Abstract
Background
Hemiarthroplasty is a common operation to treat femoral neck fracture in elderly patients. The choice of whether to use cemented stem or cementless stem in hemiarthroplasty has been controversial in clinical practice. However, recent trends regarding stem choice in South Korea are not known or documented. In this study, we assessed the trends of stem fixation in hemiarthroplasty for femoral neck fractures in South Korea.
Methods
Data of patients with femoral neck fractures, who were operated on between the years of 2007 and 2011 and were ≥ 50 years old at the time of operation, were obtained from the Health Insurance Review and Assessment Service. All new visits or admissions to clinics or hospitals for femoral neck fractures were identified using the International Classification of Disease Tenth Revision diagnostic code (S720). The trends in the utilization of cemented and cementless hemiarthroplasty were then analyzed.
Hemiarthroplasty has emerged as the standard treatment for displaced femoral neck fractures in elderly patients. However, extant concerns have been expressed in the medical literature regarding whether to use a cemented stem or cementless stem in the hemiarthroplasty procedure.1,2,3,4,5) Although the cemented stem allows for earlier weight-bearing, it is also associated with elevated risk of cement-related adverse events such as cardiopulmonary complications.1,2,6) The cementless fixation has the advantage of biologic fixation that obviates potential cement-related complications. However, the risk of intraoperative femoral fracture remains problematic with its use.2,3,4)
From a global perspective, cemented stems have traditionally been favored in Europe, while cementless stems were more frequently used in the United States.7,8,9,10) Recently, the clinical results of cementless stem procedures have been reported to be comparable with those of cemented stem for femoral neck fracture.2,11,12) While the use of a cemented stem or cementless fixation are known for other countries, the trends of stem use in South Korea are not known.
We assessed the trends of stem fixation in hemiarthroplasty for femoral neck fractures in South Korea during the most recent five years (2007 to 2011), utilizing nationwide data from the Health Insurance Review and Assessment Service (HIRA).
We accessed and analyzed the HIRA nationwide database, which includes nearly all medical claims for South Korean citizens between the years of 2007 and 2011. In South Korea, 97.0% of the population is legally mandated to enroll in the National Health Insurance scheme. (The remaining 3% of the population, who are not insured by the Korean National Health Insurance Program, are either covered by a Medical Aid Program or are temporary or illegal residents.) Patients pay, on average, a 30% co-pay of total medical costs incurred to clinics or hospitals for nearly all medical conditions except for cosmetic surgery or some new unproven therapies not covered by the National Insurance Scheme.
All clinics and hospitals then submit claims data for inpatient and outpatient care; the claims data submitted to the database includes: diagnoses (International Classification of Diseases Tenth Revision, ICD-10), procedures performed, the patient's demographic information, and direct medical costs including used materials. Once the government (HIRA) receives the data, the government pays 70% of total medical costs to the medical provider. Therefore, all patient information, including their medical records, is available from the HIRA database, which has been used for several epidemiological studies.13,14,15)
All new visits or admissions to hospitals in South Korea for femoral neck fractures were recorded prospectively in a nationwide cohort using ICD-10 codes and procedures in the HIRA database. To identify hemiarthroplasty for femoral neck fractures in patients ≥ 50 years of age, the following selections were made: the ICD-10 codes (S72.0), an age cut-off of 50 years for the patient, and procedure (hemiarthroplasty-hip).13,16,17) The cementless-stem group and cemented-stem group were differentiated based on the code of the prostheses used. A procedure with the material code for cement used was categorized in the "cemented-stem group"; the remaining patients who received procedures were, categorized into the "cementless-stem group." These data were retrospectively evaluated to assess the trends of stem fixation in hemiarthroplasty for femoral neck fractures. The HIRA Institutional Review Board approved this retrospective study.
The patients were divided into groups according to their age (50-64, 65-79, and > 80 years) and gender. The trends of fixation method were determined for each group. The chi-square test of independence was used to evaluate whether the proportion of each methods (cementless nail and cemented) changed over the study period. Statistical analyses were conducted using SPSS ver. 15.0 (SPSS Inc., Chicago, IL, USA); statistical significance was accepted for p < 0.05.
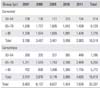
From 2007 to 2011, a total of 33,337 hemiarthroplasties for femoral neck fractures were identified in patients older than 50 years old (Table 1). Of these, the proportion of cementless fixation procedures increased from 42.7% in 2007 to 61.4% in 2011 (p < 0.001) (Fig. 1). Even after stratification by age and gender, the proportion of cementless fixation procedures increased in all groups, and that of cemented fixation showed a corresponding decrease in all groups (Fig. 2).
The choice of stem fixation in hemiarthroplasty for femoral neck fractures is controversial. We calculated recent changes in the proportions of cementless and cemented stem-fixation procedures in South Korea: Overall, the use of cementless fixation procedures increased, while that of cemented fixation procedures decreased.
Some registry-based studies have showed that cemented fixation had better mobility and a higher survival rate among patients compared with cementless fixation.4,5,9,10) However, most of the patients were evaluated using early generation cemented and cementless stems, which are not currently used.5) On the other hand, more recent studies using contemporary stem designs demonstrated that the results of cementless hemiarthroplasty were comparable with or better than those of cemented hemiarthroplasty, without the risk of cardiopulmonary complications.2,11,12)
Indeed, considerable portions of senile patients with femoral neck fractures have cardiopulmonary comorbidities and are vulnerable to cement-related complications.1,2,6) Concerns about cement-related complications might lead the surgeon to change their fixation preference, primarily due to legal concerns. In addition, a skillful cementing technique is demanded to use cemented stems in order to achieve satisfactory results.18,19,20)
Our study shows an increase in the proportion of cementless fixation procedures over the study period in all age groups. We observed a corresponding decrease in the proportion of cemented fixation in all age groups. These findings concur with the results of recent national registry studies on total hip arthroplasty (THA) conducted in several countries. The majority of THA were performed using cementless fixation in Australia, Canada, Denmark, and USA (Table 2).21,22)
There were several limitations to this study. First, the study had a fixed time period: this limitation is because HIRA limited the study period to a maximum of 5 years. Second, other factors for clinical decision-making processes, such as radiographic findings (the morphology of proximal femur and presence of osteoporosis), and demographic characteristics (preinjury ambulatory state and medical comorbidities), were not evaluated. Third, patients who were not hospitalized were not included in this study. However, the number of these patients may be negligible in Korea's health care system; this is because virtually all femoral neck fractures require surgical treatment, and are coded as such in the HIRA database. Fourth, we did not evaluate the clinical outcomes after hemiarthroplasty. However, the purpose of this study was to determine the trends of fixation methods in hemiarthroplasty for femoral neck fractures and not to compare clinical results or outcomes between the two stem-fixation methods.
To the best of our knowledge, this was the first epidemiological study to provide data on the type of stem fixation for hemiarthroplasty for femoral neck fracture in South Korea. Our study demonstrated a shift from cemented fixation to cementless fixation in hemiarthroplasty for femoral neck fractures from 2007 to 2011 in South Korea, which could provide information about contemporary trends of fixation in South Korea.
Figures and Tables
Fig. 1
Proportion of cementless fixation in hemiarthroplasty for femoral neck fractures from 2007 to 2011.
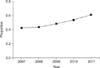
Fig. 2
The age-specific proportions of each fixation method in hemiarthroplasty for femoral neck fractures from 2007 to 2011. (A) 50-64 years of age. (B) 65-80 years of age. (C) > 80 years of age.

References
1. Hossain M, Andrew JG. Is there a difference in perioperative mortality between cemented and uncemented implants in hip fracture surgery? Injury. 2012; 43(12):2161–2164.
2. Taylor F, Wright M, Zhu M. Hemiarthroplasty of the hip with and without cement: a randomized clinical trial. J Bone Joint Surg Am. 2012; 94(7):577–583.
3. Leonardsson O, Karrholm J, Akesson K, Garellick G, Rogmark C. Higher risk of reoperation for bipolar and uncemented hemiarthroplasty. Acta Orthop. 2012; 83(5):459–466.
4. Gjertsen JE, Lie SA, Vinje T, et al. More re-operations after uncemented than cemented hemiarthroplasty used in the treatment of displaced fractures of the femoral neck: an observational study of 11,116 hemiarthroplasties from a national register. J Bone Joint Surg Br. 2012; 94(8):1113–1119.
5. Parker MJ, Gurusamy K. Arthroplasties (with and without bone cement) for proximal femoral fractures in adults. Cochrane Database Syst Rev. 2004; (2):CD001706.
6. Ahn J, Man LX, Park S, Sodl JF, Esterhai JL. Systematic review of cemented and uncemented hemiarthroplasty outcomes for femoral neck fractures. Clin Orthop Relat Res. 2008; 466(10):2513–2518.
7. Hailer NP, Garellick G, Karrholm J. Uncemented and cemented primary total hip arthroplasty in the Swedish Hip Arthroplasty Register. Acta Orthop. 2010; 81(1):34–41.
8. Crossman PT, Khan RJ, MacDowell A, Gardner AC, Reddy NS, Keene GS. A survey of the treatment of displaced intracapsular femoral neck fractures in the UK. Injury. 2002; 33(5):383–386.
9. Rogmark C, Leonardsson O, Garellick G, Karrholm J. Monoblock hemiarthroplasties for femoral neck fractures: a part of orthopaedic history? Analysis of national registration of hemiarthroplasties 2005-2009. Injury. 2012; 43(6):946–949.
10. Kannan A, Kancherla R, McMahon S, Hawdon G, Soral A, Malhotra R. Arthroplasty options in femoral-neck fracture: answers from the national registries. Int Orthop. 2012; 36(1):1–8.
11. Kim YH, Oh JH. A comparison of a conventional versus a short, anatomical metaphyseal-fitting cementless femoral stem in the treatment of patients with a fracture of the femoral neck. J Bone Joint Surg Br. 2012; 94(6):774–781.
12. Klein GR, Parvizi J, Vegari DN, Rothman RH, Purtill JJ. Total hip arthroplasty for acute femoral neck fractures using a cementless tapered femoral stem. J Arthroplasty. 2006; 21(8):1134–1140.
13. Park C, Ha YC, Jang S, Jang S, Yoon HK, Lee YK. The incidence and residual lifetime risk of osteoporosis-related fractures in Korea. J Bone Miner Metab. 2011; 29(6):744–751.
14. Yoon HK, Park C, Jang S, Jang S, Lee YK, Ha YC. Incidence and mortality following hip fracture in Korea. J Korean Med Sci. 2011; 26(8):1087–1092.
15. Lee YK, Jang S, Jang S, et al. Mortality after vertebral fracture in Korea: analysis of the National Claim Registry. Osteoporos Int. 2012; 23(7):1859–1865.
16. Kang HY, Yang KH, Kim YN, et al. Incidence and mortality of hip fracture among the elderly population in South Korea: a population-based study using the national health insurance claims data. BMC Public Health. 2010; 10:230.
17. Lippuner K, Johansson H, Kanis JA, Rizzoli R. Remaining lifetime and absolute 10-year probabilities of osteoporotic fracture in Swiss men and women. Osteoporos Int. 2009; 20(7):1131–1140.
18. Barrack RL, Mulroy RD Jr, Harris WH. Improved cementing techniques and femoral component loosening in young patients with hip arthroplasty: a 12-year radiographic review. J Bone Joint Surg Br. 1992; 74(3):385–389.
19. Russotti GM, Coventry MB, Stauffer RN. Cemented total hip arthroplasty with contemporary techniques: a five-year minimum follow-up study. Clin Orthop Relat Res. 1988; (235):141–147.
20. Harris WH, McCarthy JC Jr, O'Neill DA. Femoral component loosening using contemporary techniques of femoral cement fixation. J Bone Joint Surg Am. 1982; 64(7):1063–1067.
21. Troelsen A, Malchau E, Sillesen N, Malchau H. A review of current fixation use and registry outcomes in total hip arthroplasty: the uncemented paradox. Clin Orthop Relat Res. 2013; 471(7):2052–2059.
22. Huo MH, Dumont GD, Knight JR, Mont MA. What's new in total hip arthroplasty. J Bone Joint Surg Am. 2011; 93(20):1944–1950.




 PDF
PDF ePub
ePub Citation
Citation Print
Print



 XML Download
XML Download