Abstract
Background
The purpose of this study was to investigate the frequency and distribution of associated carpal bone fractures (CBFs) in distal radial fractures (DRFs).
Methods
Three hundred and thirteen patients who underwent surgical treatment for DRFs between March 2007 and January 2010 were reviewed retrospectively. In this study, 223 patients who had preoperative computed tomography (CT) were included. We investigated the frequency and distribution of associated CBFs on CT scans. The relationship between the frequency of associated CBFs and patient factors such as age, gender, body mass index, and the mechanism of injury was assessed.
Results
CBFs were complicated in 46 of 223 DRFs (20.9%). The distribution of CBFs was 23 cases in the triquetrum, 16 in the lunate, 12 in the scaphoid, five in the hamate, and four in the pisiform. Among the 46 cases, a fracture of one carpal bone occurred in 36 cases, two in seven cases, three in two cases, and four in one case. In 10 of the 46 cases, associated CBFs occurred in more than two carpal bones. No significant differences were observed for age, sex, body mass index, or the mechanism of injury between patients with DRFs and CBFs and those without CBFs.
The wrist is a complex joint consisting of bony structures, including the distal radius, distal ulna, and eight carpal bones and a ligament complex that divides extrinsic and intrinsic ligaments. Therefore, the prognosis of wrist injuries can be affected by soft tissue injuries as well as fractures.1-4) Distal radial fractures (DRFs) are common injuries that occur in the upper limb and are treated using various methods, including closed reduction and cast immobilization, percutaneous K-wire fixation, external fixation, intramedullary fixation, and open reduction and internal fixation. Various clinical results and complication rates have been reported.4,5) However, previous studies have been mostly limited to fractures that occur in the distal radius with associated fractures in the distal ulna. Based on the development of arthroscopic instruments and techniques, DRFs associated with soft tissue injuries such as the triangular fibrocartilage complex, scapholunate ligament, and lunotriquetral ligament have been reported. Some studies have reported that associated soft tissue injuries may affect the outcome of DRFs.1-4)
As soft tissue injuries may be accompanied by DRFs, carpal bone fractures (CBFs) may occur in association with DRFs. Avulsion fractures of carpal bones are commonly observed in patients with DRFs and may indicate injuries to the intrinsic or extrinsic ligaments of the wrist. Additionally, CBFs may be untreated, because CBFs are frequently missed on initial radiographs, which may lead to persistent pain or subsequent wrist dysfunction and eventually affect the outcome of DRF treatment. If associated CBFs are misdiagnosed and left untreated, unsatisfactory DRF clinical outcomes may occur. Therefore, associated carpal injuries must be ruled out for DRFs.6) However, the frequency and distribution of CBFs associated with DRFs have not been reported, since cases of scaphoid fractures accompanying DRFs are usually reported. The purpose of this study was to investigate the frequency and distribution of CBFs associated with DRFs.
A total of 313 patients who underwent operative treatment after being diagnosed with a DRF by plain X-ray between March 2007 and January 2010 were reviewed retrospectively. In this study, 223 patients who underwent preoperative computed tomography (CT) were included. DRFs that had a fracture-dislocation associated with a CBF or suspected intercarpal instability on plain X-ray were excluded.
There were 82 males and 141 females with a mean age of 57.6 years (range, 16 to 97 years). The mechanism of injury included fall on an outstretched hand (143 cases), fall from height (38 cases), and traffic accident (42 cases). All DRFs underwent anteroposterior, lateral, and oblique plain X-ray views of the wrist prior to and after reduction. CT scans were performed in neutral forearm rotation after wearing a sugar tongs splint. The CT machine was an Mx8000-IDT instrument (Philips, Eindhoven, The Netherlands). A 1 mm interval sectioned image was obtained and reconstructed into sagittal, axial, and coronal images using the MxView ver. 3.5 program (Moxa, Brea, CA, USA).
All DRFs were investigated for the frequency and location of associated CBFs on CT scans. The DRFs were classified by the arbeitsgemeinschaft für osteosyntheses (AO) classification,7) and the frequency of associated CBFs was checked for each AO classification. The DRFs were divided into two groups: DRFs with CBFs and those without CBFs. Differences in age, sex, and body mass index between the two groups were compared with the chi-square test. The mechanism of injury was divided into a low-energy group including fall on an outstretched hand and a high-energy group including fall from height and traffic accident. The frequency of associated CBFs between the two groups was compared with the t-test. The frequency among AO types was compared with Fisher's exact test.
Among 223 DRFs, 46 were accompanied by CBFs. There were 20 males and 26 females with a mean age of 57.3 years (range, 16 to 87 years). The mechanisms of injury included fall on an outstretched hand (30 cases), fall from height (11 cases), and traffic accident (five cases) (Table 1). The distribution of CBFs was 23 cases in the triquetrum, 16 in the lunate, 12 in the scaphoid, five in the hamate, and four in the pisiform (Fig. 1). Among the 46 DRFs with CBFs, fractures of the triquetrum were the most commonly identified, and most CBFs were identified in the proximal carpal row. Also, among the 46 DRFs with CBFs, cases with associated fractures of one carpal bone (Fig. 2) occurred in 36 case, two in seven cases (Fig. 3), three in two cases (Fig. 4), and four in one case (Fig. 5). Ten of the 46 cases were accompanied by CBFs in more than two carpal bones.
All DRFs were classified by the AO classification, and the frequency of associated CBFs was checked for each AO classification (Table 2). Type A3 was complicated in two of 44 cases, type B1 was complicated in two of 11, type B3 was one of 12, type C1 was one of 13, type C2 was 19 of 75, and type C3 was 21 of 66.
No significant differences were observed for age (p = 0.38), sex (p = 0.30), or body mass index (p = 0.28) between patients with DRFs and CBFs (46 cases) and those without CBFs (177 cases). No significant difference was observed in the frequency of associated CBFs between the low-energy and high-energy groups separated by the mechanism of injury (p = 0.86). Despite the relatively high frequency of associated CBFs in AO types C3 or C2, no difference was found among AO types (p = 0.18).
The eight carpal bones composing the wrist joint are of various sizes and shapes, and stability among carpal bones is maintained by extrinsic and intrinsic ligaments. Due to this complex anatomical structure, the diagnosis of CBFs using plain radiographs is difficult. Misdiagnosed or untreated CBFs can lead to complications including nonunion, malunion, avascular necrosis, carpal instability, articular incongruity, or traumatic arthritis and can consequently induce persistent pain and result in functional compromise.8-10) In this study, we confirmed associated CBFs in 20.6% of DRFs that had been surgically treated. However, plain radiographs were insufficient to make a diagnosis, thus most cases were confirmed by CT. Welling et al.10) suggested that CT should be considered if clinically warranted, because 30% of wrist fractures are not detected on plain radiographs. In addition, as other CBFs, except those of the scaphoid, are more difficult and have lower sensitivity for detection on plain radiographs, the need for specific radiographic views or CT is emphasized. Kiuru et al.11) also recommended the need for CT to assess complex wrist fractures or when initial radiographs are equivocal, because only plain radiographs may miss occult fractures, which usually occur in small carpal bones. In this study, only 14 of 46 DRFs associated with CBFs were detected on plain radiographs and all the others were found on CT scans.
The frequency of CBFs of all hand injuries ranges from 8% to 19%.8,9,12,13) The scaphoid accounts for about 70% of all CBFs, and the remaining carpal bones account for about 30%. More than 90% of CBFs are found in the proximal carpal row. In our study, 89% of CBFs associated with DRFs occurred in the proximal carpal row. However, the frequency of fractures of the triquetrum and lunate was higher than that of the scaphoid, and only the hamate was injured in the distal carpal row. Accordingly, the frequency and distribution of CBFs associated with DRFs were different from those of ordinary CBF cases.
DRF is one of the most common fractures in the upper extremities which results from a fall on an outstretched hand with an extended wrist. Because the mechanism of carpal bone injuries is similar to that of DRFs, CBFs may often occur simultaneously with DRFs. The complication rates of DRFs in previous studies vary from 6% to 80%.4) The clinical result of DRFs may be influenced by injury severity, any associated soft-tissue trauma, and treatment method. In accordance with the development of arthroscopic procedures for the wrist joint, associated damage to soft tissues such as the triangular fibrocartilage complex or intercarpal ligaments has been reported, and the importance of treating this accompanying damage has been emphasized.1-3) However, the prevalence and effect on clinical results of CBFs associated with DRFs have not been reported. Most reports regarding simultaneous CBFs and DRFs are scaphoid fractures, which account for 0.75%-6.5% of all DRFs. Stable internal fixation of scaphoid fractures and DRFs is generally performed for early mobilization of the wrist joint and to avoid complications such as scaphoid nonunion.14,15) Pretell-Mazzini and Carrigan6) reported simultaneous DRFs and carpal bone injuries in children. They emphasized that orthopedic surgeons must first rule out CBFs because the mechanism of injury is similar for both fractures, and inappropriate treatment may lead to unsatisfactory outcome. Most other CBFs, except scaphoid fractures, can be treated by immobilizing the patient for 4-6 weeks. In our study, all CBFs except five waist fractures of the scaphoid were conservatively managed. In accordance with the development of a locking plate for DRFs, however, early mobilization of the wrist joint is often performed after the operation for the DRF.16,17) If a CBF is not found on the initial plain radiograph and early exercise is performed after stable internal fixation of the DRF, the undetected CBFs may affect the patient's rehabilitation and treatment outcome. We generally immobilize all DRFs for about 4 weeks after surgery using a locking plate. In a comparison study between an early motion group and a late motion group by Lozano-Calderon et al.,18) no significant differences in range of motion, grip power, or clinical scoring were observed. Therefore, we believe that immobilization for an appropriate period after surgery is necessary if associated CBFs are detected or uncertain on the initial plain radiograph. Orthopedic surgeons must carefully access associated CBFs on the initial radiography or CT, which are observed as avulsion fractures and may imply ligament damage or instability of the wrist joint.4,19-21)
The strength of the present study was that it investigated the frequency and distribution of CBFs associated with DRFs, which have not been reported previously. However, several limitations should be noted. First, there was a possibility of selecting more severe fractures, because surgically treated DRFs were included and those without CT were excluded. Accordingly, the frequency of CBFs may be higher than observed due to selection bias. DRFs that are conservatively treated should be included in the materials of the study to overcome this bias. However, it should be noted that diagnosing CBFs on plain radiographs is difficult. Second, DRFs with associated CBFs were surgically treated with various methods such as volar plate fixation (29 DRFs), dorsal plate fixation (five DRFs), external fixation (seven DRFs), and percutaneous K-wire fixation (five DRFs). Because these fractures were not treated by one surgical method with the same postoperative protocol, they did not have a significance to evaluate the clinical outcomes. Third, radiological parameters of the distal radius were not evaluated, as the main purpose of this study was to investigate CBFs complicated by DRFs. Forth, we did not compare clinical outcomes between patients with DRFs and CBFs and those without CBFs. A further study is required to evaluate whether associated CBFs in DRFs affect the clinical outcome of DRFs.
In conclusion, DRFs were accompanied by CBFs at a considerably high frequency, and most of the fractures were combined in the proximal carpal row. The frequency of CBFs increased in severe fracture types such as AO types C2 and C3, and 90% of the DRFs with associated CBFs were classified as these two types. If DRFs with associated CBFs are conservatively treated, no additional attention to the CBF, except the scaphoid, may be required. In contrast, if a DRF is surgically treated and early mobilization is planned, misdiagnosed or untreated associated CBFs may affect the final outcome. Therefore, confirmation of a CBF accompanied by a DRF is required along with use of CT scan for the detection of CBFs complicated by DRFs that require operative management, as plain radiographs are insufficient for a definitive diagnosis of associated CBFs.
Figures and Tables
Fig. 1
The distribution of carpal bone fractures that occurred simultaneously with distal radial fractures.

Fig. 2
Initial radiographs (A and B) show a distal radial fracture (AO type C2) and an ulnar styloid fracture. Reconstructed computed tomography images (C and D) show a palmar pole fracture of the lunate. AO: arbeitsgemeinschaft für osteosyntheses.

Fig. 3
Initial radiographs (A and B) show a radial fracture (AO type C3) and an ulnar styloid fracture. A small bony fragment was identified on a lateral radiograph. Reconstructed axial computed tomography image (C) shows a dorsal cortical fracture of the triquetrum and a sagittal fracture of the pisiform. AO: arbeitsgemeinschaft für osteosyntheses.

Fig. 4
Initial radiographs (A and B) show a distal radial fracture (AO type C3) and an ulnar styloid fracture. However, no carpal bone fracture is shown on simple radiographs. Reconstructed computed tomography images show fractures of the scaphoid waist (C), palmar pole of the lunate (D), and the hook of the hamate (E). AO: arbeitsgemeinschaft für osteosyntheses.

Fig. 5
Initial radiographs (A and B) show a distal radial fracture (AO type C3) and an ulnar styloid fracture. Bony fragments of the distal radial fracture are displaced over the dorsum of the lunate, and a small bony fragment was identified on a lateral radiograph. Reconstructed computed tomography images show a dorsal pole fracture of the scaphoid (C), a cartilage injury of the dorsal pole of the lunate (D), a dorsal cortical fracture of the triquetrum, and a comminuted fracture of the pisiform (E). AO: arbeitsgemeinschaft für osteosyntheses.
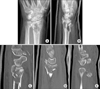
Table 2
The Frequency of Fractures of Each Carpal Bone That Complicated 223 Distal Radial Fractures

Subtypes of carpal fractures were classified according to Vigler et al.8)
References
1. Osterman AL, VanDuzer ST. Arthroscopy in the treatment of distal radial fractures with assessment and treatment of associated injuries. Atlas Hand Clin. 2006. 11(2):231–241.
2. Lindau T, Arner M, Hagberg L. Intraarticular lesions in distal fractures of the radius in young adults: a descriptive arthroscopic study in 50 patients. J Hand Surg Br. 1997. 22(5):638–643.
3. Geissler WB, Freeland AE, Savoie FH, McIntyre LW, Whipple TL. Intracarpal soft-tissue lesions associated with an intra-articular fracture of the distal end of the radius. J Bone Joint Surg Am. 1996. 78(3):357–365.
4. Turner RG, Faber KJ, Athwal GS. Complications of distal radius fractures. Hand Clin. 2010. 26(1):85–96.
5. Wolfe SW. Wolfe SW, Hotchkiss RN, Pederson WC, Kozin SH, editors. Distal radius fractures. Green's operative hand surgery. 2011. 6th ed. Philadelphia, PA: Churchill Livingstone;561–638.
6. Pretell-Mazzini J, Carrigan RB. Simultaneous distal radial fractures and carpal bones injuries in children: a review article. J Pediatr Orthop B. 2011. 20(5):330–333.
7. Muller ME, Nazarian S, Koch P, Schatzker J. The comprehensive classification of fractures long bones. 1990. New York: Springer-Verlag;54–63.
8. Vigler M, Aviles A, Lee SK. Carpal fractures excluding the scaphoid. Hand Clin. 2006. 22(4):501–516.
9. Papp S. Carpal bone fractures. Hand Clin. 2010. 26(1):119–127.
10. Welling RD, Jacobson JA, Jamadar DA, Chong S, Caoili EM, Jebson PJ. MDCT and radiography of wrist fractures: radiographic sensitivity and fracture patterns. AJR Am J Roentgenol. 2008. 190(1):10–16.
11. Kiuru MJ, Haapamaki VV, Koivikko MP, Koskinen SK. Wrist injuries; diagnosis with multidetector CT. Emerg Radiol. 2004. 10(4):182–185.
12. van Onselen EB, Karim RB, Hage JJ, Ritt MJ. Prevalence and distribution of hand fractures. J Hand Surg Br. 2003. 28(5):491–495.
13. Hove LM. Fractures of the hand: distribution and relative incidence. Scand J Plast Reconstr Surg Hand Surg. 1993. 27(4):317–319.
14. Trumble TE, Benirschke SK, Vedder NB. Ipsilateral fractures of the scaphoid and radius. J Hand Surg Am. 1993. 18(1):8–14.
15. Rutgers M, Mudgal CS, Shin R. Combined fractures of the distal radius and scaphoid. J Hand Surg Eur Vol. 2008. 33(4):478–483.
16. Carter PR, Frederick HA, Laseter GF. Open reduction and internal fixation of unstable distal radius fractures with a low-profile plate: a multicenter study of 73 fractures. J Hand Surg Am. 1998. 23(2):300–307.
17. Smith DW, Brou KE, Henry MH. Early active rehabilitation for operatively stabilized distal radius fractures. J Hand Ther. 2004. 17(1):43–49.
18. Lozano-Calderon SA, Souer S, Mudgal C, Jupiter JB, Ring D. Wrist mobilization following volar plate fixation of fractures of the distal part of the radius. J Bone Joint Surg Am. 2008. 90(6):1297–1304.
19. Smith DK, Murray PM. Avulsion fractures of the volar aspect of triquetral bone of the wrist: a subtle sign of carpal ligament injury. AJR Am J Roentgenol. 1996. 166(3):609–614.
20. Cockshott WP. Distal avulsion fractures of the scaphoid. Br J Radiol. 1980. 53(635):1037–1040.
21. Slutsky DJ. Predicting the outcome of distal radius fractures. Hand Clin. 2005. 21(3):289–294.




 PDF
PDF ePub
ePub Citation
Citation Print
Print



 XML Download
XML Download