Abstract
Background
The management of the pulseless perfused hand in association with a supracondylar humerus fracture following operative stabilisation remains controversial. Previous authors have suggested the use of color-flow duplex monitoring, magnetic resonance angiography and segmental pressure monitoring as objective steps to ascertain blood flow following adequate internal fixation. We examine the use of the waveform of the pulse oximeter in objectively determining a perfused limb and in predicting the need for surgical exploration in patients who present with a pulseless perfused hand after operative stabilisation for supracondylar fracture of the humerus.
Methods
A retrospective review of all supracondylar fractures over a 60 month duration (2005-2009) in our instituition was performed. Each electronic record was reviewed and limbs which had absent radial pulse following admission were identified. X-ray films of each of the patients were reviewed. A search using the Pubmed database was performed with the following keywords, supracondylar humerus fracture, pediatric, pulseless, vascular injury, arterial repair.
Results
In this series of pulseless perfused hands following operative fixation of supracondylar fracture, a total of 26 patients were reviewed. All were Gartland grade III extension type fractures. Postoperative pulse oximeter waveforms were present in all but 4 patients. These patients subsequently had exploration of the brachial artery with significant findings. In the remaining 22 patients, waveforms were present and the child had return of the radial pulse soon after operative fixation without any further need for surgical exploration. At 24 months follow-up, all children were well with no neurovascular compromise.
Conclusions
The presence of a waveform on a pulse oximeter is a sensitive and easily available modality in determining vascular perfusion as compared to other more complex investigations. The high sensitivity of this test will allow surgeons to objectively determine the requirement for surgical exploration of the brachial artery.
The pulseless pediatric supracondylar fracture of the humerus is often treated with emergent operative stabilization with closed reduction and percutaneous pinning (CRPP).1) In younger children, the use of clinical assessment and ultrasonographic diagnosis may be difficult due to the fretful nature of the child. This forms the basis of investigating the clinical usefulness of a pulse oximeter in pulseless perfused hands both in diagnosis and in deciding for surgical exploration postfixation.
At presentation to the emergency department, three scenarios manifest: 1) a pulseless hand, 2) a hand with intact but diminished pulse volume in comparison with the contralateral side, 3) a hand with an intact radial pulse. Postfixation, three scenarios manifest: 1) a poorly perfused hand with an absent radial pulse. This group will most likely require brachial artery exploration, 2) a perfused hand with a good radial pulse. This group does not need any further intervention, 3) a perfused hand with no radial pulse. This is the group of patients which we are interested in and will be referred to as the "pulseless perfused hand."
Our study looked specifically at the presence or absence of a waveform of the pulse oximeter in a child who presents with a pulseless hand and the waveform following adequate stabilization via CRPP.
There is no consensus on the treatment of the pulseless perfused hand following operative fixation. Various treatments such as observation,2) arteriography,3,4) magnetic resonance angiography,4) emergent exploration5-8) and delayed exploration9) have been suggested following fracture stabilization.
The purpose of our study is first to determine the usefulness of pulse oximetry in diagnosis of the pulseless hand and second, its usefulness as a predictor for the need of brachial artery exploration in children who were found to have pulseless perfused hands.
This is an Institutional Review Board (IRB) approved retrospective sequential review of case notes and X-rays of all children admitted to our institution between 2005 and 2009 with a displaced supracondylar humerus fracture. All children were followed at least 24 months.
Upon admission to the emergency department, all children were examined clinically and had a pulse oximeter probe placed over the ipsilateral hand. The inclusion criteria was a pulseless perfused hand following a supracondylar fracture of the distal humerus as defined by an objective finding of no waveform on the Nellcor N395 pulse oximeter (Coviden, Boulder, CO, USA).
We reviewed the medical records to determine demographic information, mechanism of injury, perfusion and pulse oximeter readings on admission. Associated nerve palsies and radiographs were reviewed. We used the modified Gartland's classification system10) to ascertain the grade of the fracture. The type of operative intervention and the intraoperative findings was examined. All patients had immediate postoperative evaluation of the hand in the area of color, perfusion and pulse oximeter waveform readings. As mentioned above, the pulse oximeter used in this study was a Nellcor N395 pulse oximeter. A good waveform (Fig. 1) and a poor or absent wave form (Fig. 2) is illustrated.
We defined a pulseless supracondylar humerus fracture as having no palpable radial pulse despite full extension of the elbow and a well perfused hand with capillary refill of less than 2 seconds. Subsequent examination findings 1 hour postsurgery and 12 hours postsurgery were also documented. All patients were followed for a minimum of 24 months and then referred back under the care of their regular physicians. Patients with an absent radial pulse and who had an absent pulse oximeter waveform post CRPP had open exploration of the brachial artery. Open exploration of the brachial artery was undertaken by a consultant vascular surgeon using a standard anteromedial approach.
A total of 3,182 patients presented to our department with a supracondylar humerus fracture from 2005 to 2009. 781 children sustained displaced supracondylar fractures of Gartland grade IIb or III and were admitted for operative stabilization.
In the emergency department, the above criteria for determining if a hand was pulseless were applied. We identified 37 (4.7%) patients presenting with a pulseless hand following a supracondylar humerus fracture. All were grade III extension-type fractures and were closed injuries. All 37 received closed reduction and percutaneous pinning emergently within 6 hours of presenting to the hospital. All patients had near anatomic reduction and restoration of the Baumann's angle. Postoperatively, 11 patients had return of the radial pulse. The remaining 26 patients had no palpable radial pulse but had a perfused hand with good capillary refill. Each of these patients had a pulse oximeter applied intraoperatively and in retrospective analysis were divided into 2 groups.
This group had 22 patients. All patients had a good waveform and at the 1 hour postoperative review, had an intact radial pulse. The radial pulse remained present over the next 24 hours. At follow-up, all patients continued to have intact radial pulses. Seven of the patients had a documented anterior interosseous nerve injury which recovered by the 3rd month postsurgery. No patient subsequently developed ischemic contractures or noted any forearm claudication in their school physical exercise classes.
This group had four patients and all received emergent open exploration of the brachial artery. In three cases, anatomical pathology was observed in the brachial artery. One case had entrapment of the brachial artery in the fracture site (Table 1, subject 26). In two cases, the artery was tented by the supratrochlear branch of the brachial artery (Table 1, subjects 12 and 21). Although radiological reduction was obtained in subjects 12 (Fig. 3) and 21 (Fig. 4), the supratrochlear branch of the brachial artery remained tethered by the unossified components of the fracture, the torn periosteum and the jagged edge of the fracture. These were not obvious on the plain radiographs documenting the reduction. The ligation of the binding supratrochlear branch and the freeing of the entrapped brachial artery in these 3 cases led to a prompt return of the radial pulse intraoperatively. The fourth case (Table 1, subject 9), had a large hematoma in the anteromedial cubital fossa but no appreciable pathology over the brachial artery. Following evacuation of the hematoma, radial pulse promptly returned. In the early postoperative period, the radial pulse remained present 24 hours postoperative and during all subsequent follow-up visits.
All 4 patients remained well and at 24 months, had a palpable radial pulse with no intervening events of restenosis. Of the 4 cases only 1 had concomitant nerve injury affecting the anterior interosseus nerve. The nerve injury recovered at follow-up. All 4 patients did not have any eventual loss of function or forearm claudication. No patients in group 1 or group 2 developed forearm compartment syndrome.
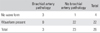
At long term follow-up, no patients in our series had any long term sequelae of Volkmann ischemic contracture. All patients achieved fracture union and were discharged from follow-up once they had reached at least 24 months of follow-up from the date of injury (Table 1). Of the remaining 744 supracondylar fractures requiring CRPP, none developed ischemic contractures. Table 2 summarizes the effectiveness of using this test in predicting the need for exploration based on the waveform obtained via pulse oximetry.
Current literature points to many studies using color flow Doppler ultrasound in the emergency department, perioperative and postoperative setting as a tool in determining the patency of the brachial artery in the setting of a pulseless supracondylar humerus fracture.4,11,12) To our knowledge, this is the first study in pulseless supracondylar humerus fractures that uses the pulse oximeter in diagnosis to conclusion of treatment with excellent results.
Pulse oximetry waveform is used to determine the need for vascular exploration. None of our patients developed Volkmann's ischemic contracture and all of them had successful return of the radial pulse at 24 hours postprocedure and at 1 year follow-up.
We recognize that a child who may have a diminished pulse at presentation may eventually have a pulseless hand as part of a continuum of fracture hematoma and compression of the brachial artery. A child with a brachial artery intimal damage which may progress to late brachial artery occlusion may also not be recognized in the initial setting. These subjects would not have been included in our study as a waveform would have been present at presentation. Thus, we looked at the remaining 744 patients to detect if there was any delayed compartment syndrome, late ischemic contracture or forearm claudication but none was found in the postoperative examination at 24 hours or in subsequent outpatient follow-up.
With that background, we propose a treatment algorithm using the pulse oximeter for children with supracondylar humerus fractures presenting with an absent pulse (Fig. 5).
Traditionally, many authors have advocated observation as a treatment of choice.2,4,13) Increasingly, many have advocated early intervention once there is recognition of vascular injury. Noaman14) explored the brachial artery in 31 children in whom the radial pulse was absent after closed reduction and pinning in a series of 840 grade III fractures. His indications were a pulseless forearm with a pink or cold hand, an absent radial pulse one hour after satisfactory closed reduction and percutaneous pinning and an absent radial pulse associated with an open fracture or signs of tethering of the brachialis muscle. There was arterial damage in 30 children and in one the artery was released from the site of the fracture. Korompilias et al.,15) in his series of 5 children with a pink, pulseless hand also recommended surgical exploration to restore the patency of the brachial artery even in the presence of a viable and well-perfused hand after an attempt at closed reduction.
Most recently, White et al.7) systematically reviewed 19 papers in the English literature where pulseless and perfused supracondylar fractures were managed. A total of 331 such fractures were recorded. Of these, 157 remained pulseless post reduction. Of this group, 90% underwent surgical exploration and 82% was found to have brachial artery injury. This paper also went on to analyze the results of patency of the brachial artery following exploration and in 54 such explorations 91% remained patent at the 1 year follow-up. While the results of this review appear to indicate that brachial artery injury was much higher than our series, we believe that there is some selection bias using pooled retrospective data from 19 such studies. We experienced similar levels of patency of the brachial artery postsurgical exploration at the 1 year follow-up (100%). This systematic review further supports early intervention once there is recognition of brachial artery pathology and challenges early suggestions of 'watchful waiting'.
In contrast, Ramesh et al.16) reported a series of patients with well perfused hands but absent radial pulse following humerus supracondylar fracture fixation. The author cautioned that these patients did not have excruciating pain distal to the elbow that persisted beyond 12 hours after the injury as compared to the series by Blakey et al.9) This demonstrates that the upper limb has an extremely good collateral blood supply.
The abundant collateral supply of the elbow comes from the superior and inferior ulnar collateral artery medially and the profunda brachii artery laterally. These arteries branch from the brachial artery proximal to the olecranon fossa, where supracondylar humerus fractures frequently occur. The profunda brachii artery branches to give a radial recurrent branch and an interosseous recurrent branch. The superior ulnar collateral artery runs posterior to the medial epicondyle to form the posterior ulnar recurrent artery. The inferior ulnar collateral artery runs anterior to the medial condyle of the humerus to become the anterior ulnar recurrent artery. The radial recurrent and both the ulnar recurrent arteries then rejoin the radial and ulnar artery respectively at the level of the biceps insertion on the radial neck.17) This rich collateral network forms the basis for pulseless perfused hands (Table 1, subject 26) despite brachial artery entrapment at the level of the supracondylar humerus.
While we have no patient in our study with both an absent radial pulse and a well perfused limb on long term follow-up, we recognize that it may be possible for a waveform to be present despite brachial artery occlusion due to the rich network of collaterals at the elbow joint. Our study however did not show any patients who did not have return of the radial pulse once intraoperative pulse oximetry showed a good waveform. This may be a limitation of our study due to its small sample size or may indicate that pulse oximetry is truly objective in determining the eventual return of the radial pulse. At a minimum of 24 months follow-up, all patients had well palpable radial pulses indicating that stenosis or delayed intimal damage resulting in occlusion unlikely occurred.
We are of the opinion that given the readily available resource of the pulse oximeter in the operating room, the challenges of subjectivity in monitoring pain in the postoperative patient and the good results following surgical exploration of the brachial artery that surgical exploration should be undertaken once there is documented injury to the brachial artery. Our study demonstrates that the pulse oximeter is an objective tool to support or reject the decision for surgical exploration.
Mangat et al.18) advocated that the likelihood of vascular injury was high with documented anterior interosseous nerve or median nerve injury in his series of 19 patients over a 14-year period. Our study showed different results as only 1 patient who required surgical exploration with positive findings of brachial artery pathology had nerve injury at presentation. In the group which had a good waveform and which did not require exploration, 7 patients had nerve injury which recovered during follow-up. None of these patients required surgical exploration. We surmise that nerve injury, while associated with the incidence of brachial artery pathology in a pulseless hand, is not an objective predictor of surgical exploration.
The use of pulse oximetry allows easy access and is a relatively cheap alternative to Doppler ultrasound. Furthermore, it removes the subjectivity in examining the peripheral nerves in an already fretful and irritable child. This allows earlier diagnosis and treatment of the pulseless limb following supracondylar fracture.
Previous authors have also suggested the use of angiography to assess the vascular status of the affected limb.3,19) Shaw et al.11) expressed that this may potentially increase the time required before a vascular exploration. Angiography is also invasive and has risks of iatrogenic injury to the artery due to its small size.20) In addition, there are also risks of contrast allergy.
We recognize that the use of the pulse oximeter in colder environments may lead to false positives as a result of peripheral vasoconstriction. However, this scenario was avoided by adequately warming the operating theatre.
We acknowledge limitations to our study with respect to its limited sample size and the lack of imaging or exploration to confirm the absence of injury to the brachial artery. Based on the eventual presence of a radial pulse, this study shows a positive predictive value of 0.75, and a negative predictive value of 1.0. We will need to continue evaluating this with increasing numbers that are added to our study population over time. We are optimistic that this test has a high specificity of 95.65%, and would want to embark on future studies that test the true effectiveness of the algorithm and to pit the results of the pulse oximeter with that of color flow Doppler in a prospective context to assess the patency of the brachial artery.
In conclusion, the pulse oximeter is an excellent and readily available tool in the emergency department and the operative room to assist diagnosis of the pulseless hand and subsequently, to discern arterial injury in well perfused, postfixation supracondylar humerus fractures.
Figures and Tables
Fig. 3
Subject 12 (Table 1), preoperative film (A) and postoperative film (B). Note the fine jagged edge of the fracture site in the anterior humerus. Radiological indices are restored.

References
1. Green NE. Green NE, Swiontkowski MF, editors. Fractures and dislocations about the elbow. Skeletal trauma in children. 2002. 3rd ed. Philadelphia: Saunders;257–321.
2. Garbuz DS, Leitch K, Wright JG. The treatment of supracondylar fractures in children with an absent radial pulse. J Pediatr Orthop. 1996. 16(5):594–596.
3. Shuck JM, Omer GE Jr, Lewis CE Jr. Arterial obstruction due to intimal disruption in extremity fractures. J Trauma. 1972. 12(6):481–489.
4. Sabharwal S, Tredwell SJ, Beauchamp RD, et al. Management of pulseless pink hand in pediatric supracondylar fractures of humerus. J Pediatr Orthop. 1997. 17(3):303–310.
5. Schoenecker PL, Delgado E, Rotman M, Sicard GA, Capelli AM. Pulseless arm in association with totally displaced supracondylar fracture. J Orthop Trauma. 1996. 10(6):410–415.
6. Copley LA, Dormans JP, Davidson RS. Vascular injuries and their sequelae in pediatric supracondylar humeral fractures: toward a goal of prevention. J Pediatr Orthop. 1996. 16(1):99–103.
7. White L, Mehlman CT, Crawford AH. Perfused, pulseless, and puzzling: a systematic review of vascular injuries in pediatric supracondylar humerus fractures and results of a POSNA questionnaire. J Pediatr Orthop. 2010. 30(4):328–335.
8. Reigstad O, Thorkildsen R, Grimsgaard C, Reigstad A, Rokkum M. Supracondylar fractures with circulatory failure after reduction, pinning, and entrapment of the brachial artery: excellent results more than 1 year after open exploration and revascularization. J Orthop Trauma. 2011. 25(1):26–30.
9. Blakey CM, Biant LC, Birch R. Ischaemia and the pink, pulseless hand complicating supracondylar fractures of the humerus in childhood: long-term follow-up. J Bone Joint Surg Br. 2009. 91(11):1487–1492.
10. Beaty JH, Kasser JR . Beaty JH, Kasser JR, editors. Supracondylar fractures of the distal humerus. Rockwood and Wilkins' fractures in children. 2005. Philadelphia: Lippincott Williams & Wilkins;577–624.
11. Shaw BA, Kasser JR, Emans JB, Rand FF. Management of vascular injuries in displaced supracondylar humerus fractures without arteriography. J Orthop Trauma. 1990. 4(1):25–29.
12. Fry WR, Smith RS, Sayers DV, et al. The success of duplex ultrasonographic scanning in diagnosis of extremity vascular proximity trauma. Arch Surg. 1993. 128(12):1368–1372.
13. Malviya A, Simmons D, Vallamshetla R, Bache CE. Pink pulseless hand following supra-condylar fractures: an audit of British practice. J Pediatr Orthop B. 2006. 15(1):62–64.
14. Noaman HH. Microsurgical reconstruction of brachial artery injuries in displaced supracondylar fracture humerus in children. Microsurgery. 2006. 26(7):498–505.
15. Korompilias AV, Lykissas MG, Mitsionis GI, Kontogeorgakos VA, Manoudis G, Beris AE. Treatment of pink pulseless hand following supracondylar fractures of the humerus in children. Int Orthop. 2009. 33(1):237–241.
16. Ramesh P, Avadhani A, Shetty AP, Dheenadhayalan J, Rajasekaran S. Management of acute 'pink pulseless' hand in pediatric supracondylar fractures of the humerus. J Pediatr Orthop B. 2011. 20(3):124–128.
17. McMinn RM. Last's anatomy: regional and applied. 1994. 9th ed. New York: Churchill Livingstone;78–96.
18. Mangat KS, Martin AG, Bache CE. The 'pulseless pink' hand after supracondylar fracture of the humerus in children: the predictive value of nerve palsy. J Bone Joint Surg Br. 2009. 91(11):1521–1525.
19. Luria S, Sucar A, Eylon S, et al. Vascular complications of supracondylar humeral fractures in children. J Pediatr Orthop B. 2007. 16(2):133–143.
20. Shaker IJ, White JJ, Signer RD, Golladay ES, Haller JA Jr. Special problems of vascular injuries in children. J Trauma. 1976. 16(11):863–867.




 PDF
PDF ePub
ePub Citation
Citation Print
Print







 XML Download
XML Download