Abstract
Background
Several studies have reported the clinical outcomes of medial ulnar collateral ligament (MUCL) reconstruction of the elbow joint in throwing athletes, including the rate of return to sports. However, little has been known about the imaging outcomes after MUCL reconstruction. The aim of this study is to report the clinical and imaging outcomes after MUCL reconstruction using figure of eight fashion in the elite and professional baseball players.
Methods
This study included 17 baseball players, who underwent MUCL reconstruction between July 2007 and May 2010. The average follow-up period was 48.6 months. Imaging assessment consisted of preoperative plain and stress radiographs, magnetic resonance imaging, and postoperative serial ultrasonography. The clinical assessments were composed of visual analogue scale (VAS) for pain, range of motion, and the Conway scale.
Results
The mean VAS score was 6.4 (range, 3 to 8) preoperatively and 2.2 (range, 0 to 4) postoperatively (p < 0.05). There were nine players (53%) classified as excellent who returned to sports at the same or higher level compared to preinjury. Serial ultrasonography revealed well-maintained grafts at 3 and 12 months in all of the players. Five out of 17 players showed decreased echogenecity in the common flexor tendon at 3 months, which was considered as remaining tissue swelling and resolved completely at 12 months.
The medial ulnar collateral ligament (MUCL) of the elbow is primary static constraint of the ulnohumeral joint to valgus force.1,2) The anterior bundle of the MUCL is the major stabilizing structure of the elbow.3,4) Repeated throwing can lead to microtrauma or rupture of the MUCL.5) The injuries to MUCL of the elbow are most common in the overhead athletes, particularly the baseball players.2,4,6,7,8,9,10) The players with partial tears of the MUCL may return to play after proper rehabilitation. However, those with complete tears, which induce considerable valgus laxity or persistent medial elbow pain, need to have the operation in order to return to sports activities.
Several studies have reported outcomes regarding returning to the preinjury level after MUCL reconstruction, in the throwing athletes. In 1986, Jobe et al.11) firstly described a MUCL reconstruction, reporting 62.5% of return rate in the overhead athletes. The return rates reported in the recent clinical studies vary from 33% to 92%.4,6,12,13,14,15,16) One of the probable reasons for the inconsistent return rate is the innate drawback of the figure eight technique. The previous article reported that the disadvantage of MUCL reconstruction, using figure of eight technique, was difficult to maintain tension because of the high number of holes in medial epicondyle.17)
However, as far as we are aware, no study has evaluated on the integrity of the incorporated grafts, which would validate the success of the surgical treatment. The aim of this study is to report the clinical and image outcomes after MUCL reconstruction, using the figure of eight fashion in high school and elite baseball players. The primary measure for the outcomes was the graft integrity evaluated with ultrasonography, and the secondary measures for the outcomes were postoperative pain, range of motion (ROM), and the Conway scale.
From February 2007, the MUCL reconstruction was performed at our institution by the senior author. This study targeted 17 consecutive baseball players, who underwent the MUCL reconstruction between July 2007 and May 2010 and had postoperative ultrasonographic evaluation.
All of the players were men, with the mean age of 18.7 years (range, 16 to 24 years) at the time of the operation. The average follow-up period was 48.6 months (range, 25 to 64 months). In the study group, six patients were high school baseball pitchers, eight were collegiate baseball pitchers, one was collegiate baseball catcher, one was professional baseball pitcher, and one was professional infielder.
Out of 17 elite baseball players, 6 reported of distinct injury with the sudden onset of symptoms after a single pitch or a throw. The other 11 had no distinct injury, but they stated of the gradual onset of pain in the medial elbow associated with decreased pitching. All of the baseball players had the elbow pain and they experienced loss of velocity and control, or were unable to continue to pitch.
The mean length of time between the onset of symptoms and reconstruction of the ligament was 15.5 months (range, 3 weeks to 6 years). Four players had previous operations on the affected elbow. One had MUCL reconstruction at another hospital 5 years ago. He had revision operation due to re-rupture of the MUCL, 5 months before the operation. Three patients had previous operations for valgus extension overload syndrome (arthroscopic spur resection of olecrenon tip), osteochondritis dissecans of capitellum (arthroscopic microfracture), and loose body (arthroscopic loose body removal).
The indications for the reconstruction were (1) more than 2 mm of valgus laxity of the elbow at stress radiographs, (2) severe medial elbow pain with valgus stress test or (3) complete tear of the anterior band of MUCL that prevented the athlete from throwing or performing at his normal level.
MUCL reconstruction was performed with the flexor-pronator muscle splitting approach, combined with figure of eight fashion graft through ulnar 1-tunnel and humeral 2-tunnel.11,18) Ulnar nerve anterior transposition was performed for the first five cases regardless of the ulnar nerve symptoms, and the remaining 12 cases did not perform the transposition of the ulnar nerve regardless of the presence of ulnar neuropathy. The opposite palmaris longus tendon was used for the autograft in all of the cases.
Before the surgery, plain radiographs including anterioposterior, lateral (extension and flexion), and valgus-stress radiograph, and magnetic resonance image were performed. Valgus-stress radiographs were taken in both arms with the elbow flexed at 30°, under the general anesthesia at the time of the operation. The postoperative ultrasonography was taken at 3 and 12 months, in the involved arm with the elbow flexed at 30° under valgus stress. A specialized radiologist, with 10 years of experience on musculoskeletal ultrasonography, performed all of the follow-up examinations using HDI 5000 system or IU-22 system (both from Philips Healthcare, Bothell, WA, USA).
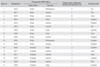
The clinical assessments were composed of the postoperative pain evaluation using visual analogue scale (VAS), valgus stress test, postoperative level of competition measured with ROM, and the Conway scale. The VAS pain score is a horizontal line with 10 cm in length, which is anchored by word descriptors "no pain" on the left side and "very severe pain" on the right side. The Conway scale is divided into excellent, good, fair, and poor, based on the level of competition (Table 1).7)
The elbow was maintained in the hinged brace at 30° of flexion with the forearm in neutral position for 6 weeks. Then, the passive ROM exercise started. The brace was set to allow 30° to 100° in ROM for 3 weeks. After 9 weeks, full ROM exercise was permitted with the arm in the brace. The brace was taken off at 12 weeks postoperation, at which time the athletes started the strengthening exercise program. At 4 months after the surgery, interval throwing program was initiated. At 6 month after surgery, the athlete began to pitch at half of their velocity, and they anticipated returning to their preinjury levels of competition at 9 months.
The mean VAS score was 6.4 (range, 3 to 8) preoperatively and 2.2 (range, 0 to 4) postoperatively (p < 0.05). All of the players had negative valgus stress test, postoperatively. The overall rate of return to play was 77% (13/17). According to the Conway scale, 9 out of 17 (53%) players were classified as excellent, who returned to their preinjury or even higher level, and 4 players (24%) were classified as good, who returned to a lower level (Table 2). The follow-up contacts revealed that 2 players, who were classified as excellent, quitted baseball due to meniscal injury, at 35 months, and due to private affair, at 42 months, after the operation. Preoperative mean ROM was 0.6° hyperextension to 138.5° flexion (range, 10° hyperextension to 150° flexion) and mean postoperative ROM was 0.9° flexion contracture to 134.4° flexion (range, 0° flexion to 140° flexion; p > 0.05).
Serial ultrasonography revealed the well-maintained grafts and intact flexor-pronator muscle at 3 and 12 months in all of the players (Fig. 1). The changes in the graft thickness and flexor-pronator muscle were not observed in the evaluations between 3 and 12 month among all of the players. Five of 17 players showed decreased echogenecity in the common flexor tendon at 3 months, which was considered as remaining tissue swelling, and were resolved completely at 12 months.
Four players had preoperative ulnar nerve symptoms, one of whom received ulnar nerve anterior transposition, and the other three players did not undergo the procedure for the ulnar nerve. Among these three players, two returned to the previous level of competition with resolution of the ulnar nerve symptoms. However, one could not return to play due to persistent ulnar nerve symptom and subsequent posteromedial pain on the affected elbow joint. After the MUCL reconstruction combined with the ulnar nerve anterior transposition, two players complained of the tingling sensation in the 5th finger. One had resolution of the symptom in three months without further procedure. The other had persistent ulnar nerve symptoms and failed to return to play, and he immediate received the ulnar nerve decompression at eight days postoperation. A myositis ossificans occurred in one player who returned to preinjury level of play, which brought mild limitation of the ROM (0°-110°). Flexion contracture was noted of about 5° and 10 ° in two players, both of whom returned to preinjury level of play.
The MUCL reconstruction has evolved to provide successful return to preinjury level of play, since Jobe et al.11) first presented the surgical technique in 1986. The original Jobe technique involved an extensive dissection of the common flexor-pronator mass to expose MUCL origin and transposing the ulnar nerve. The free tendon graft was pulled through the tunnel in figure of eight fashion. However, this technique was reported to cause complications related to postoperative ulnar neuropathy.7,11) Although muscle splitting technique13) was invented to avoid complications related to the surgical approach of Jobe technique, several drawbacks of figure of eight fashion were brought to attention, such as the risk of medial epicondyle fracture as well as the difficulty in maintaining the initial graft tension. However, the graft integrity has not been investigated to validate the effects of the surgical technique. In this study, graft maintenance was evaluated using a serial ultrasonography at 3 and 12 months postoperation, and the first one investigated on the initial fixation failure and the second one decided on the full return to play. The ultrasonography revealed well-maintained grafts in all of the players, without any abnormal findings such as peri-ligamentous fluid collection or graft attenuation. In spite of these favorable imaging outcomes, a total of 8 out of 17 players could not return to preinjury level of play. We considered the reasons for the graft integrity not providing consistent return to play. There are two tentative answers to this. First, the figure of eight fashion involved three large humeral tunnels, and this may consequently increase the risk of making a tunnel in an inappropriate isometric position. Second, Ahmad and ElAttrache19) suggested that the patients with valgus extension overload syndrome need to be evaluated for MUCL insufficiency. They stated that the computed tomography scan was necessary to evaluate the loose body or osteophyte fragmentation. In our cases, one player had arthroscopic olecranon spur resection, due to valgus extension overload syndrome, and another player had arthroscopic micro-fracture, due to osteochondritis dissecans of capitellum. With regard to this, players with MUCL injury should concomitantly be evaluated for intraarticular lesions.
The notable complications were ulnar nerve symptoms. In our 5 early cases, we performed operation on the obligatory ulnar nerve anterior transposition, which resulted in ulnar neuropathy in 2 of the cases. One patient had transient tingling sensation in the 5th finger, immediately after the operation. Another patient did not recover from 5th finger parasthesia. However, in 11 later cases, in which the ulnar nerve transposition was not performed, the complication rate of ulnar nerve neuropathy dropped to 0.09 (1/11). An obvious cause of the ulnar nerve complications would be an extensive mobilization and traction. Furthermore, the medial stability of the elbow would reduce ulnar nerve irritation. Thompson et al.13) demonstrated that exposing the ulnar nerve has no benefit in MUCL reconstruction of the elbow. Postoperatively, he only had 5% of the transient ulnar nerve symptoms and all of the patients were resolved of the symptoms. Therefore, in the patients without ulnar nerve symptoms preoperatively, ulnar nerve anterior transposition should not be performed to decrease surgical complications.
There were several limitations that warrant review. First, small number of enrolled players makes it difficult to fully evaluate the correlation between the clinical and imaging outcomes. Larger populations would be required to validate our findings. Secondly, we studied elite players, and overall return rate reflects on only the elite sports level. Therefore, it is hard to apply our results to the general populations, which include players in the recreational levels. Thirdly, returning to full sports activities could not actually be achieved within 12 months. To confirm the success of the operation, additional evaluation should be performed.
In conclusions, this study demonstrated that well-maintained graft was achieved in all of the players. However, only 53% of the players returned to preinjury level after the MUCL reconstruction using the figure of eight technique. Therefore, the data did not support our hypothesis stating that well-maintained graft would provide successful return to play.
Figures and Tables
 | Fig. 1Postoperative ultrasonography showing patent MUCL graft at 3 months (A) and 12 months (B). The thickness of the incorporated graft is consistent at each evaluation (3.8 mm). MUCL: medial ulnar collateral ligament, ME: medial epicondyle, ST: sublime tubercle of ulna, CF: common flexor tendon. |
Table 1
The Conway Scale

Reprint from Conway et al.7) with permission from The Journal of Bone and Joint Surgery, Inc.
References
1. Ciccotti MG, Jobe FW. Medial collateral ligament instability and ulnar neuritis in the athlete's elbow. Instr Course Lect. 1999; 48:383–391.
2. Hechtman KS, Tjin-A-Tsoi EW, Zvijac JE, Uribe JW, Latta LL. Biomechanics of a less invasive procedure for reconstruction of the ulnar collateral ligament of the elbow. Am J Sports Med. 1998; 26(5):620–624.
3. Morrey BF, An KN. Articular and ligamentous contributions to the stability of the elbow joint. Am J Sports Med. 1983; 11(5):315–319.
4. Schwab GH, Bennett JB, Woods GW, Tullos HS. Biomechanics of elbow instability: the role of the medial collateral ligament. Clin Orthop Relat Res. 1980; (146):42–52.
5. Elattrache NS, Thompson B. Clinical impact of elbow magnetic resonance imaging. Oper Tech Sports Med. 1997; 5(1):33–36.
6. Jobe FW, Nuber G. Throwing injuries of the elbow. Clin Sports Med. 1986; 5(4):621–636.
7. Conway JE, Jobe FW, Glousman RE, Pink M. Medial instability of the elbow in throwing athletes: treatment by repair or reconstruction of the ulnar collateral ligament. J Bone Joint Surg Am. 1992; 74(1):67–83.
8. Azar FM, Andrews JR, Wilk KE, Groh D. Operative treatment of ulnar collateral ligament injuries of the elbow in athletes. Am J Sports Med. 2000; 28(1):16–23.
9. Morrey BF, An KN. Functional anatomy of the ligaments of the elbow. Clin Orthop Relat Res. 1985; (201):84–90.
10. Morrey BF, Tanaka S, An KN. Valgus stability of the elbow: a definition of primary and secondary constraints. Clin Orthop Relat Res. 1991; (265):187–195.
11. Jobe FW, Stark H, Lombardo SJ. Reconstruction of the ulnar collateral ligament in athletes. J Bone Joint Surg Am. 1986; 68(8):1158–1163.
12. Dines JS, Yocum LA, Frank JB, ElAttrache NS, Gambardella RA, Jobe FW. Revision surgery for failed elbow medial collateral ligament reconstruction. Am J Sports Med. 2008; 36(6):1061–1065.
13. Thompson WH, Jobe FW, Yocum LA, Pink MM. Ulnar collateral ligament reconstruction in athletes: muscle-splitting approach without transposition of the ulnar nerve. J Shoulder Elbow Surg. 2001; 10(2):152–157.
14. Feltner ME. Three-dimensional interactions in a two-segment kinetic chain. Part II: application to the throwing arm in baseball pitching. Int J Sports Biomech. 1989; 5(4):420–450.
15. Fleisig GS, Barrentine SW. Biomechanical aspects of the elbow in sports. Sports Med Arthrosc. 1995; 3(3):149–159.
16. Hechtman KS, Zvijac JE, Wells ME, Botto-van Bemden A. Long-term results of ulnar collateral ligament reconstruction in throwing athletes based on a hybrid technique. Am J Sports Med. 2011; 39(2):342–347.
17. Rohrbough JT, Altchek DW, Hyman J, Williams RJ 3rd, Botts JD. Medial collateral ligament reconstruction of the elbow using the docking technique. Am J Sports Med. 2002; 30(4):541–548.
18. Smith GR, Altchek DW, Pagnani MJ, Keeley JR. A muscle-splitting approach to the ulnar collateral ligament of the elbow: neuroanatomy and operative technique. Am J Sports Med. 1996; 24(5):575–580.
19. Ahmad CS, ElAttrache NS. Valgus extension overload syndrome and stress injury of the olecranon. Clin Sports Med. 2004; 23(4):665–676.




 PDF
PDF ePub
ePub Citation
Citation Print
Print


 XML Download
XML Download