimizing radiation exposure, all patients wore lead aprons and lead thyroid collars.
In both procedures, the hamstring autograft tendon was harvested from the affected limb through a transverse 4-cm skin incision among the skin crease over the medial aspect of the proximal tibia. The semitendinosus and gracilis tendons were harvested. A double loop (four-stranded) graft of the hamstring tendon (semitendinosus and gracilis) was made for group I (transtibial SB technique) (Fig. 1A), while triple-stranded semitendinosus (for AM bundle) and triple-stranded gracilis (for PL bundle) grafts were used for group II (transportal DB technique) (Fig. 1B).
The transtibial SB ACL reconstruction was performed with a remnant preservation technique. 8) Conventional anterolateral (AL) and AM portals were created for arthroscopic examination. An accessory AM portal was made for later traction of the sutured remnant tissue and convenience during suturing. A suture hook (ConMed Linvatec, Largo, FL, USA) with a No. 0 polydioxanone synthetic (PDS) thread (Ethicon, Sommerville, NJ, USA) was inserted through the AM portal and passed through the remnant ACL tissue. Both ends of the PDS were retrieved through the far AM portal. The remnant tissue on the tibial side was elevated using a curette and debrided while the remnant ACL stump was retracted to the medial side for protection during ACL reconstruction and better visualization. A tibial tunnel was created using an ACL tibial guide (ConMed Linvatec) set at a 45° angle with the tip of the tibial guide positioned at the central portion of the ACL remnant tissue. The extra-articular landmark of the tibial tunnel was 1 cm above the insertion of the pes anserinus and 1.5 cm medial to the tibial tubercle. After forming the tibial tunnel, a femoral tunnel was made using the transtibial technique between the 10 and 10:30 o'clock position for the right knee and between the 1:30 and 2 o'clock position for the left knee. A reamer 1.0 mm smaller than the graft diameter was introduced, and the femoral tunnel was made at a 32-mm depth and 1 to 2 mm anterior to the posterior cortex. Subsequently, a dilator (ConMed Linvatec) was used to create a tunnel size equal to the graft diameter. 10)
For femoral fixation of the graft and remnant tissue, two sleeves for the RigidFix cross pins (DePuy Mitek, Raynham, MA, USA) were inserted from the lateral side of the lateral femoral condyle through a 1-cm skin incision. After arthroscopically confirming the precise location for insertion of the cross pins, a Maxon 2-0 suture loop was inserted through the inferior sleeve of the cross pin and retrieved at the far AM portal. Then, the ends of the PDS sutures were inserted into the Maxon suture loop and retrieved from the inferior sleeve of the cross pin. After graft passage, a superior cross pin (3.3 mm) was fixed and the graft was tensioned with 20 Lbs of pressure at full extension using a tensionometer (Mitek, Johnson & Johnson, Raynham, MA, USA) before tibial interference screw fixation. Finally, inferior cross pin (2.7 mm) fixation was performed with a slightly smaller tension using the PDS for the remnant tissue. For tibial fixation, bioscrew and post-tie fixation was performed in all cases.
For transportal anatomic DB ACL reconstruction, accurately placed portals were necessary. After formation of routine AL and AM portals, the fat pad was debrided to allow clear visualization of the anterior horn of the medial meniscus. Needle localization was again used to establish the accessory AM portal at this point. When the needle is introduced, it should be directed toward the femoral insertion site to ensure adequate access for later tunnel drilling. The correct position of this portal is significantly more medial than the position of standard medial portals. Therefore, the portal lies close to the medial condyle and careful attention must be taken to avoid iatrogenic cartilage injury.
After examining the rupture patterns of ACL, the femoral footprints of both the AM and PL bundles were carefully defined and marked with a thermal device (Arthrocare Co., Sunnyvale, CA, USA). If it was difficult to delineate the anatomical outer margin of the footprint, osseous landmarks at the femoral origin were used to define the anatomical insertion sites of the two bundles. 11) Notchplasty was not performed. After the femoral and tibial footprints were defined, measurements of the length and width of each insertion sites were collected using a metal ruler.
For creation of the femoral tunnels, the arthroscope was inserted through the AM viewing portal. The centers of the femoral insertion sites of the PL bundle and AM bundle were preliminarily marked with a Steadman awl inserted through the accessory AM portal. The guide pin was directed toward the marked point using the Bullseye femoral footprint guide (ConMed Linvatec) and gently drilled to engage the pin into the provisional hole. After engaging the pin, the knee was fully bent. Placing the knee at a deep flexion angle allowed for a more anteriorly aimed pin. The Sentinal drill bit (ConMed Linvatec), which was matched to the graft size of each bundle, was used for tunnel drilling in order to minimize the chance of a chondral lesion. The 4.5-mm cannulated EndoButton reamer was drilled into the lateral cortex. The EndoButton depth gauge (Smith and Nephew Endoscopy, Andover, MA, USA) was used to measure the distance from the inner aperture to the lateral cortex. The appropriately sized EndoButton (Smith and Nephew Endoscopy) was then chosen. A careful inspection of the bone bridge between the 2 tunnels with the arthroscope in the AM portal was carried out to ensure that no tunnel communication occurred.
The tibial tunnels were then created with the knee flexed at 90°. An ACL tip-guide (ConMed Linvatec) set at 45° was inserted through the accessory AM portal to create the PL tibial tunnel. The tip of the guide was centered at the previously marked anatomic insertion site of the PL bundle. The ACL guide was secured externally over the AM cortex of the tibia just anterior to the leading edge of the superficial medial collateral ligament. A 3.2-mm guide wire was inserted through the drill sleeve and advanced to the footprint of the PL bundle. The ACL tip-guide was then removed from the knee, adjusted to 50°, and reinserted through the AM portal for creation of the AM tibial tunnel. The tip of the guide was again aimed at the center of the anatomic insertion site of the AM bundle, and the drill sleeve was advanced to the AM tibial cortex.
The PL graft was passed first, followed by the AM graft. On the femoral side, an EndoButton CL (Smith and Nephew Endoscopy) was used for femoral-side fixation. In some cases, when the distance between the aperture and the lateral femoral cortex (far cortex) was shorter than 30 mm, an EndoButton Direct (Smith and Nephew Endoscopy) was used to maximize the amount of graft in the tunnel. The grafts were pretensioned by flexing and extending the knee through 20 cycles of full motion. Final fixation of the grafts was conducted at 0° of flexion for AM and PL bundle.
A CT scanner (Light Speed VCT, GE Medical Systems, Milwaukee, WI, USA) was used for all examinations, with data collected within 1 week of surgery for all patients. The collimation was 16 × 0.625 mm, the tube parameters were 120 kVp and 200 mA, and the acquisition matrix was 512 × 512. The field of view was 140 mm and the slice thickness was 0.625 mm. The knee was placed in full extension. The bone was segmented and reconstructed to a 3D point cloud model from the axial CT scan slices with use of Mimics software v14.0 (Materialise, Leuven, Belgium). The reconstructed 3D point cloud bone models were then imported in the commercial package Geomagic Studio v10.0 (Research Triangle Park, NC, USA) for processing into 3D surface models.
Tunnel measurements using 3D-CT were performed as previously developed and described by Forsythe et al.7) Initially, the distal femur model was positioned horizontally in the "strictly lateral position," where both femoral condyles were superimposed as described by Bernard et al.12) for the lateral radiograph of the knee. The model was then rotated to a distal view, and the medial femoral condyle was virtually removed at the highest point of the anterior aperture of the intercondylar notch leaving the lateral femoral condyle. Finally, the model was rotated back to the "strictly lateral position," which was confirmed through superimposition of a full distal femur model. A snapshot of the mediolateral view of the lateral femoral condyle was taken in this lateral position. The locations of the tunnels were quantified from the deepest subchondral contour to the center of the tunnel, and the percentage distance from the intercondylar notch roof was determined (Fig. 2).
The proximal tibial model was initially placed in the posterior view. Then, the model was rotated to visualize the superior aspect of the proximal tibia, and internal rotation and external rotation were adjusted so that the most posterior articular margins of both the medial and lateral tibial condyles were at the same horizontal level. The top view of the proximal tibia was considered satisfactory when the visual axis was perpendicular to the plane of the medial tibial articular margin. This position was verified by turning the model laterally to view the medial aspect, and the degree of flexion or extension was adjusted to align it to the medial articular margin in the vertical direction before the model was returned to the top view. A snapshot of the top view of the proximal tibia was then recorded. The tibial tunnel locations were expressed as percentages measured from the anterior border and the medial border from the total depth (A) and the total width (M) of the proximal tibia, respectively (Fig. 3).
The images of the mediolateral view of the lateral femoral condyle and the top view of the proximal tibia were independently measured, by 2 orthopedic surgeons to evaluate the ACL tunnel positions. The measurement was repeated by both observers after a 2-week interval. ImageJ software (National Institutes of Health, Bethesda, MD, USA) was used to measure the distances and ratios using these images. In this study, arthroscopic terminology was used to describe the position of the femoral tunnel in the notch relative to the flexed knee: shallow or deep and high or low.13)
Clinical evaluations were performed on four occasions: preoperatively, follow-up examination at 6 and 12 months, and finally after two years. The final data consisting of at least 2 years of follow-up were analyzed in this study. Preoperative and postoperative knee functions were evaluated in all the patients using Lysholm knee scores14) to document subjective symptoms; Tegner activity score;15) and the knee ligament standard of the International Knee Documentation Committee (IKDC).16) Preinjury Tegner activity scores and activity level by IKDC guidelines were calculated from what patients reported their activities to be before the time of ACL injury. Ligament instability was examined using a Telos stress radiographic unit (Telos, Weiterstadt, Germany). Differences between the anterior translation of the affected and normal sides were used to determine the degree of laxity. To minimize susceptibility bias, all evaluations were made by one observer not involved in the surgery.
Preoperative demographic data were compared for the 2 groups using a t-test (Fisher exact test for gender.) A preoperative and latest postoperative comparison of Lysholm knee scores, Tegner activity scores, and Telos stress test was performed with a paired-sample t-test. A comparison between the two groups was done using an independent-samples t-test. Preoperative and postoperative IKDC scores were compared and verified by using the Cochran-Mantel-Haenszel test, which was also used to compare the two groups.
The intraobserver and interobserver reliabilities of each measurement were represented by the intraclass correlation coefficient (ICC) and standard error of measurement. The single measured ICC was used to determine intraobserver reliability of measurements obtained on two occasions by each observer. The average measured ICC was used to evaluate interobserver reliability by comparing the mean of two measurements of each variable. The ICC is measured with a value from 0 to 1, where x > 0.80 represents good agreement, a score between 0.60 and 0.79 represents moderate agreement, and x < 0.59 represents poor agreement.
The mean, standard deviation (SD), standard error (SE), minimum, maximum and 95% confidence interval (CI) values were determined for each measurement. The Kolmogorov-Smirnoff test was used to assess the assumption of normality. All statistical analyses were performed with SPSS ver. 12.0 (SPSS Inc., Chicago, IL, USA) and Excel 2007 (Microsoft Co., Redmond, WA, USA). A p-value of less than 0.05 was considered significant.
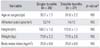
There were no significant differences between the SB and DB patient demographic characteristics (p > 0.05) (Table 1). All patients in the studied group were male with a mean age of 33.7 ± 1.7 years for SB and 31.8 ± 2.2 years for DB ACL reconstruction patients. The ICC demonstrated high intraobserver and interobserver reliability (all values > 0.9). The measurements did not differ based on the surgeon performing the measurements or whether it was the first or second measurement.
The mean diameter of double loop graft used for SB reconstruction technique was 8 ± 1 mm for femoral side and 8 ± 1 mm for the tibial tunnel. The mean diameters of triple-stranded semitendinosus (for AM bundle) and triple-stranded gracilis (for PL bundle) grafts used in DB reconstruction technique for femoral side were 7 ± 1 mm and 5 ± 1 mm, respectively. For tibial side, the graft diameters for AM and PL bundle were 7 ± 1 mm and 5 ± 1 mm, respectively.
The Lysholm knee scoring system was used to analyze subjective symptoms. The mean preoperative Lysholm knee score for all 53 patients was 45 ± 8 points (range, 36 to 67 points) and a postoperative score of 92 ± 5 points (range, 82 to 98 points). This was a statistically significant increase according to the paired-sample t-test (p < 0.01). Preoperatively, 16 patients (30.2%) were rated fair and 37 patients (69.8%) rated poor. At latest follow-up, 22 patients (41.5%) had excellent; 26 (49.1%), good; and 5 (9.4%), fair results. The preoperative mean Lysholm knee scores were 44 ± 7 for SB group (range, 38 to 60) and 48 ± 6 for DB group (range, 42 to 65), without a statistically significant difference (p = 0.124). Both groups demonstrated postoperative increases in knee score. At latest follow-up, the mean score for SB group was 92 ± 5 and 91 ± 4 for DB group, without a statistically significant difference (p = 0.147).
The mean preinjury and preoperative Tegner scores for 53 knees were 8 ± 1.2 (range, 6 to 10) and 2.3 ± 1.3 (range, 1 to 4), respectively. Mean postoperative Tegner score was 7.0 ± 1.3 (range, 4 to 9). Improvement from preoperative to postoperative values was statistically significant (p = 0.027). The mean preoperative score for SB group A was 2.2 ± 1.4 mm (range, 1 to 4 mm), and that for DB group was 2.3 ± 1.1 mm (range, 1 to 4 mm). The mean postoperative score for SB group was 6.8 ± 1.5 mm (range, 4 to 9 mm), and that for DB group was 7.2 ± 1.1 mm (range, 4 to 9 mm). There was no statistical difference between the 2 groups (p = 0.23).
Fifty-one of 53 patients (94.3%) subjectively rated their knee function as normal or nearly normal when compared with preinjury status.
At latest follow-up, 2 patients (7.7%) reported pain during moderate or strenuous activities, and 2 patients (7.7%) reported swelling during moderate or strenuous activities from SB group. From DB group, 2 patients (7.4%) reported swelling during moderate or strenuous activities, and 2 patients (7.4%) displayed symptoms of partial giving way during moderate or strenuous activities.
Final examination of range of motion with a goniometer showed the mean side-to-side difference in knee flexion to be 3.5° ± 2.7° in SB group and 3.2° ± 2.9° in BD group. There was no significant difference (p > 0.05). None of the patients had an extension deficit at their final follow-up examination.
The side-to-side difference, determined using the Telos stress radiographic unit, was 12.3 ± 1.5 mm (range, 10 to 15 mm) preoperatively for all patients. The mean difference for SB group was 12.4 ± 1.5 mm (range, 10 to 15 mm), and that for DB group was 12.2 ± 1.4 mm (range, 10 to 15 mm). Postoperatively, a statistically significant decrease was seen at latest follow-up in all patients, with a mean difference of 3.6 ± 2.2 mm (range, 1 to 8 mm) (p = 0.01). For SB group, the difference decreased to a mean of 3.2 ± 1.6 mm (range, 1 to 7 mm) and 3.4 ± 1.6 mm (range, 1 to 8 mm) for DB group. There was no statistical difference between the two groups (p = 0.33).
The preoperative IKDC values were C (n = 13, 24.5%) and D (n = 40, 75.5%) in all patients. At latest follow-up, the distribution of grades was normal in 22 patients (41.5%); nearly normal in 24 patients (45.3%); abnormal in 6 patients (11.3%); and severely abnormal in 1 patient (1.9%) (Table 2). Statistically significant grade improvement was observed postoperatively compared with preoperative grades (p < 0.01). A group comparison of IKDC showed no statistically significant difference (p = 0.054).
The femoral tunnel for the transtibial SB technique was located at a rather shallow position than the AM tunnel of transportal DB technique. In addition, it was located in a higher position than the PL tunnel of transportal DB technique (Table 3). The femoral tunnel for the SB technique was located 35.07% ± 5.33% in depth and 16.62% ± 4.99% in height (Fig. 2, white dotted circle). The AM tunnel of DB technique was located 30.48% ± 5.02% in depth and 17.12% ± 5.84% in height. The PL tunnel of the DB technique was located 34.76% ± 5.87% in depth and 45.55% ± 6.88% in height (Fig. 2, white plane circles).
The tibial tunnel position with the transtibial SB technique was located between the AM and PL tunnel positions formed with the transportal DB technique (Table 4). The tibial tunnel with the SB technique was located 45.43% ± 4.81% from the anterior margin and 47.62% ± 2.51% from the medial tibial articular margin (Fig. 3, white dotted circle). The AM tunnel of the DB technique was located 33.76% ± 7.83% from the anterior margin and 45.56% ± 2.71% from the medial tibial articular margin. The PL tunnel of the DB technique was located 53.19% ± 3.74% from the anterior margin and 46.00% ± 2.48% from the medial tibial articular margin (Fig. 3, white plain circles).
The most important finding of the present study is: when using the transtibial SB technique for ACL reconstruction, the center of the femoral tunnel was typically positioned shallow form the AM bundle footprint at the height of the femoral condyle. To the author's knowledge, this is the first study directly comparing the tunnel footprints in prospective manner between in vivo primary transtibial SB and transportal DB ACL reconstruction.
Correct-tunnel positioning is essential for successful ACL reconstruction. Erroneous placement of the transplant can result in early graft failure, lack of extension and flexion, and continued instability.17) Especially at the femoral site, small changes in tunnel position have large effects on ACL graft-length patterns in knee motion.1) Zantop et al.18) were able to show that the anatomical placement of the PL bundle results in the restoration of knee kinematics closer to those of the intact knee than when the tunnel is drilled in a nonanatomical position.
During the postoperative course of ACL reconstruction, standard radiographs are frequently used for routine evaluation. However, in the case of soft tissue grafts it is often difficult, or even impossible, to identify the femoral tunnel opening and orientation. A conventional X-ray image contains information from all planes, resulting in an accumulation of shadows as a function of the density of the tissue. The literature has described different methods for the description and evaluation of the femoral insertion sites of the AM and PL bundles. The ratio between femoral length along Blumensaat's line and the distance of the ACL insertion from the posterior border, as proposed by Aglietti et al.,19) was refined by the quadrant method of Bernard et al.12) Edwards et al.20) introduced a surgical modification of this grid based on the quadrant classification of Blumensaat's line by Harner et al.21) Amis and Jakob 22) referenced the circular profile of the posterior and distal lateral femoral condyles with Blumensaat line extended to the anterior and posterior margins of the reference circle. The present study used the modified quadrant method of Bernard et al.12) because it is widely accepted and easy to implement.
For the tibial side, there is broad consensus to describe the insertions as a ratio between the distance of the insertions of the ACL to the anterior margin of the tibial plateau and the broadest diameter of the tibial plateau.22) Aglietti et al.19) described the insertion position as the percentage from the front (along the tangent to the plateaus) of the sagittal length of the tibial plateaus, a method that might be inaccurate, especially in degenerative joints. Anatomic and radiologic study transformed this method for the evaluation of the AM and PL bundles.23) Tsukada et al.24) reported on the insertions of the bundles in the transverse orientation. In contrast to this anatomical study, the present study explored the insertions on axial CT scans to avoid being misled by soft tissue when defining the bony margins of the tibial plateau.
The CT scanners produce 3D stacks of parallel plane images, each of which consists of an array of X-ray absorption coefficients. These slides can be viewed one at a time and only contain information from that one plane. The volume-rendering technique is a technique for visualizing sampled functions of three spatial dimensions by computing 2D projections of a colored, semitransparent volume. The high definition of this technique provides good visualization of the tunnel aperture and the surrounding bony morphology in both the distal femur and proximal tibia models with no artifacts, and 3D assessment of the tunnel position allows accurate quantification of angles, diameters, and distances. In addition to these advantages, appropriate software, such as Mimics v14.0 and Geomagic Studio v10.0 used in this study, improves the accuracy and the reliability through the use of embedded program tools. The 3D-reconstructed model can be cut, rotated, and measured according to the user's intensions. By selectively removing sections of the bone from the model and rotating the model view, regions of the bone that are traditionally difficult to see (e.g., the medial wall of the lateral femoral condyle) can be clearly visualized. Since each bone model is aligned with an anatomically defined coordinate system, measurements are independent of limb orientation during imaging. In addition, the 3D shape of the intercondylar notch precludes the use of conventional 2D-CT scans for measurement of ACL tunnel location.25) The intercondylar notch roof is better delineated on the 3D-CT scan image of the lateral condyle compared with Blumensaat's line, which is a condensation of bone at the intercondylar notch roof on a radiographic image.26) The intercondylar notch roof seen in the mediolateral view of the lateral femoral condyle is located at the highest point of the anterior aperture of the intercondylar notch, which is not always positioned at the middle of the notch because of variation in notch shape. Tunnel position evaluation using 3D-CT has been shown to be highly reliable,6) a conclusion supported by the results of the present study (high ICC with good agreement for all measurements).
The transtibial SB ACL reconstruction technique has been the traditional method for ACL reconstruction. Although the tibial tunnel position of the transtibial SB technique in this study (45.43% from anterior, 47.62% from the medial cortical margin of proximal tibia) was in a rather central position between the AM and PL anatomical footprint, the femoral tunnel position in this study was shallow (35.07% in deep-shallow direction) and high (16.62% from intercondylar notch roof), far from the center of the anatomical attachment site.27) Regarding the position of the femoral tunnel during transtibial guided femoral tunnel drilling, there have been multiple studies showing that most femoral tunnels are placed in a nonanatomical position. Dargel et al.28) reported suboptimal femoral tunnel radiographic position using a transtibial technique with tunnels located in an anterior and vertical position relative to the native footprint. Giron et al.29) reported on the technical impossibility of restoring both the anatomic tibial and femoral origins of the ACL using a transtibial technique despite any modifications. Tunnels tend to be consistently placed superior to the anatomical footprint because of the restricted angulations from the tibial tunnel in the frontal and sagittal planes. The results in this study regarding the femoral footprint of the SB reconstruction technique report similar findings. Modifications of the conventional transtibial technique have been described in an effort to improve femoral tunnel obliquity and restore the native femoral ACL footprint. Some surgeons have advocated independent drilling of the femoral tunnel through the medial arthroscopic portal, with the knee placed in hyperflexion.30) However, direct comparative analysis is beyond the scope of this study.
For the last 5-10 years, many studies have reported the results of anatomic DB ACL reconstruction with various outcomes. While many surgical techniques have described the surgical positioning of the femoral tunnels, there is no accepted criterion to quantify these positions. Through radiographic analysis, Zantop et al.23) studied the insertions of the AM and PL bundles of the ACL on the femoral side, according to the quadrant technique described by Bernard et al.12) The authors showed that the center of the AM bundle was 22.3% of the height of the lateral femoral condyle and 18.5% along Blumensaat's line. The center of the PL bundle was located at 53.6% and 29.3% of the height of the lateral femoral condyle and along the Blumensaat's line, respectively.23) Accordingly, from previous anatomical reports,23) the average position of the center of the AM insertion on the femur was 22% in a deep-shallow direction and at 23.9% in a high-low direction. The center of the PL bundle was reported to be 29.5% in a deep-shallow direction and 52.7% in a high-low direction. When compared with previous studies, the femoral AM and PL tunnels in this study were placed rather shallow (30.48% and 34.76%) and high (17.12% and 45.55%) in the femoral condyle. The average tibial footprints in previous reports were AM 32.5% and PL 47.3% from the anterior border of the tibia.20,23) In the present study, the tibial AM tunnel position (33.76%) was similar to those in previous reports,20,23) however, the tibial PL tunnel was located in a rather deep position (53.19%).
There are some limitations with the present study. One is the small number of patients studied. Another limitation is that only male patients were included. Gender differences were therefore not represented, and further study including females would enhance the significance of the study. The lack of a clinical long-term follow-up may be viewed as another weakness of this study. However, the aim of this study was to determine the postoperative positions of the femoral and tibial tunnels in the SB and DB ACL reconstruction techniques. Tunnel position should be documented before presenting any results from an anatomic ACL reconstruction, and in this respect, 3D-CT scanning is a valuable method. However, we do not advocate the routine use of 3D-CT after ACL reconstruction. While the radiation dose is small, radiation risk might always be a cause of concern. Accordingly, 3D-CTs are recommended in cases of fair clinical outcome, ACL revision surgery, or complications, such as unusual tunnel enlargement.
In conclusion, using the 3D-CT measuring method, the location of the tibia tunnel was between the AM and PL footprints, but the center of the femoral tunnel was at more shallow position from the AM bundle footprint when ACL reconstruction was performed by the transtibial SB technique.
Figures and Tables
 | Fig. 1(A) Double loop (four stranded) graft of hamstring tendon (semitendinosus and gracilis) was made for group I (transtibial single bundle technique). The double loop graft was composed of femoral side (30 mm), intraarticular portion (30 mm), and the rest for tibial tunnel including post-tie fixation. (B) A triple-stranded semitendinosus (for anteromedial bundle, bottom) and triple stranded gracilis (for posterolateral bundle, above), were made for group II (transportal double bundle technique). Each triple loop was composed of femoral side (25 mm), intraarticular portion (25 mm) and the rest for the tibia tunnel. |
 | Fig. 2A view of the lateral femoral condyle in a strictly lateral position, with both condyles superimposed, was obtained from the three-dimensional model using the Geomagic program. Distance D is defined as the total sagittal diameter of the lateral femoral condyle measured along the intercondylar notch roof. Distance H represents the height measured from the intercondylar notch roof to a line tangent to the distal subchondral contour of the condyle. The locations of the tunnels were quantified from the deepest subchondral contour to the center of the tunnel and were presented as the percentage distance from the intercondylar notch roof. The mean positions are expressed as a white dotted circle for the single bundle tunnel and white plane circles for the double bundle tunnels. |
 | Fig. 3The visual axis of the top view of the proximal tibia was perpendicular to the plane of the medial articular margin. A rectangular measurement frame was drawn with the posterior border tangent to the most posterior articular margins of both the medial and lateral tibial condyles. The anterior border of the rectangle was a line tangent to the most anterior articular margin of the medial tibial condyle. The tibial tunnel locations are expressed as percentages measured from the anterior border and the medial border from the total depth (A) and the total width (M) of the proximal tibia. The mean positions are expressed as dotted white circle for the single bundle tunnel and plain white circles for the double bundle tunnels. |
Table 1
Preoperative Patient Characteristics of the Single Bundle and Double Bundle Reconstruction Groups
ACKNOWLEDGEMENTS
The authors thank Ms. Min-Jung Lee for her assistance with the statistical assessment of the data in this study and Ms. Ah-Reum Kim for patient data collection.
References
1. Musahl V, Plakseychuk A, VanScyoc A, et al. Varying femoral tunnels between the anatomical footprint and isometric positions: effect on kinematics of the anterior cruciate ligament-reconstructed knee. Am J Sports Med. 2005; 33(5):712–718.
2. Iriuchishima T, Tajima G, Ingham SJ, et al. Intercondylar roof impingement pressure after anterior cruciate ligament reconstruction in a porcine model. Knee Surg Sports Traumatol Arthrosc. 2009; 17(6):590–594.
3. Kondo E, Yasuda K, Azuma H, Tanabe Y, Yagi T. Prospective clinical comparisons of anatomic double-bundle versus single-bundle anterior cruciate ligament reconstruction procedures in 328 consecutive patients. Am J Sports Med. 2008; 36(9):1675–1687.
4. Hoser C, Tecklenburg K, Kuenzel KH, Fink C. Postoperative evaluation of femoral tunnel position in ACL reconstruction: plain radiography versus computed tomography. Knee Surg Sports Traumatol Arthrosc. 2005; 13(4):256–262.
5. Basdekis G, Christel P, Anne F. Validation of the position of the femoral tunnels in anatomic double-bundle ACL reconstruction with 3-D CT scan. Knee Surg Sports Traumatol Arthrosc. 2009; 17(9):1089–1094.
6. Lertwanich P, Martins CA, Asai S, Ingham SJ, Smolinski P, Fu FH. Anterior cruciate ligament tunnel position measurement reliability on 3-dimensional reconstructed computed tomography. Arthroscopy. 2011; 27(3):391–398.
7. Forsythe B, Kopf S, Wong AK, et al. The location of femoral and tibial tunnels in anatomic double-bundle anterior cruciate ligament reconstruction analyzed by three-dimensional computed tomography models. J Bone Joint Surg Am. 2010; 92(6):1418–1426.
8. Ahn JH, Lee YS, Ha HC. Anterior cruciate ligament reconstruction with preservation of remnant bundle using hamstring autograft: technical note. Arch Orthop Trauma Surg. 2009; 129(8):1011–1015.
9. Hantes ME, Mastrokalos DS, Yu J, Paessler HH. The effect of early motion on tibial tunnel widening after anterior cruciate ligament replacement using hamstring tendon grafts. Arthroscopy. 2004; 20(6):572–580.
10. Ahn JH, Park JS, Lee YS, Cho YJ. Femoral bioabsorbable cross-pin fixation in anterior cruciate ligament reconstruction. Arthroscopy. 2007; 23(10):1093–1099.
11. Ferretti M, Ekdahl M, Shen W, Fu FH. Osseous landmarks of the femoral attachment of the anterior cruciate ligament: an anatomic study. Arthroscopy. 2007; 23(11):1218–1225.
12. Bernard M, Hertel P, Hornung H, Cierpinski T. Femoral insertion of the ACL: radiographic quadrant method. Am J Knee Surg. 1997; 10(1):14–21.
13. Amis AA, Beynnon B, Blankevoort L, et al. Proceedings of the ESSKA scientific workshop on reconstruction of the anterior and posterior cruciate ligaments. Knee Surg Sports Traumatol Arthrosc. 1994; 2(3):124–132.
14. Lysholm J, Gillquist J. Evaluation of knee ligament surgery results with special emphasis on use of a scoring scale. Am J Sports Med. 1982; 10(3):150–154.
15. Tegner Y, Lysholm J. Rating systems in the evaluation of knee ligament injuries. Clin Orthop Relat Res. 1985; (198):43–49.
16. Hefti F, Muller W, Jakob RP, Staubli HU. Evaluation of knee ligament injuries with the IKDC form. Knee Surg Sports Traumatol Arthrosc. 1993; 1(3-4):226–234.
17. Ho JY, Gardiner A, Shah V, Steiner ME. Equal kinematics between central anatomic single-bundle and double-bundle anterior cruciate ligament reconstructions. Arthroscopy. 2009; 25(5):464–472.
18. Zantop T, Diermann N, Schumacher T, Schanz S, Fu FH, Petersen W. Anatomical and nonanatomical double-bundle anterior cruciate ligament reconstruction: importance of femoral tunnel location on knee kinematics. Am J Sports Med. 2008; 36(4):678–685.
19. Aglietti P, Zaccherotti G, Menchetti PP, De Biase P. A comparison of clinical and radiological parameters with two arthroscopic techniques for anterior cruciate ligament reconstruction. Knee Surg Sports Traumatol Arthrosc. 1995; 3(1):2–8.
20. Edwards A, Bull AM, Amis AA. The attachments of the anteromedial and posterolateral fibre bundles of the anterior cruciate ligament. Part 2: femoral attachment. Knee Surg Sports Traumatol Arthrosc. 2008; 16(1):29–36.
21. Harner CD, Marks PH, Fu FH, Irrgang JJ, Silby MB, Mengato R. Anterior cruciate ligament reconstruction: endoscopic versus two-incision technique. Arthroscopy. 1994; 10(5):502–512.
22. Amis AA, Jakob RP. Anterior cruciate ligament graft positioning, tensioning and twisting. Knee Surg Sports Traumatol Arthrosc. 1998; 6:Suppl 1. S2–S12.
23. Zantop T, Wellmann M, Fu FH, Petersen W. Tunnel positioning of anteromedial and posterolateral bundles in anatomic anterior cruciate ligament reconstruction: anatomic and radiographic findings. Am J Sports Med. 2008; 36(1):65–72.
24. Tsukada H, Ishibashi Y, Tsuda E, Fukuda A, Toh S. Anatomical analysis of the anterior cruciate ligament femoral and tibial footprints. J Orthop Sci. 2008; 13(2):122–129.
25. Inoue M, Tokuyasu S, Kuwahara S, et al. Tunnel location in transparent 3-dimensional CT in anatomic double-bundle anterior cruciate ligament reconstruction with the trans-tibial tunnel technique. Knee Surg Sports Traumatol Arthrosc. 2010; 18(9):1176–1183.
26. Farrow LD, Gillespie RJ, Victoroff BN, Cooperman DR. Radiographic location of the lateral intercondylar ridge: its relationship to Blumensaat's line. Am J Sports Med. 2008; 36(10):2002–2006.
27. Gavriilidis I, Motsis EK, Pakos EE, Georgoulis AD, Mitsionis G, Xenakis TA. Transtibial versus anteromedial portal of the femoral tunnel in ACL reconstruction: a cadaveric study. Knee. 2008; 15(5):364–367.
28. Dargel J, Schmidt-Wiethoff R, Fischer S, Mader K, Koebke J, Schneider T. Femoral bone tunnel placement using the transtibial tunnel or the anteromedial portal in ACL reconstruction: a radiographic evaluation. Knee Surg Sports Traumatol Arthrosc. 2009; 17(3):220–227.
29. Giron F, Cuomo P, Edwards A, Bull AM, Amis AA, Aglietti P. Double-bundle "anatomic" anterior cruciate ligament reconstruction: a cadaveric study of tunnel positioning with a transtibial technique. Arthroscopy. 2007; 23(1):7–13.
30. Bedi A, Musahl V, Steuber V, et al. Transtibial versus anteromedial portal reaming in anterior cruciate ligament reconstruction: an anatomic and biomechanical evaluation of surgical technique. Arthroscopy. 2011; 27(3):380–390.




 PDF
PDF ePub
ePub Citation
Citation Print
Print





 XML Download
XML Download