Abstract
Curved periacetabular osteotomy (CPO) was developed for the treatment of dysplastic hips in 1995. In CPO, the exposure of osteotomy sites and osteotomy of the ischium are made in the same manner as Bernese periacetabular osteotomy, and iliac and pubic osteotomies are performed in the same manner as rotational acetabular osteotomy. We studied the dynamic instabilities of 25 dysplastic hips before and after CPO using triaxial accelerometry. Overall magnitude of acceleration was significantly decreased from 2.30 ± 0.57 m/sec2 preoperatively to 1.55 ± 0.31 m/sec2 postoperatively. Pain relief and improvement of acetabular coverage resulting from acetabular reorientation seem to be related with reduction of dynamic instabilities of dysplastic hips. Isokinetic muscle strengths of 24 hips in 22 patients were measured preoperatively and after CPO. At 12 months postoperatively, the mean muscle strength exceeded the preoperative values. These results seem to be obtained due to no dissection of abductor muscles in CPO. The preoperative presence of acetabular cysts did not influence the results of CPO. An adequate rotation of the acetabular fragment induced cyst remodeling. Satisfactory results were obtained clinically and radiographically after CPO in patients aged 50 years or older. CPO alone for the treatment of severe dysplastic hips classified as subluxated hips of Severin group IV-b with preoperative CE angles of up to -20° could restore the acetabular coverage, weight-bearing area and medialization of the hip joint. CPO without any other combined procedure, as a treatment for 17 hips in 16 patients with Perthes-like deformities, produced good mid-term clinical and radiographic results. We have been performing CPO in conjunction with osteochondroplasty for the treatment of acatabular dysplasia associated with femoroacetabular impingement since 2006. The combined procedure has been providing effective correction of both acetabular dysplasia and associated femoral head-neck deformities without any increased complication rate. We have encountered an obturator artery injury in one case and two intraoperative comminuted fractures. Although serious complications such as motor nerve palsy, deep infection, necrosis of the femoral head or acetabulum, and delayed union or nonunion of the ilium were reported, such complications have never occurred in our 700 cases so far.
Developmental dysplasia of the hip is one of the most common causes of osteoarthritis (OA) of the hip.1) In Japan, more than 70% of hip OA is caused by developmental dysplasia of the hip.2,3) Total hip arthroplasty is the most effective procedure for older patients with advanced or end stage OA of the hip. However, disappointing results after total hip arthroplasy have been described in younger patients.4,5,6,7) In comparison of their cost-effectiveness in terms of cost per quality-adjusted life year for the young adult, periacetabular osteotomy is more cost-effective in the early stage of OA of the hip than total hip arthroplasty.8)
The most physiological solution for a young adult who has a dysplastic hip is redirection of the acetabulum into a normal position. The Bernese periacetabular osteotomy, developed by Ganz et al.,9) provides good coverage of the femoral head by redirecting the acetabulum. This osteotomy preserves the vascular supply of the transferred acetabulum and allows considerable medialization of the hip joint, but it has several disadvantages due to the asphericity of the osteotomy surfaces. Because this osteotomy is a series of straight cuts, incongruity at the site of the osteotomy and anterior displacement of the hip joint may occur in patients who need an extensive acetabular reorientation.10) Because a gap is created at the site of the osteotomy, bone grafting and relatively rigid fixation with hardware are needed to secure the rotated acetabular fragment. To reduce these drawbacks, curved periacetabular osteotomy (CPO) was developed for the treatment of hip dysplasias in 1995.11) In CPO, the exposure of osteotomy sites and osteotomy of the ischium are made in the same manner as the Bernese periacetabular osteotomy, and iliac and pubic osteotomies are performed in the same manner as a rotational acetabular osteotomy.12) In this review, we described our investigations to solve a number of problems concerning dysplastic hips, and our experience performing CPO on more than 700 hips.
In dysplastic hips, there are two major factors leading to OA of the hip: mechanical overload and instability, resulting from inadequate osseous coverage of the femoral head. Although mechanical stress on dysplastic hips has been widely described, the dynamic instability has not been evaluated quantitatively in clinical cases. We have investigated the dynamic instability of 48 hips in 24 patients with unilateral hip dysplasia (center-edge [CE] angle < 25°) by evaluating their walking patterns under routine conditions using triaxial accelerometry.13) The overall magnitude of acceleration of the dysplastic hips was significantly larger than that of normal hips, with an increase in the dynamic instability of the hip in proportion to the degree of dysplasia (CE angle). We have also studied the dynamic instabilities of 25 dysplastic hips preoperatively and 1 year postoperatively in hip patients receiving CPO using triaxial accelerometry.14) The overall magnitude of acceleration was significantly decreased from 2.30 ± 0.57 m/sec2 preoperatively to 1.55 ± 0.31 m/sec2 postoperatively. The Harris hip score improved from 78.08 points preoperatively to 95.36 points postoperatively, and radiographic parameters all showed significant improvements. This study suggests that the pain relief and improvement of acetabular coverage resulting from acetabular reorientation is strongly related to the reduction in the dynamic instabilities of dysplastic hips.
The acetabular rim and labrum in the area with inadequate osseous coverage of the femoral head is subject to abnormal stress and instability, which may cause the labrum to rupture and a fragment of bone to separate from the adjacent bone margin.15) In our study of the tensile properties of the human acetabular labrum among diagnosis-based groups, including OA, developmental dysplasia of the hip, and other cases such as those with idiopathic necrosis of the femoral head, the OA group demonstrated the lowest value of mean stress at failure.16) A significant difference in the mean tensile stress at failure between genders was found: that of males was significantly greater than that of females. Inadequate osseous coverage of the femoral head in most dysplastic hips is located in the anterosuperior area of the hip joint. A negative correlation was found in dysplastic hips between the tensile stress at failure of the anterosuperior labrum and age, while the degeneration of the anterosuperior labrum was more severe than that of the posteroinferior labrum.17) We propose that degeneration of the fibers of the anterosuperior labrum due to OA may influence the stress and strain it can withstand.
Hydrostatic intracapsular pressure and inflammatory cytokines may play an important role in the pathophysiology of OA. Positive correlations between the intracapsular pressure and both the concentration of interleukin-1β (IL-1β) and the volume of the joint fluid were made as a result of our clinical study measuring the intracapsular pressure of the early dysplastic hips, and its relation to the concentration of IL-1β, the volume of the joint fluid, and the clinical and radiographic findings before CPO.18) These findings suggest that the inflammatory cytokines produced by the synovial membrane as a consequence of instability of the hip joint may be of importance for the initiation and/or development of OA in dysplastic hips. If inadequate osseous coverage of the femoral head is not treated in dysplastic hips, OA may be developed, caused mainly by abnormal stress and instability due to deterioration of the mechanical integrity of the joints. Inflammatory cytokines and mechanical weakness of tissues, due to aging and feminine gender, seem to accelerate the progression of OA (Fig. 1).
The patient is placed on a radiolucent table in the supine position. An anterior incision is made, beginning over the iliac crest at 2.5 cm posterior to the anterior superior iliac spine, and extending distally for approximately 9 cm along the tensor fasciae latae muscle (Fig. 2). The fascia over the tensor fasciae latae muscle belly is incised in line with the muscle fibers. The medial part of the incised fascia, along with the sartorius muscle, is reflected medially to protect the lateral femoral cutaneous nerve, and the tensor fascia latae muscle belly is reflected laterally. The anterior superior iliac spine is then osteotomized in a wedge-shaped fashion, with the inguinal ligament and sartorius muscle remaining attached (Fig. 3). The osteotomized anterior superior iliac spine, having the inner table of the pelvis as a base, is about 4 cm in length and 1.5 cm in width, and is retracted medially. No exposure of the outer table of the pelvis is needed in this operation. It is unnecessary to expose the neurovascular bundle that includes the femoral artery, vein, and nerve. The supra-acetabular portion of the iliacus muscle is then detached. The corpus of the pubis is exposed, and the blunt tip of a Chiari retractor is inserted into the posterior border of the quadrilateral space and fixed in the greater sciatic notch as a landmark. To create a working space for the osteotomy, a 3 cm wide retractor is inserted into the quadrilateral space and placed in front of the Chiari retractor (Fig. 4). Using a power drill, a C-shaped osteotomy line is started proximal to the anteroinferior iliac spine, ending in the distal part of the quadrilateral surface (Fig. 5). In order to keep the posterior column of the acetabulum intact and to avoid an intra-articular osteotomy, the most posterior part of the C-shaped osteotomy line in the quadrilateral surface should be about one-finger breadth anterior to the sciatic notch.19) The osteotomy line is also marked at a point just medial to the iliopubic eminence of the superior ramus of the pubis. After the osteotomy line is checked with an intraoperative fluoroscopy, the elevator is introduced into the space between the distal joint capsule and the psoas tendon with the hip in flexion and slight adduction. When the tip of the elevator contacts the ischium, the chisel is inserted along the elevator, and it is confirmed using intraoperative fluoroscopy that the direction of the blade is toward the infracotyloid groove. The chisel is hammered a few centimeters into the ischium. Osteotomy of the superior ramus of the pubis is carried out just medial to the iliopubic eminence and performed at an inclination of 30° to the horizontal line for medialization of the femoral head.20) The obturator artery and nerve pass through the obturator foramen under the bone. Retractors should be placed under the bone to protect the neurovascular structures. Osteotomy of the quadrilateral surface is carried out using a curved chisel. Lastly, osteotomy is carried out in the supra-acetabular portion of the ilium, into which the blade of the curved osteotome is hammered in a proximal-lateral direction. The C-shaped osteotomy enables smooth acetabular reorientation and medialization because the osteotomy surfaces have the same curvatures. The acetabular fragment is redirected and fixed temporarily with a Kirschner-wire. then the hip is flexed and rotated internally to verify that there is no excessive anterior or lateral correction that might lead to femoroacetabular impingement (FAI). To confirm a lack of FAI, the anterior part of the hip joint capsule is palpated when the hip is placed in flexion and internal rotation. If abutment of the anterior femoral head and neck on the anterior rim of the acetabulum is detected, the reoriented acetabular fragment is rotated posteriorly, or a resection osteochondroplasty of the nonspherical portion of the femoral head-neck junction is performed to relieve the impingement.21) Then, the acetabular fragment is fixed with two or three poly-L-lactic acid screws. The osteotomized anterior superior iliac spine is placed back in its original position and fixed with two titanium cannulated cancellous screws.
Active motion exercises are initiated on the first postoperative day. Partial weight-bearing (10 kg) on two crutches or a walker is allowed on the third postoperative day, and full weight-bearing is allowed after 8 weeks postoperation.
Good function of the abductor muscles in the hip is important to reduce dynamic instability of dysplastic hips while walking.22) The results of our previous study, examining the effects of subperiosteal dissection on blood flow in an animal model, suggested that the mid-portion of the gluteus medius muscle receives much of its blood from the ilium.23) Extensive dissection of the abductors from the outer aspect of the pelvis for the sake of iliac osteotomy may cause ischemic insult to the functional integrity of the muscle, and result in persistently poor postoperative abductor function.
Isokinetic muscle strengths of 24 hips in 22 patients were measured preoperatively, and again 6 and 12 months after CPO.24) At 12 months postoperatively, the mean muscle strength (percentage difference with the preoperative value) of the muscles was as follows: abductor, 42.2 Nm (129.6%); adductor, 39.4 Nm (131.4%); flexor, 48.4 Nm (121%); extensor, 45.8 Nm (130.5%). All of these values exceeded the preoperative values. These results seem to have been obtained thanks to the lack of dissection of the abductor muscles in CPO.
Acetabular retroversion can result from posterior wall deficiency in an otherwise normally oriented acetabulum, excessive anterior coverage secondary to a malpositioned acetabulum, or both, and is commonly associated with acetabular dysplasia. We retrospectively examined anteroposterior radiographs of the pelvis of 250 patients (342 hips) and found that the prevalence of acetabular retroversion was 18% in those with developmental dysplasia of the hip.25) The posterior wall coverage of dysplastic hips with acetabular retroversion tends to be lower than that of those with an anteverted acetabulum. Posterior OA of the hip developed postoperatively in 29% of the hips whose had a retroverted acetabulum preoperatively that had not reoriented after CPO.26) A marked decrease in free flexion was noted in patients with postoperative acetabular retroversion.27) Acetabular retroversion is a risk factor leading to degenerative OA of the hip. When a corrective osteotomy is performed in a patient with developmental dysplasia and a retroverted acetabulum, the surgeon should transfer the osteotomized acetabulum in a posterolateral direction while simultaneously moving the femoral head medially to prevent the development of OA in the posterior part of the hip due to posterior wall deficiency.
In a normal hip, the radiographic appearance of the subchondral plate in the superior aspect of the acetabulum or sourcil covers the contained femoral head, and is uniform and symmetrical. In a dysplastic hip, that of the sourcil covers only a small part of the subluxed femoral head, and becomes irregular and eccentric, showing an increased load distribution on the hip joint. The sourcil was found to be enlarged after reorientation of the acetabulum by osteotomy.28) We compared the enlargement of the sourcil after CPO in 19 patients aged 46 years or older with that in 47 patients aged less than 46 years, and found no significant differences between both groups.29) It seems that joint remodeling of the hip in patients over 46 years old is not inferior to that in younger patients (Fig. 6).
The presence of subchondral bone cysts reflects degeneration or defects of the articular cartilage, and elevated local stresses in the subchondral bone of dysplastic hips. To assess whether the presence of acetabular cysts negatively influences the effectiveness of CPO for the treatment of OA secondary to hip dysplasia, we reviewed the condition of 46 hips in 43 patients who underwent CPO. Of the 46 hips, 21 had acetabular cysts preoperation (cyst group) and 25 did not (control group).30) The clinical results were similar between the two groups. There were no differences in radiographic evaluations between the two groups, with a mean follow-up of more than 5 years each. In the cyst group, complete or partial healing of the cysts was observed in 17 of the 21 hips. A postoperative increase of 20° or more in the CE angle was found in 14 of these 17 hips. These results showed conclusively that the preoperative presence of acetabular cysts did not influence the results of periacetabular osteotomy. An adequate rotation of the acetabular fragment induced cyst remodeling.
Although periacetabular osteotomy has been established as an effective treatment for OA of dysplastic hips in younger patients to relieve hip pain and prevent early onset of secondary OA, the effectiveness of this osteotomy for older patients remains controversial. We evaluated 46 hips in 42 patients (older group) aged 50 years or older with developmental dysplasia of the hip that had undergone CPO, and compared the results of the operation those of 50 hips in 44 patients aged below 50 years (younger group) treated by the same osteotomy.31) The mean ages of older group and younger group were 54.6 years (range, 50 to 65 years) and 32.3 years (range, 19 to 49 years), respectively. There were no significant differences between the two groups preoperatively and postoperatively in their mean Harris hip scores, or in any of the radiographic measurements, including the CE angle, acetabular head index, acetabular roof obliquity, and head lateralization. Satisfactory results were obtained clinically and radiographically after CPO in patients aged 50 years or older. However, in patients with advanced OA, CPO should be performed with great care.
We investigated the results of CPO alone for the treatment of severe dysplastic hips (44 hips) of Severin32) group IV-b, compared to those for moderate dysplastic hips (147 hips) of Severin group III and IV-a.33) The mean postoperative acetabular roof obliquity and head lateralization index values did not differ significantly between the two groups. Good clinical results and low complication rates were obtained in both groups. This shows that using CPO alone for the treatment of severe dysplastic hips classified as subluxated hips of Severin group IV-b, with preoperative CE angles of up to -20°, could restore the acetabular coverage, weight-bearing area and medialization of the hip joint.
We often see residual deformities of the hip following the treatment for developmental dysplasia of the hip, or after Legg-Calvé-Perthes disease. These deformities characteristically include proximal femoral deformities, including the shortening of the femoral neck, the relative overgrowth of the greater trochanter, the flattened femoral head, and secondary acetabular dysplasia. These are so-called Perthes-like deformities. Surgical treatment for dysplastic hips with Perthes-like deformities in skeletally mature patients remains controversial. It is unclear whether we should treat both the deformed proximal femora and the dysplastic acetabulum, or treat them respectively. We retrospectively evaluated 17 hips in 16 patients who underwent CPO for the treatment of dysplastic hips with Perthes-like deformities.34) The average age of patients at surgery was 36.9 years, and the average follow-up was 6.6 years. The average Harris hip score significantly improved from 68.2 points preoperatively to 91.1 points postoperatively. The average lateral center edge angle improved significantly from -0.3° preoperatively to 30.4° postoperatively. Clohisy et al.35) previously reported the clinical results of periacetabular osteotomy for the treatment of Perthes-like deformities in 24 hips in 20 patients. A proximal femoral valgus-producing osteotomy was simultaneously performed in 13 of the 24 hips. The average Harris hip score in those patients was generally equal to that of the patients in our study preoperatively and at follow-up; however, they described that 6 of the 24 hips had additional surgical procedures or major complications. CPO, without any other combined procedure, produced good mid-term clinical and radiographic results in pateints with Perthes-like deformities (Fig. 7). None of our patients had additional surgical procedures or major complications.
Paliobeis and Villar36) reported that 47% of patients with FAI also had radiographic evidence of dysplasia. Clohisy et al.37) reported the analysis of the femoral head-neck junction in symptomatic acetabular dysplasia, revealing that 73.1% of dysplastic hips had an abnormal head-neck ratio or alpha angle, and 72% were judged to have an aspheric femoral head. Recently, Nassif et al.38) reported the results of femoral head-neck junction osteochondroplasy performed concurrently with a periacetabular osteotomy for the treatment of symptomatic acetabular dysplasia associated with femoral head-neck junction deformities. They described that this combined procedure provided effective correction of associated femoral head-neck junction deformities, and produced similar early functional outcomes when compared with isolated periacetabular osteotomy. We have also been performing CPO in conjunction with osteochondroplasty for the treatment of acatabular dysplasia associated with FAI since 2006.21,39) Although it usually takes about 15 minutes longer than an isolated periacetabular osteotomy, the combined procedure has been providing effective correction of both acetabular dysplasia and associated femoral head-neck deformities without any increase in the complication rate (Fig. 8).
Arterial injuries are rare, but potentially devastating complications of periacetabular osteotomy. They will cause lethal bleeding if untreated promptly, and may only be seldom reported due to litigation. When performing a rotational acetabular osteotomy,12) the osteotomy is done from the lateral surface of the pelvis with the patient in a lateral position. Osteotomies and fixation are made from the outward pelvis going inward. If excessive drilling is done for fixation of the transferred acetabulum, there is potential danger to the external iliac artery. We found in Japanese patients that the external artery was located closer and more ventral to the anterior inferior iliac spine in right hemipelves than in left hemipelves, and that the average distance from the outer surface of the iliac osteotomy site to the external iliac artery was significantly shorter in females (average, 31.7 mm) than in males (average, 38.2 mm).40) On the basis of these findings, a rotational acetabular osteotomy on a right pelvis, especially in females, seems to be potentially more dangerous with regard to the risk of vascular injury to the external iliac artery than that on the left side. On the other hand, the external iliac artery in the Bernese periacetabular osteotomy or CPO is completely safe, because iliac osteotomies are made from the inward pelvis going outward with a modified Smith-Petersen approach. However, in any type of reorientation osteotomy of the acetabulum, there is a potential risk of intraoperative injury to the obturator artery,41,42) which is located in close proximity to the pubic osteotomy site. We examined 32 cadaver hemipelves and analyzed the anatomical relationship between the obturator artery and the pubic osteotomy site during periacetabular osteotomy in detail.43) The results indicated that the obturator artery is located closest to the distal part of the pubic osteotomy line around the base of the pubis, and that a chisel should be inserted into the pubis at a distance greater than 6 mm form the medial base of the iliopubic ramus. We have encountered injuries to this artery in only one out of more than 700 cases. In this case, pubic osteotomy was done just at the medial base of the iliopubic ramus, and trans-arterial embolization was immediately performed after CPO without any ensuing sequelae. We also examined 29 cadaver hemipelves to analyze the anatomical relationship between the obturator artery and the ischial osteotomy site during periacetabular osteotomy in detail, and found that this procedure can be performed safely via the anterior approach if a chisel with a blade of 20 mm or shorter is used.44)
There have been only two intraoperative comminuted fractures in our series so far. One comminuted fracture of the acetabulum occurred during an iliac osteotomy in a 46-year-old woman in January 1998 (Fig. 9). The other occurred at the posterior column during an osteotomy of the quadrilateral space in a 31-year-old woman in April 1998. In both patients, bed rest with skin traction was maintained for 3 weeks after surgery, and touch-down weight bearing on crutches was then begun. Full weight-bearing was not allowed until 10 weeks postoperatively. Bony union and pain relief were observed in both patients. In both of these cases, the intraoperative fractures were caused by inadvertent use of the chisel. Since then, as osteotomies have been performed by going deep gradually with careful use of the chisel, there have been no further intraoperative fractures with this procedure.
The skin incision of a Smith-Petersen approach has a strong possibility to cross over the lateral femoral cutaneous nerve.45) Since 2006, we have modified the surgical exposure to decrease the possibility of causing lateral femoral cutaneous nerve injuries.33) The skin incision in this modified surgical exposure, which is a few centimeters lateral to the original surgical exposure, is made along the tensor fasciae latae. The membrane of the tensor fasciae latae is incised along itself, and part of the muscle is retracted laterally. Then, the lateral femoral cutaneous nerve, with its surrounding tissues, is retracted medially without exposure of the lateral femoral cutaneous nerve. Thanks to this modification of the surgical exposure, dysesthesia of the lateral femoral cutaneous nerve has been dramatically decreased.
Although it was assumed that a superior limb of the pubis nonunion would occur mainly in severe dysplastic hips, likely as a result of a large transfer of the acetabular fragment, this complication also occurred in moderate dysplastic hips. Though it is difficult to reach a clear conclusion as to the cause of this complication because of the small number of cases, it may be attributable to overcorrection or lateralization, producing a large gap in the osteotomy site of the pubis. Most of the patients with pubic nonunion were asymptomatic (Fig. 10); however, careful follow-up is required because stress fractures are believed to arise when the load transmission only occurs through the inferior limb of the pubis and ischium.46)
References
1. Aronson J. Osteoarthritis of the young adult hip: etiology and treatment. Instr Course Lect. 1986; 35:119–128. PMID: 3819398.
2. Nakamura S, Ninomiya S, Nakamura T. Primary osteoarthritis of the hip joint in Japan. Clin Orthop Relat Res. 1989; (241):190–196. PMID: 2924462.

3. Takeyama A, Naito M, Shiramizu K, Kiyama T. Prevalence of femoroacetabular impingement in Asian patients with osteoarthritis of the hip. Int Orthop. 2009; 33(5):1229–1232. PMID: 19277653.

4. Dorr LD, Kane TJ 3rd, Conaty JP. Long-term results of cemented total hip arthroplasty in patients 45 years old or younger: a 16-year follow-up study. J Arthroplasty. 1994; 9(5):453–456. PMID: 7807101.
5. Duffy GP, Berry DJ, Rowland C, Cabanela ME. Primary uncemented total hip arthroplasty in patients <40 years old: 10- to 14-year results using first-generation proximally porous-coated implants. J Arthroplasty. 2001; 16(8 Suppl 1):140–144. PMID: 11742466.
6. Burston BJ, Yates PJ, Hook S, Moulder E, Whitley E, Bannister GC. Cemented polished tapered stems in patients less than 50 years of age: a minimum 10-year follow-up. J Arthroplasty. 2010; 25(5):692–699. PMID: 19577886.

7. Kim YH, Kim JS, Park JW, Joo JH. Comparison of total hip replacement with and without cement in patients younger than 50 years of age: the results at 18 years. J Bone Joint Surg Br. 2011; 93(4):449–455. PMID: 21464481.
8. Sharifi E, Sharifi H, Morshed S, Bozic K, Diab M. Cost-effectiveness analysis of periacetabular osteotomy. J Bone Joint Surg Am. 2008; 90(7):1447–1456. PMID: 18594092.

9. Ganz R, Klaue K, Vinh TS, Mast JW. A new periacetabular osteotomy for the treatment of hip dysplasias: technique and preliminary results. Clin Orthop Relat Res. 1988; (232):26–36. PMID: 3383491.

10. Millis MB, Murphy SB, Poss R. Osteotomies about the hip for the prevention and treatment of osteoarthrosis. Instr Course Lect. 1996; 45:209–226. PMID: 8727740.

11. Naito M, Shiramizu K, Akiyoshi Y, Ezoe M, Nakamura Y. Curved periacetabular osteotomy for treatment of dysplastic hip. Clin Orthop Relat Res. 2005; (433):129–135. PMID: 15805948.

12. Ninomiya S, Tagawa H. Rotational acetabular osteotomy for the dysplastic hip. J Bone Joint Surg Am. 1984; 66(3):430–436. PMID: 6699061.

13. Maeyama A, Naito M, Moriyama S, Yoshimura I. Evaluation of dynamic instability of the dysplastic hip with use of triaxial accelerometry. J Bone Joint Surg Am. 2008; 90(1):85–92. PMID: 18171961.

14. Maeyama A, Naito M, Moriyama S, Yoshimura I. Periacetabular osteotomy reduces the dynamic instability of dysplastic hips. J Bone Joint Surg Br. 2009; 91(11):1438–1442. PMID: 19880886.

15. Klaue K, Durnin CW, Ganz R. The acetabular rim syndrome: a clinical presentation of dysplasia of the hip. J Bone Joint Surg Br. 1991; 73(3):423–429. PMID: 1670443.

16. Ishiko T, Naito M, Moriyama S. Tensile properties of the human acetabular labrum-the first report. J Orthop Res. 2005; 23(6):1448–1453. PMID: 16099616.

17. Kumano T, Naito M, Ishiko T, Moriyama S, Tanaka J. Regional difference of tensile properties of the human acetabular labrum in various hip disorders. Curr Orthop Pract. 2008; 19(5):564–569.

18. Xie J, Naito M, Maeyama A. Intracapsular pressure and interleukin-1beta cytokine in hips with acetabular dysplasia. Acta Orthop. 2010; 81(2):189–192. PMID: 20367415.
19. Shiramizu K, Naito M, Asayama I, Yatsunami M. A quantitative anatomic characterization of the quadrilateral surface for periacetabular osteotomy. Clin Orthop Relat Res. 2004; (418):157–161. PMID: 15043108.

20. Teratani T, Naito M, Shiramizu K, Nakamura Y, Moriyama S. Modified pubic osteotomy for medialization of the femoral head in periacetabular osteotomy: a retrospective study of 144 hips. Acta Orthop. 2008; 79(4):474–482. PMID: 18766479.

21. Teratani T, Naito M, Kiyama T, Maeyama A. Periacetabular osteotomy in patients fifty years of age or older: surgical technique. J Bone Joint Surg Am. 2011; 93(Suppl 1):30–39. PMID: 21411684.
22. Kuroda D, Maeyama A, Naito M, et al. Dynamic hip stability, strength and pain before and after hip abductor strengthening exercises for patients with dysplastic hips. Isokinet Exerc Sci. 2013; 21(2):95–100.

23. Akiyoshi Y, Naito M, Takagishi H, Imai K, Ogata K. Blood flow of the gluteus medius muscle: an animal study. Int Orthop. 1999; 23(4):202–204. PMID: 10591934.
24. Ezoe M, Naito M, Asayama I. Muscle strength improves after abductor-sparing periacetabular osteotomy. Clin Orthop Relat Res. 2006; 444:161–168. PMID: 16449917.

25. Ezoe M, Naito M, Inoue T. The prevalence of acetabular retroversion among various disorders of the hip. J Bone Joint Surg Am. 2006; 88(2):372–379. PMID: 16452750.

26. Kiyama T, Naito M, Shiramizu K, Shinoda T. Postoperative acetabular retroversion causes posterior osteoarthritis of the hip. Int Orthop. 2009; 33(3):625–631. PMID: 18157533.

27. Xie J, Naito M, Maeyama A. Evaluation of acetabular versions after a curved periacetabular osteotomy for dysplastic hips. Int Orthop. 2010; 34(4):473–477. PMID: 19424696.

28. Ida T, Naito M, Nakamura Y, et al. Improved joint congruency induces joint remodeling after curved periacetabular osteotomy. Hip Joint. 2011; 37:832–835.
29. Kinoshita K, Naito M, Nakamura Y, et al. The comparison of old patients after periacetabular osteotomy and younger about joint remodeling. In : AAOS 2011 Annual Meeting; 2011 Feb 16-19; San Diego, CA.
30. Nakamura Y, Naito M, Akiyoshi Y, Shitama T. Acetabular cysts heal after successful periacetabular osteotomy. Clin Orthop Relat Res. 2007; 454:120–126. PMID: 16906117.

31. Teratani T, Naito M, Kiyama T, Maeyama A. Periacetabular osteotomy in patients fifty years of age or older. J Bone Joint Surg Am. 2010; 92(1):31–41. PMID: 20048093.

32. Severin EA. Contribution to the knowledge of congenital dislocation of the hip joint: late results of closed reduction and arthrographic studies of recent cases. Acta Chir Scand. 1941; 84(Suppl 63):1–142.
33. Karashima H, Naito M, Shiramizu K, Kiyama T, Maeyama A. A periacetabular osteotomy for the treatment of severe dysplastic hips. Clin Orthop Relat Res. 2011; 469(5):1436–1441. PMID: 20936385.

34. Shinoda T, Naito M, Nakamura Y, Kiyama T. Periacetabular osteotomy for the treatment of dysplastic hip with Perthes-like deformities. Int Orthop. 2009; 33(1):71–75. PMID: 17999061.

35. Clohisy JC, Nunley RM, Curry MC, Schoenecker PL. Periacetabular osteotomy for the treatment of acetabular dysplasia associated with major aspherical femoral head deformities. J Bone Joint Surg Am. 2007; 89(7):1417–1423. PMID: 17606777.

36. Paliobeis CP, Villar RN. The prevalence of dysplasia in femoroacetabular impingement. Hip Int. 2011; 21(2):141–145. PMID: 21484736.

37. Clohisy JC, Nunley RM, Carlisle JC, Schoenecker PL. Incidence and characteristics of femoral deformities in the dysplastic hip. Clin Orthop Relat Res. 2009; 467(1):128–134. PMID: 19034600.

38. Nassif NA, Schoenecker PL, Thorsness R, Clohisy JC. Periacetabular osteotomy and combined femoral head-neck junction osteochondroplasty: a minimum two-year follow-up cohort study. J Bone Joint Surg Am. 2012; 94(21):1959–1966. PMID: 23138238.
39. Nakamura Y, Ida T, Naito M. Clinical results of curved periacetabular osteotomy with osteochondroplasty for acetabular dysplasia with FAI. In : The 86th Annual Meeting of the Japanese Orthopaedic Association; 2013 May 23-26; Hiroshima, Japan.
40. Kambe T, Naito M, Asayama I, et al. Vascular anatomy for rotational acetabular osteotomy: cadaveric study. J Orthop Sci. 2003; 8(3):323–328. PMID: 12768473.

41. Brenoe AS, Andersen PE, Overgaard S. Endovascular embolisation of severe bleeding in connection with periacetabular osteotomy. Ugeskr Laeger. 2006; 168(14):1453–1454. PMID: 16584678.
42. Nishibe N, Tanabe T, Tagawa A, Ninomiya S. A case report of intra pelvic arterial injury in the rotational acetabular osteotomy. Hip Joint. 2008; 28:165–167.
43. Kinoshita K, Naito M, Shiramizu K, Kamada S. Prevention of obturator artery injury during pubic osteotomy in periacetabular osteotomy. Curr Orthop Pract. 2011; 22(2):171–175.

44. Kamada S, Naito M, Shiramizu K, Nakamura Y, Kinoshita K. Is the obturator artery safe when performing ischial osteotomy during periacetabular osteotomy? Int Orthop. 2011; 35(4):503–506. PMID: 20556381.

45. Kiyama T, Naito M, Shiramizu K, Shinoda T, Maeyama A. Ischemia of the lateral femoral cutaneous nerve during periacetabular osteotomy using Smith-Petersen approach. J Orthop Traumatol. 2009; 10(3):123–126. PMID: 19551340.

46. Espinosa N, Strassberg J, Belzile EL, Millis MB, Kim YJ. Extraarticular fractures after periacetabular osteotomy. Clin Orthop Relat Res. 2008; 466(7):1645–1651. PMID: 18465184.

47. Siebenrock KA, Schöll E, Lottenbach M, Ganz R. Bernese periacetabular osteotomy. Clin Orthop Relat Res. 1999; (363):9–20. PMID: 10379300.

48. Davey JP, Santore RF. Complications of periacetabular osteotomy. Clin Orthop Relat Res. 1999; 363:33–37. PMID: 10379302.

Fig. 1
Radiographs of a 56-year-old female patient with moderate dysplasia of the right hip. (A) Radiograph at presentation showing moderate hip dysplasia with early stage osteoarthritis (OA). (B) Radiograph at 20 months after presentation showing end-stage OA.
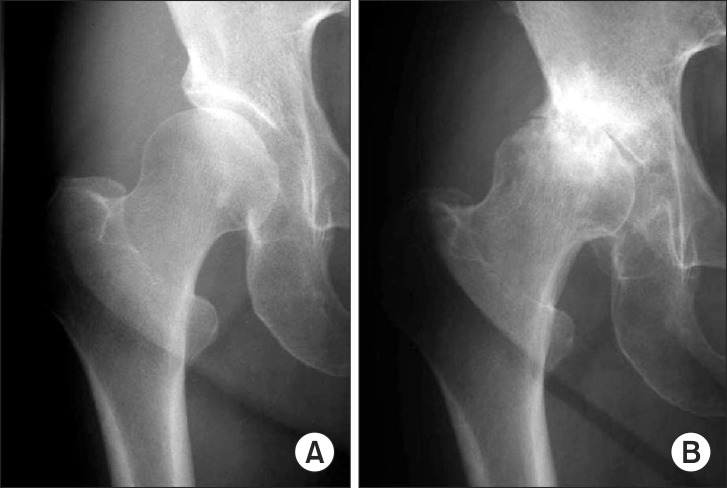
Fig. 2
Schematic drawing of the skin incision. The skin is incised a few centimeters lateral to the course of the lateral femoral cutaneous nerve. ASIS: anterior superior iliac spine.
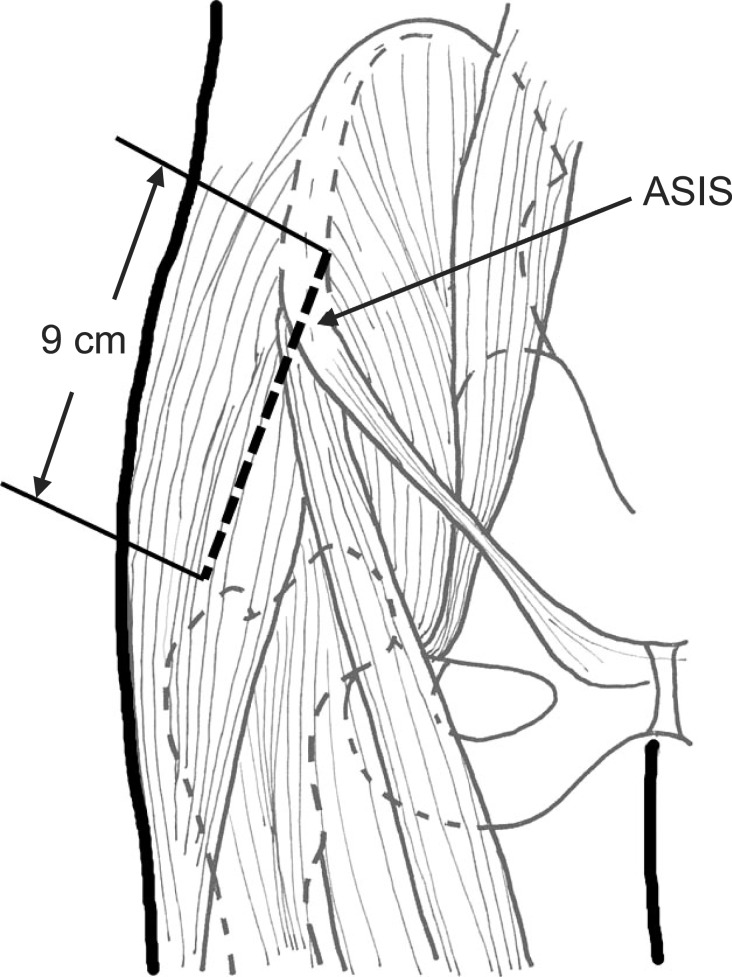
Fig. 3
Schematic drawing of the osteotomy of the anterior superior iliac spine. The anterior superior iliac spine is osteotomized in a wedge-shaped fashion, with the inguinal ligament and sartorius muscle remaining attached in order to prevent the outer table of the pelvis from dissecting. TFLM: tensor fasciae latae muscle, ASIS: anterior superior iliac spine, IL: ilioinguinal ligament, SM: sartorius muscle.
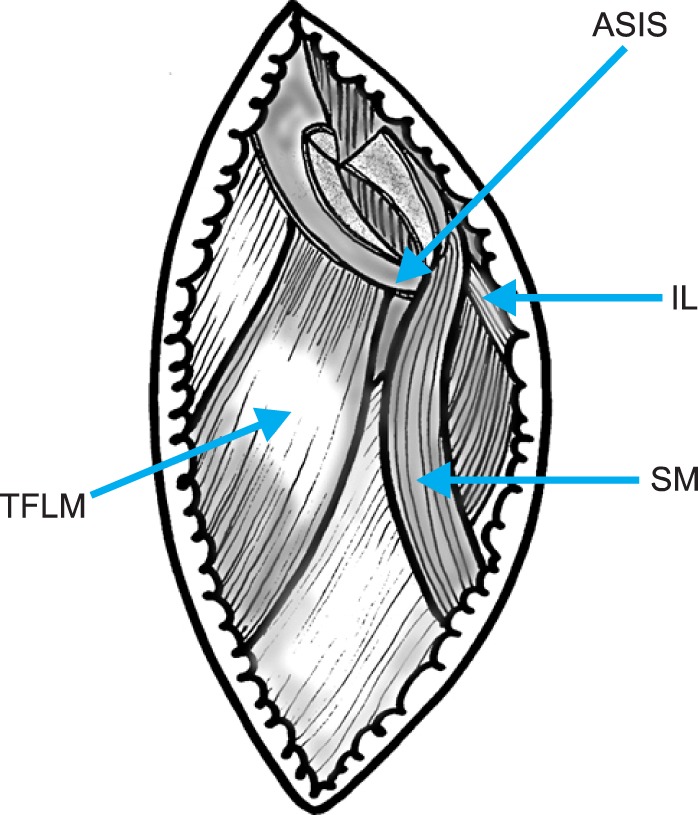
Fig. 4
Photograph of creation of a working space in the quadrilateral space. The blunt tip of a Chiari retractor is fixed in the greater sciatic notch as a landmark. A 3 cm wide retractor is placed in front of the Chiari retractor.
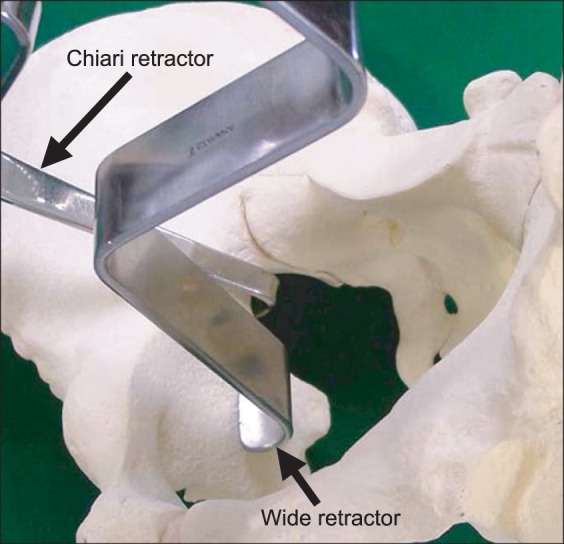
Fig. 5
Photograph of C-shaped osteotomy line of curved periacetabular osteotomy. Using a power drill, a C-shaped osteotomy line is started proximal to the anteroinfer

Fig. 6
A 50-year-old woman who underwent curved periacetabular osteotomy (CPO) on her right hip. (A) Preoperative radiograph showing advanced osteoarthritis in her right hip. (B) Preoperative false-profile radiograph showing subluxation of the femoral head in her right hip. (C) Postoperative radiograph at 16 years (age 66), showing improvement of the femoral head coverage in her right hip. The Harris hip score of her right hip improved from 46 points preoperatively to 92 points at 16 years after CPO. (D) Sixteen-year postoperative (age 66) false-profile radiograph showing reduction of the femoral head and good congruity in her right hip. The sourcil of her right hip is markedly enlarged, compared to that before CPO (B).
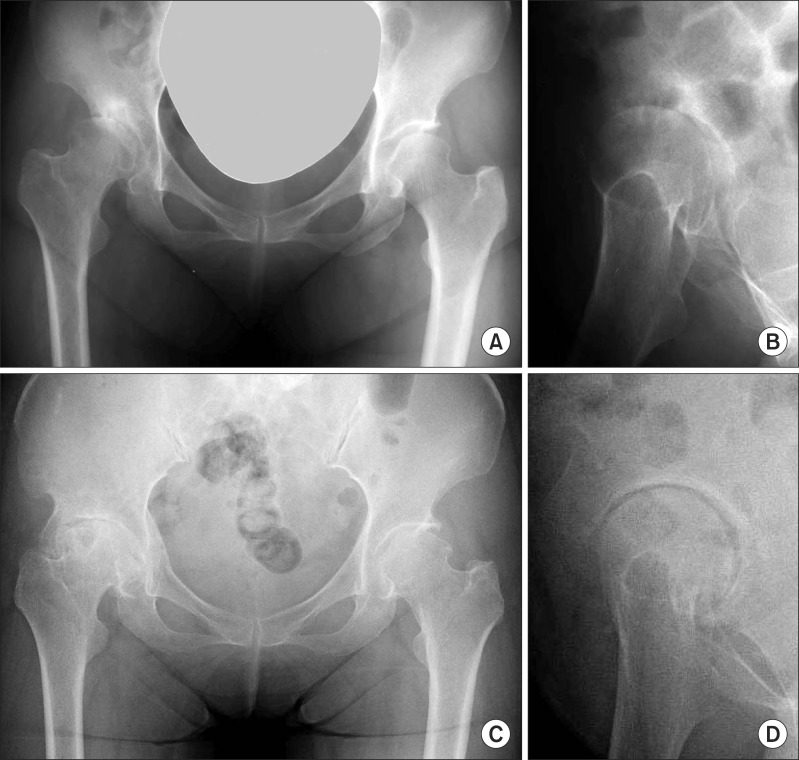
Fig. 7
A 35-year-old man who underwent curved periacetabular osteotomy for the treatment of a dysplastic hip with Perthes-like deformities. (A) Preoperative radiograph showing so-called Perthes-like deformities and retroversion of the acetabulum in his right hip. (B) Five-year postoperative radiograph showing improvement of the femoral head coverage and anteversion of the acetabulum in his right hip. The Harris hip score of his right hip improved from 57 points preoperatively to 98 points postoperatively.
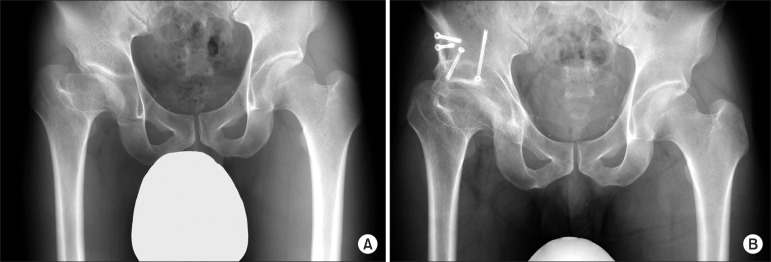
Fig. 8
A 43-year-old woman who underwent curved periacetabular osteotomy in conjunction with osteochondroplasty on both hips. (A) Preoperative radiograph showing moderate acetabular dysplasia in both hips. (B) Preoperative cross-table radiograph showing a slightly prominent head-neck junction of her right hip. (C) Preoperative cross-table radiograph showing a slightly prominent head-neck junction of her left hip. (D) Radiograph made 2 years postsurgery on her left hip (1 year postsurgery on her right hip) showing improvement of the femoral head coverage in both hips. Signs of impingement also disappeared in both hips. (E) Postoperative cross-table radiograph showing recontouring of the femoral head-neck junction of her right hip. The Harris hip score improved from 83 points preoperatively to 94 points at 1 year postsurgery. (F) Postoperative cross-table radiograph showing recontouring of the femoral head-neck junction of her left hip. The Harris hip score improved from 73 points preoperatively to 96 points at 2 years postsurgery.
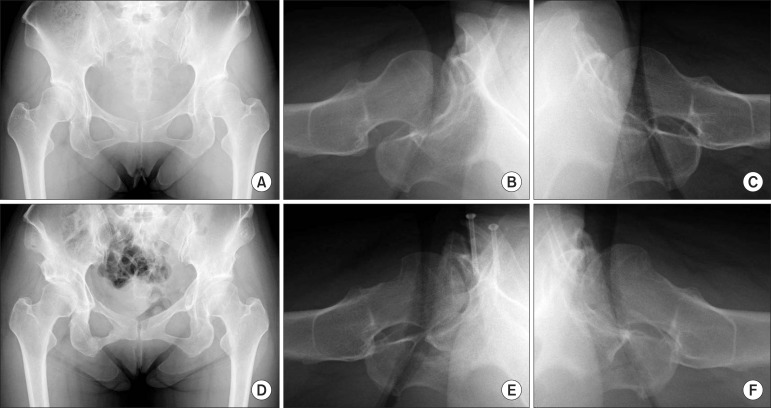
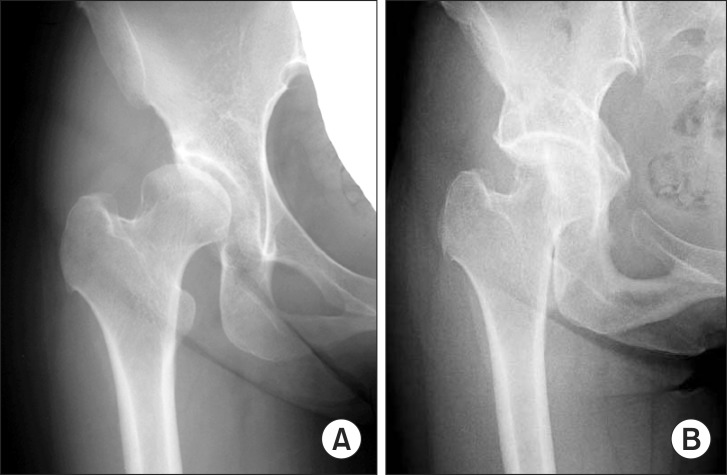
Fig. 9
A 46-year-old woman who had an intraoperative comminuted fracture of the acetabulum during the iliac osteotomy. (A) Preoperative radiograph showing acetabular dysplasia with advanced osteoarthritis in her left hip. (B) Immediate postoperative radiograph showing the comminuted fracture of the osteotomized acetabulum. (C) Radiograph made 6 years postsurgery showing the increased joint space of her left hip. The Harris hip score improved from 61 points preoperatively to 86 points at 6 years postsurgery.

Fig. 10
A 40-year-old-woman who had pubic nonunion after curved periacetabular osteotomy. (A) Preoperative radiograph showing moderate acetabular dysplasia with early stage osteoarthritis in her right hip. (B) Radiograph made 12 years postsurgery showing the pubic nonunion in her right hip. The Harris hip score improved from 96 points preoperatively to 100 points postoperatively.




 PDF
PDF ePub
ePub Citation
Citation Print
Print


 XML Download
XML Download