Abstract
Background
Several studies have shown that better placement of the acetabular cup and femoral stem can be achieved in total hip arthroplasty (THA) by using the computer navigation system rather than the free-hand alignment methods. However, there have been no comparisons of the relevant clinical advantages in using the computer navigation as opposed to the manual intraoperative measurement devices. The purpose of this study is to determine whether the use of computer navigation can improve postoperative leg length discrepancy (LLD) compared to the use of the measurement device.
Methods
We performed a retrospective study comparing 30 computer-assisted THAs with 40 THAs performed using a simple manual measurement device.
The measurement of leg length discrepancy (LLD) is important in planning a successful total hip arthroplasty (THA). Many clinical and radiological methods with varying degrees of accuracy have been proposed to carry out this measurement. Intraoperative techniques to assess LLD and femoral offset restoration include devices that vary from a Steinmann pin or K-wire, bent to act as a marker or caliper, to specific proprietary devices.1,2,3,4) We also have used a simple manual measurement device, the PCA limb lengthening gauge (Stryker, Mahwah, NJ, USA), to perform the intraoperative leg length measurement. We reported on the accuracy of the device system (Fig. 1) in the previous paper.5) Using this device intraoperatively, the postoperative LLD measured from radiographs was 3.1 mm (range, 0 to 19 mm) on average, and the mean error, calculated as the difference between the radiographic measurements and the intraoperative measurements in absolute values, was 2.1 mm (range, 0 to 7 mm). Other studies have shown that the mean LLD with published techniques was 0.3-9.0 mm and the total range of results for LLD was -22 to +35 mm.6,7,8,9) Thus, the results of our previous study suggest that good equalization of the leg-length after THA was achieved using the manual device.
On the other hand, the use of computer navigation in arthroplasty has been increasing over the last decade, and current research has been performed to evaluate the effectiveness of computer technology. The computed tomography (CT)-based and imageless navigation systems have been compared with the freehand methods, not only in cadaveric studies but also in the clinical patient populations. These studies have shown a higher percentage of acetabular cups implanted within the safe zone when compared to the freehand implantation.10,11,12) There are some studies published on the results of femoral stem placement and evaluation of the effects of navigation on LLD.13,14,15) However, no study has reported on any relevant clinical advantages of using navigation compared to intraoperative measurement devices. We performed a retrospective study comparing 30 computer-assisted THAs with 40 THAs performed using the simple manual measurement device system.
The purpose of this study is to determine whether the use of computer navigation in THA could achieve better results, in terms of postoperative LLD, than a simple measurement device.
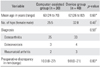
A total of 85 patients who had a unilateral primary THA in our department between August 2002 and July 2007 were included in the study. We excluded 15 patients with the significant hip dysplasia (Crowe 3 or 4), advanced erosive arthritis, and collapse of the femoral head in the contralateral hip, since the equalization of the leg length is not likely to be achieved in these circumstances. None of the remaining 70 patients had undergone previous surgery to the hip, so the contralateral hips are normal or near normal. Thirty patients, who underwent a computer-assisted THA using a CT-based navigation system (CT-based Hip Navigation software, ver. 1.0, Stryker), were included in the computer-assisted group. Forty patients, who underwent a THA using the gauge that we previously studied, were included in the device group. The groups were similar in terms of age and preoperative diagnosis. Intragroup comparisons were made by the Mann-Whitney U-test and chi-squared test. The mean age at the time of the operation was 63 years (range, 24 to 79 years) in the computer-assisted group and 62 years (range, 26 to 82 years) in the device group. The preoperative diagnosis was osteoarthritis (OA) in 58 hips, osteonecrosis of the femoral head in 7 hips, and rheumatoid arthritis (RA) in 5 hips (Table 1). All operations were performed by a single surgeon (TK) through the posterolateral approach, with patients in the lateral decubitus position under the general anesthesia. The postoperative leg length was determined in preoperative planning. Except for the patients whose compensatory lumbar scoliosis was not reversible, the objective was to have no LLD after THA.
To determine the correct socket position in the computer-assisted group, the anterior pelvic plane was intraoperatively identified with a tracker fixed with two 4.0 threaded pins on the same side as the anterior superior iliac spine. Following the dislocation of the hip joint, a femoral tracker was fixed on the distal femur with two more 4.0 threaded pins to determine the leg length. The registration of the pelvis and the femur were completed by surface matching and digitizing over 30 points with a pointer, respectively. The verification points for the pelvis and the femur were set on the posterosuperior portion of acetabular rim and the greater trochanter, respectively. After implantation of the acetabular cup and the femoral stem, their positioning including the leg lengthening was recorded.
In the device group, the leg-length was assessed using the PCA limb lengthening gauge, which is composed of 2 pins (diameter, 3.2 mm) and a gauge. The pins were inserted into the acetabulum and the greater trochanter, and the surgeon measured the distance between the pins (Fig. 1). The pins were inserted to the positions on the lengthening axis before the femoral head was dislocated. The gauge was set between the pins, and the following distances were recorded 3 times during the surgery: before the dislocation, after inserting the trial components, and after setting the real prosthesis. The gauge and the pins on the femoral side were removed during the surgical operation (Fig. 2). The level of the femoral neck osteotomy and the implant neck length were adjusted according to the distance measured after inserting the trial components. The difference between the length before the femoral head dislocation (first measurement) and the length after setting the real prosthesis (third measurement) was determined as the intraoperative leg-lengthening.
Preoperative and postoperative LLD measurements were made using the radiographs. The anteroposterior radiographs of the pelvis were obtained preoperatively and postoperatively in a standardized fashion with both hips extended and internally rotated. The leg-length was obtained as the distance between the lines that connect the lowest edge of the right and left tear drop to the most prominent point of the lesser trochanter.
We compared the preoperative and postoperative radiographic measurements with the intraoperative measurements in each groups, and evaluated the correlation between the two values (Pearson coefficient of correlation).
There are no statistically significant differences in patient demographics or in preoperative LLD between the two groups. The mean preoperative LLD on radiographs was 10.0 mm (range, 0 to 27 mm) in the computer-assisted group and 9.8 mm (range, 0 to 21 mm) in the device group. The mean value of the radiographic measurements on leg lengthening was 12.0 mm (range, 0 to 27 mm) in the computer-assisted group and 9.7 mm (range, 0 to 21 mm) in the device group, and the intraoperative measurements were 13.0 mm (range, 0 to 23 mm) and 10.4 mm (range, 0 to 20 mm), respectively. The Pearson correlation coefficients between the two values were 0.88 (p < 0.001) and 0.89 (p < 0.001). The significant correlations between radiographic and intraoperative measurements were observed in each group (Fig. 3). Postoperative LLD was on the average of 3.0 mm (range, 0 to 8 mm) in the computer-assisted group and 2.9 mm (range, 0 to 10 mm) in the device group. The mean errors between the radiographic measurements and the intraoperative measurements were 2.4 mm (range, 0 to 6 mm) and 2.1 mm (range, 0 to 7 mm), respectively. Statistically significant differences in postoperative LLD and measurement error were not seen between the two groups (Table 2). Two patients had a postoperative LLD of 6 mm or greater in the computer-assisted group compared to seven patients in the device group. All patients in this seven, we had recognized the loosening of the pins with osteoporotic bones during surgery.
This difference was not statistically significant (Fig. 4). In neither group did the postoperative LLD exceed 2 cm. No intraoperative complications were encountered in either group.
The leg length equality is an important functional parameter that is strongly related to the success in THA. The LLD can contribute to hip instability, ipsilateral knee pain, low back pain, sciatic nerve palsy, and aseptic prosthesis loosening.2,6,16) These problems can lead to revision surgeries and may even be the sources of litigation.2,9) Edeen et al.16) and Ranawat et al.3) wrote that the leg-length difference must be 10 mm or less, in order for a patient to have a good quality of life. In spite of the careful attention, an unexpected difference of 10-16 mm can sometimes occur.2,16) The possible reasons are the excessive acetabular reaming during the surgery, sinking of the collarless stem, flexion contracture of the hip joint before the surgery, inaccurate preoperative planning based on the radiographs at several different magnifications, and an inexperienced surgeon. The minor discrepancies of up to 1cm are usually asymptomatic, but in some patients even a small discrepancy may be a source of dissatisfaction.2,16)
Avoiding postoperative LLD remains an important focus for all surgeons performing THA. To this end, a number of techniques have been proposed to assess leg length intraoperatively, which can produce varying results.13,14,15) For example, published methods include the use of an 'L' shaped caliper to allow measurement of the long axis of the femur,4) a carpenter's or dual pin calipers to minimize loosening,17) and direct measurement with a ruler.6) We have demonstrated that the PCA limb lengthening gauge provides equivalent or even more precise data, with less error, on the postoperative leg-length compared to the devices introduced in these reports. In the present study, which considers only the postoperative LLD, the gauge was as good as CT-based navigation; but the cup and stem alignments are not examined. The disadvantage of this device is loosening of the pins in patients with osteoporotic bones, because the pin on the femur is removed during surgery causing it to become easily loosened. The inaccurate abduction/adduction repositioning of the femur with respect to the pelvis also can cause substantial error in the measurement of the length and can offset changes.18) These points should be improved in order to achieve more accurate measurements.
Recently, quite sophisticated intraoperative support systems, such as computer navigation systems, have been developed for more precise surgery. Several studies have shown that better placement of the acetabular cup and femoral stem can be achieved in THA, using either a CT-based or image-free computer navigation system than using the free-hand alignment methods. The authors of many of these studies suggest that the technological advances now available could result in more accurate implant alignment, translating into better stability, performance, and survivorship.10,11,12,13,14,15) The range of LLD cases, in which such a navigation system has been used, is well reported in the literature. Manzotti et al.13) used image-free navigation and reported that the postoperative LLD was 5.06 ± 2.99 mm and the LLD was within 12 mm in all of their patients. Murphy and Ecker15) used CT-based navigation and reported that postoperative LLD and measurement errors were 6.1 ± 4.3 mm (range, -5 to 20 mm) and -0.5 ± 1.77 mm (range, -5 to 3.9 mm), respectively. In this study, postoperative LLD was 3.0 ± 2.0 mm (range, 0 to 8 mm) and within 5 mm in 93%. The measurement error, which is the difference between the postoperative measurements and intraoperative records, was 2.4 ±1.7 mm (range, 0 to 6 mm). Our study showed reasonable and equivalent results compared to these previous reports and showed that CT-based navigation is reliable for leg length adjustment.
However, there is no literature demonstrating any relevant clinical advantages of using navigation compared to manual intraoperative measurement devices. Our study shows quite acceptable equalization of the leg-length after THA, using both computer navigation and a simple manual device. Although there are no statistically significant differences between the two groups, we had fewer cases with the residual discrepancy greater than 6 mm and a lower number of cases with postoperative over-lengthening in the computer-assisted group. This shows the possibility that using CT-based navigation, compared to the simple manual measurement device system, could enhance the surgeons' ability to correct LLD with a lower number of outliers from preoperative planning.
We recognize that our study has some limitations. First, postoperative evaluation was based on the plain pelvic radiographs instead of the CT scans, which have been used in other studies to eliminate the variables of pelvic tilt that exists while taking radiographs.19,20) Various authors have pointed out that the linear measurements and calculations from plain X-rays are susceptible to error, due to variations in positioning of the pelvis relative to the plane of the film and the divergence of the X-ray beams.15,20)
In our study, the plain pelvic radiographs did not always guarantee the neutral positioning of the hip in all cases. On the other hand, CT based navigation measured leg length with the pelvis and femur in a standardized position. It was not fair to compare these data sets, so further evaluation based on CT scans will be needed. Secondly, since this was a retrospective analysis, the patients were not randomized and the follow-ups were too short to detect differences in the clinical outcomes. Finally, the number of cases in each group was small, and as a result, we may not have detected all the clinical differences between the two groups. Further accumulation of cases will be needed. Based on the number of outliers (> 6 mm LLD), it appears that the computer-assisted group may present an advantage when the number of cases are increased.
The results of this study indicate that both methods result in acceptable equalization of the leg length after THA in radiological assessment.
Figures and Tables
Fig. 1
PCA limb lengthening gauge. The left pin goes into the acetabulum, and the right pin into the femur. A stopper and a thread cutting are added to the pin for the acetabulum.
Fig. 2
(A) Intraoperative photograph in the device group. The lengthening axis is marked and the device is placed. (B) A scheme showing the location of the device.

References
1. McGee HM, Scott JH. A simple method of obtaining equal leg length in total hip arthroplasty. Clin Orthop Relat Res. 1985; (194):269–270.
2. Woolson ST, Harris WH. A method of intraoperative limb length measurement in total hip arthroplasty. Clin Orthop Relat Res. 1985; (194):207–210.
3. Ranawat CS, Rao RR, Rodriguez JA, Bhende HS. Correction of limb-length inequality during total hip arthroplasty. J Arthroplasty. 2001; 16(6):715–720.
4. Shiramizu K, Naito M, Shitama T, Nakamura Y, Shitama H. L-shaped caliper for limb length measurement during total hip arthroplasty. J Bone Joint Surg Br. 2004; 86(7):966–969.
5. Maeda T, Kabata T, Ebara H. A gauge for limb length measurement during total hip arthroplasty. J Joint Surg. 2006; 25:452–455.
6. Hofmann AA, Bolognesi M, Lahav A, Kurtin S. Minimizing leg-length inequality in total hip arthroplasty: use of preoperative templating and an intraoperative x-ray. Am J Orthop (Belle Mead NJ). 2008; 37(1):18–23.
7. White TO, Dougall TW. Arthroplasty of the hip: leg length is not important. J Bone Joint Surg Br. 2002; 84(3):335–338.
8. Konyves A, Bannister GC. The importance of leg length discrepancy after total hip arthroplasty. J Bone Joint Surg Br. 2005; 87(2):155–157.
9. Jasty M, Webster W, Harris W. Management of limb length inequality during total hip replacement. Clin Orthop Relat Res. 1996; (333):165–171.
10. Sugano N, Nishii T, Miki H, Yoshikawa H, Sato Y, Tamura S. Mid-term results of cementless total hip replacement using a ceramic-on-ceramic bearing with and without computer navigation. J Bone Joint Surg Br. 2007; 89(4):455–460.
11. Ybinger T, Kumpan W, Hoffart HE, Muschalik B, Bullmann W, Zweymuller K. Accuracy of navigation-assisted acetabular component positioning studied by computed tomography measurements: methods and results. J Arthroplasty. 2007; 22(6):812–817.
12. Langlotz U, Grutzner PA, Bernsmann K, et al. Accuracy considerations in navigated cup placement for total hip arthroplasty. Proc Inst Mech Eng H. 2007; 221(7):739–753.
13. Manzotti A, Cerveri P, De Momi E, Pullen C, Confalonieri N. Does computer-assisted surgery benefit leg length restoration in total hip replacement? Navigation versus conventional freehand. Int Orthop. 2011; 35(1):19–24.
14. Schmerwitz U. Total hip arthroplasty: first experiences with pinless THA software to determine leg length and offset. Orthopedics. 2007; 30:10 Suppl. S124–S126.
15. Murphy SB, Ecker TM. Evaluation of a new leg length measurement algorithm in hip arthroplasty. Clin Orthop Relat Res. 2007; 463:85–89.
16. Edeen J, Sharkey PF, Alexander AH. Clinical significance of leg-length inequality after total hip arthroplasty. Am J Orthop (Belle Mead NJ). 1995; 24(4):347–351.
17. Bose WJ. Accurate limb-length equalization during total hip arthroplasty. Orthopedics. 2000; 23(5):433–436.
18. Sarin VK, Pratt WR, Bradley GW. Accurate femur repositioning is critical during intraoperative total hip arthroplasty length and offset assessment. J Arthroplasty. 2005; 20(7):887–891.
19. Haaker RG, Tiedjen K, Ottersbach A, Rubenthaler F, Stockheim M, Stiehl JB. Comparison of conventional versus computer-navigated acetabular component insertion. J Arthroplasty. 2007; 22(2):151–159.
20. Kalteis T, Handel M, Bathis H, Perlick L, Tingart M, Grifka J. Imageless navigation for insertion of the acetabular component in total hip arthroplasty: is it as accurate as CT-based navigation? J Bone Joint Surg Br. 2006; 88(2):163–167.




 PDF
PDF ePub
ePub Citation
Citation Print
Print





 XML Download
XML Download