Abstract
Background
This study examined the clinical outcomes of indirect reduction maneuver and minimally invasive approach for treating displaced proximal humerus fractures in patients older than 60.
Methods
Thirty-two patients (11 male and 21 female) who had undergone treatment for displaced proximal humerus fracture were evaluated. The mean age of the patients was 72.4 years (range, 60 to 92 years). All cases were followed up for at least 12 months. All patients were interviewed and evaluated on the visual analog scale, with gender-specific constant score correction for age, standardized X-rays to check the neck-shaft angle (NSA) and the presence of medial support, and bone mineral density. Statistical analysis was performed with a multiple regression analysis.
Results
The average visual analog scale score was 2.4, and the average gender-specific constant score correction for age was 80.6 points. Final functional outcomes were 8 excellent, 15 good, 7 fair, and 2 poor. The average NSA was 122.8°; and the radiological results were 20 good, 11 fair, and 1 poor. There was significant difference of the gender-specific constant score for age between the group of NSA more than 110° and the group of NSA less than 110° (p = 0.00). There were 26 cases with and 6 cases without medial support, with significant difference between the gender-specific constant score correction for age of these groups (p = 0.01). Complications occurred in 4 patients (12.5%).
Conclusions
The indirect reduction maneuver and minimally invasive approach were safe and reliable options for the treatment of displaced proximal humerus fractures in the elderly patients. An inadequate reduction (i.e., less than 110° NSA) or lack of medial support (e.g., no cortical or screw support) were significant factors contributing to poor functional outcomes.
Proximal humerus fractures with minimal displacement and adequate stability are usually treated conservatively. In contrast, displaced fractures have a wide variety of surgical treatment options. Many treatment methods have been introduced, such as open reduction and internal fixation with multiple K-wires and screws fixation, various types of proximal humeral plates, use of intramedullary nails, and prosthetic replacement. Several complications have been described in association with these techniques, including reduction loss, implant failure, nonunion or malunion, impingement, and osteonecrosis of the humeral head.1,2) If adequate reduction is not achieved or the medial buttress is not sufficient, reduction loss and subsequent fixation failure are possible, especially in osteoporotic elderly patients.3)
Recent advances in the local anatomy, fracture geometry, implant design, surgical approach, and fixation techniques have led to minimally invasive approaches to treating proximal humerus fractures. Minimally invasive techniques have been developed to reduce the rate of avascular necrosis and nonunion, which have been attributed to soft tissue disruption and local blood supply impairment. Adequate reduction may be achieved using an indirect reduction maneuver. A biomechanical study suggested that angular stable locking plates could also resist the physiologic loads encountered in osteoporosis.4)
Several clinical studies have described minimally invasive plate osteosynthesis, but few have documented the importance of an indirect reduction and clinical results of a minimally invasive approach for displaced proximal humerus fractures, including three- and four-part fractures.3,5) The aim of this study was to examine the clinical outcomes of an indirect reduction maneuver and a minimally invasive approach for treating displaced proximal humerus fractures in elderly patients.
The study population comprised 38 patients older than 60 years, who had undergone treatment for proximal humerus fractures at our institution between March 2007 and August 2010, and provided informed consent to participate. Twenty-five patients were admitted after slipping down, and seven after automobile accidents. The inclusion criteria of this study, based on the Neer classification,6) were as follows: fracture of the shoulder joint; greater than 10 mm displacement of the fracture fragment and 5 mm displacement of the greater tuberosity; angular displacement greater than 45°; and loss of the medial metaphyseal column. The exclusion criteria were two part fractures involving only the greater or lesser tuberosity, open fractures, pathological fractures, and concomitant neurovascular injury. Four patients were lost to follow-up, while 1 patient with previous shoulder surgery and 1 patient with AO type C3 fracture, which needed additional arthrotomy to reduce the dislocation of the fragment, were excluded. Overall, 32 patients (11 male and 21 female) were included. The mean age of the patients was 72.4 years (range, 60 to 92 years) (Table 1). Fractures were categorized according to the Neer6) and AO classification systems.7) A computed tomography was used to confirm the degree of an articular involvement of the intra-articular fractures.
All cases were followed-up for at least 12 months (range, 12 to 48 months), and 25 of the cases were followed-up for more than 24 months. At the last follow-up, patients were examined and interviewed in regards to the functional and radiological outcomes. Patients subjectively evaluated their pain according to the visual analog scale (range, 0 to 10 points). Constant scores8) were used to assess shoulder pain (range, 0 to 15 points), strength (range, 0 to 25 points), activities of daily living (range, 0 to 20 points), and range of motion (range, 0 to 40 points). Functional results according to the constant score were classified as excellent (≥ 86 points), good (71 to 85 points), fair (56 to 70 points), and poor (≤ 55 points). The constant scores were then corrected for gender and age.
Standardized X-rays in the anteroposterior and axillary lateral views were used to evaluate the fracture healing, neck-shaft angle (NSA) by Paavolainen et al.,9) and presence of medial support. We categorized the patients into the group with NSA more than 110° and less than 110°; and the gender-specific constant score correction for age of the group with NSA more than 110° were compared to those of the group less than 110°. The presence of medial support was defined by Gardner et al.10) as the anatomic reduction of the medial cortex, lateral impaction of the proximal fragment in the distal shaft fragment, or an oblique locking screw positioned inferomedially. The gender-specific constant score correction for age of the group with medial support (presence group) was compared with that of the group without medial support (absence group).
This study was approved by Institutional Review Board Committee of Samsung Medical Center.
The procedure was performed under general anesthesia with the patient placed in the supine position on radiolucent table with a 10 cm high shoulder pillow to elevate both shoulders. In our experience, the intraoperative image intensifier is more effective with the patient in the supine position than in the beach chair position, and the cephalad positioning is superior for performing the operation.
An indirect reduction maneuver was attempted. In case of a three-part fracture, the pectoralis major muscle pulled the humeral shaft medially, and the deltoid raised the shaft against gravity. The articular fragment generally fell and impacted into the defect of broken tuberosities or sometimes elevated. The supraspinatus and infraspinatus displaced the greater tuberosity cranially and dorsally (Fig. 1A). First, a longitudinal traction to the arm with counter traction was applied against the deltoid. After confirming the disengagement of the head to shaft, a lateral compression to the humeral shaft was applied against the pectoralis major next. Last, an abduction, internal rotation, and elevation of the humeral shaft aligned with greater and lesser tuberosity was gently applied. All procedure was performed while being checked under an image intensifier (Fig. 1B).
The affected shoulder was then prepped and draped in the routine manner. In a deltoid splitting approach, the acromion was used as a landmark of the anterolateral edge. Since the axillary nerve was located 6.3 ± 0.5 cm below the acromion by Gardner et al.,11) an assumed nerve course was marked or sutured 5 cm distal from the acromion, and this line was not crossed. A skin incision was made beginning at the anterolateral tip of the acromion extending approximately 5 cm distally. The subcutaneous tissue, fascia, and deltoid muscle were dissected to expose the great tuberosity, but the deltoid muscle was not dissected to expose the axillary nerve and circumflex artery. A 3 cm distal incision with longitudinal split of the deltoid muscle insertion was developed to place the plate. A submuscular tunnel along the humeral shaft was created using an elevator. An indirect reduction was tried again as described previously. If the head fragment was derotated, elevated, or impacted, it could be reduced using an elevator as a joy stick. The greater tuberosity also could be reduced using a hook or a reduction clamp.
A plate was then inserted through the created tunnel at least 5 mm distal to the greater tuberosity and 2 mm posterior to the bicipital groove. The PHILOS plates (Synthes Inc., Stratec Medical Ltd., Solothurn, Switzerland) were used in all cases. Care was taken to ensure that sufficient space was maintained between the plate and tendon of the long head of the biceps to prevent damage to the anterior humeral circumflex bundle. The position of the plate was corrected using proximal and distal drill sleeves.
The most distal, or second most distal, screw was inserted first to place the plate in a central position on the humeral shaft. Proximal locking screws were then inserted in sequence. The most proximal four to six screws were not in a location to threaten the axillary nerve, according to results by Smith et al.12) If needed, a greater tuberosity repair was augmented by nonabsorbable sutures through the rotator cuff tendons and proximal suture holes in the plate, or a rotator cuff repair was performed if necessary (Fig. 1C). The longitudinally split deltoid was sutured from anterior to posterior over the plate. The correct plate and screw placement and fixation stability were verified radiologically (Fig. 1D). This procedure was applied to two-, three-, and four-part fractures (Fig. 2).
The shoulder was immobilized with a U slap shoulder splint covering the shoulder joint for three to four weeks after the operation. Passive motion exercise in the scapular plane, without arm rotation, was initiated on the first day following surgery. Controlled active mobilization was started one to three weeks after surgery, depending on stability and bone quality. After three to four weeks, the splint was removed, and active exercises were begun.
There were 15 cases of two-part, 12 cases of three-part, and 5 cases of four-part fractures. There were 10 cases of type A (A1, 2; A2, 4; A3, 4), 14 cases of type B (B1, 8; B2, 5; B3, 1), and 8 cases of type C (C1, 6; C2, 2; C3, 0) fractures. The average visual analog scale score was 2.4 points (range, 0 to 5 points), and the average constant score was 75.7 points (range, 35 to 90 points). The average four subscales of the constant score were 13.1 points (pain, range 8 to 15 points), 18.8 points (strength, range 10 to 25 points), 17.5 points (activities of daily living, range 12 to 20 points), and 26.3 points (range of motion, range 10 to 35 points). The average of gender-specific constant score correction for age was 80.6 points (range, 53 to 92 points). The mean forward flexion, lateral abduction, internal rotation, and external rotation were 145.5° (range, 120° to 180°), 128.7° (range, 100° to 180°), 77.5° (range 60° to 90°), and 34.1° (range, 30° to 80°), respectively. Final functional outcomes were: 8 excellent, 15 good, 7 fair, and 2 poor (Table 2).
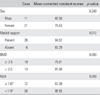
The average NSA was 122.8° (range, 90° to 140°), and radiological results were 20 good, 11 fair, and 1 poor. There was a significant difference between the gender-specific constant score correction for age of the good group and those of the poor group (p = 0.00). There were 26 cases of presence and 6 cases of absence of medial support. There was also a significant difference between the gender-specific constant score correction for age of the presence group and those of the absence group (p = 0.01) (Table 3).
Complications occurred in 4 patients (12.5%) of 32 patients (Table 4). One patient (3.1%) suffered plate impingement, as the plate was positioned too far cranially; and symptoms improved after plate removal. One patient (3.1%), who had underlying diabetes mellitus and early liver cirrhosis, had a superficial wound infection that required surgical debridement and delayed suture. One patient (3.1%) had a fixation failure and required a conversion to a prosthetic replacement. She had a varus malreduction of 30° and, ultimately, collapse of the humeral head four weeks postoperatively. None of the patients had the osteonecrosis of the humeral head. One patient underwent revision to a prosthetic replacement. Three patients were suspected of having axillary nerve injury, as they had difficulty in elevating forward flexion and lateral abduction. However, only one (3.1%) of the three patients was diagnosed as an axonotmesis by the electromyelography and nerve conduction velocity testing; and the shoulder pain and motion of this patient improved spontaneously at the last follow-up. The possible causes included temporary deltoid weakness as a consequence of the deltoid split approach, adhesion of the plate to the nerve, and axillary nerve injury during the approach.
The principle goal in the surgical treatment of proximal humeral fractures is to achieve effective stabilization of an adequately reduced fracture to maximize functional outcomes. If adequate reduction is not achieved with a varus malreduction, or the level of bone loss is too great, a subsequent fixation failure is possible, particularly in osteoporotic bones. Correct fixation techniques are essential for preventing reduction loss and collapse of the fracture fragment.
The anterolateral deltopectoral approach is considered the general approach for proximal humerus fractures. However, a substantial soft tissue dissection with a half detachment of the origin of the deltoid muscle is inevitable, which not only jeopardizes the anterior circumflex humeral artery (the main blood supply to the humeral head) but also carries a risk of devascularization of the fracture fragment. Although the union rates of internal fixation with conventional or locking plates are high, the many complications and risks of reoperation result in suboptimal techniques. Thanasas et al.13) reported that patients continued to improve up to one year postoperation, achieving a mean constant score of 74.3. Nevertheless, after a review of twelve studies, including 791 patients, they reported the following incidence of complications: avascular necrosis, 7.9%; screw cut out, 11.6%; and reoperation, 13.7%. Sproul et al.14) who reviewed twelve studies, including 514 patients, reported a mean constant score of 74 and an overall rate of complications of 49%, including varus malunion and a reoperation rate of 14%. This study found an 18.2% overall complication rate, which was presumed to be due to the use of an indirect reduction maneuver and minimally invasive technique. Therefore, the minimally invasive technique has become increasingly popular, coupled with the benefits of locking plates for early functional recovery.
Currently, the biological approach, including the minimally invasive technique, has become more important than the open, extensive approach in osteosynthesis for fracture treatment.15,16) Information on clinical results after the minimally invasive plating of proximal humerus fractures has become more readily available. Lill et al.17) reported favorable results in an early follow-up after applying a locking late in 35 patients. The constant score was 97% of the age- and gender-related normal values (74 points). Lau et al.3) reported that 17 out of 92 patients had complications, indicating an 18.5% complication rate. Another advantage is that minimally invasive techniques are also applied to fractures of the greater tuberosity in osteoporosis as a buttress plate and to metadiaphyseal fractures, using a modified method. Rancan et al.5) reported that minimally invasive, long PHILOS plate osteosynthesis is a safe procedure for the treatment of metadiaphyseal fractures of the proximal humerus. Nevertheless, some authors hold different views regarding the successful treatment. Krappinger et al.2) reported that the bone quality, biological age, anatomic reduction, and medial cortical support are essential for successful surgical treatment. They recommend the consideration of primary arthroplasty, if an anatomic reduction and restoration of the medial cortical support cannot be achieved. Despite the excellent clinical outcomes, the superiority of this technique over alternative methods, such as conservative treatment and open reduction, cannot be proven and may not be over emphasized. However, differences in clinical benefits and complications between a minimally invasive approach and a deltopectoral approach are beginning to be observed.
Knowledge of the fracture geometry and advances in reduction techniques are essential for achieving an adequate reduction. Investigators have used a range of indirect or percutaneous reduction techniques, depending on the type of fracture and fragment displacement.18,19) In four-part fractures, the shaft fragment is medialized by the pull of the pectoralis major. The articular fragment falls into the defect of broken-out tuberosities and becomes elevated or impacted. The supraspinatus and infraspinatus pulls the greater tuberosity cranially and dorsally, and the subscapularis leads the lesser tuberosity to a medial displacement. The longitudinal traction with counter traction against the deltoid, lateral compression to humeral shaft against the pectoralis major, abduction of the shaft aligned with the greater tuberosity, and elevation of the distal shaft were necessary to achieve the good alignment. An indirect reduction maneuver could achieve good alignment in most cases by our experience. If the head fragment is so derotated, elevated, or impacted, and the greater tuberosity is so displaced to reduce, an additional procedure using an elevator, a bone hook, or a reduction clamp may be necessary.20) There are some with concerns for the plate blocking the healing of the detached deltoid insertion. But the repair of the longitudinally split deltoid from anterior to posterior was sufficient for the rehabilitation. It was also confirmed that the deltoid was fully healed with the removal of the plate.
Many surgeons have doubted the possibility of achieving effective stabilization in four-part fractures. In a valgus impacted fracture, indirect reduction and effective stabilization can be achieved, whereas this is difficult to achieve in a varus extended fracture. In a valgus impacted fracture, the plate acts as a mechanical strut under compressive forces resisting valgus subsidence. In a varus extended fracture, the plate functions as a tension band by pulling the humeral head out of varus force.21) This is the most important distinction between a valgus impacted and varus extended fracture. Additional bone grafts, inferomedial screws, or tension band wiring to reinforce the inferomedial metaphyseal region and prevent the collapse of the humeral head should be considered.
The maintenance of NSA and restoration of medial support are important in achieving an adequate reduction. The degree of humeral head angulation has a substantial effect on the final clinical outcomes. Malreduction of the humeral head is the most common technical error in plate fixation. Patients with a poor reduction had greater than 20° of varus malreduction, which resulted in the mechanical loss of fixation and poor subsequent clinical outcomes.
Care should be taken to prevent axillary nerve injury.22) Gardner et al.,11) through a cadaveric study, reported that the axillary nerve was located 6.3 ± 0.5 cm below the acromion. Smith et al.12) reported that the safe zone of the PHILOS plate for proximal screw insertion consisted of the six most proximal holes only. They emphasized the necessity of gentle palpation and digital protection of the nerve during proximal plate and screw insertion. Nonetheless, routine identification of the axillary nerve to avoid traction injury is not recommended. Six patients were suspected of having an axillary nerve injury as they had difficulty elevating in forward flexion and lateral elevation. One patient was diagnosed with axonotmesis.
This study has several limitations. First, this study is a small case series of a prospective study; and many additional cases will be required to validate these findings. Second, another study comparing the deltopectoral and minimally invasive approach will be necessary to improve the quality and validity of the current study. Lastly, the difficulty in classifying many of the fractures confounded interpretation of the data and assignment of the fracture type according to the Neer and AO classifications. An attempt was made to include as many three- and four-part fractures, but some of these fractures may also be regarded as two-part fractures.
In conclusion, an indirect reduction maneuver and minimally invasive approach were safe and reliable treatment options for the displaced proximal humerus fractures in elderly patients. The maintenance of NSA and restoration of medial support were the most important factors. An inadequate reduction, such as less than 100° of NSA, or no medial support, such as no cortical or screw support, were significant factors associated with poor functional outcomes.
Figures and Tables
Fig. 1
(A) Intraoperative C-arm image of a 90-year-old woman with a three-part and B1 fracture. (B) C-arm image after indirect reduction. (C) Photograph of rotator cuff repair with nonabsorbable sutures after minimally invasive plate insertion. (D) A postoperative radiograph demonstrates that the neckshaft angle is 130°, and the medial cortex is anatomically reduced.

Fig. 2
(A, B) Preoperative and one-year postoperative radiographs of a 70-year-old woman with two-part and C1 fracture. (C, D) Preoperative and oneyear postoperative radiographs of a 60-year-old man with three-part fracture and C1 fracture. (E, F) Preoperative and one-year postoperative radiographs of a 65-year-old woman with a four-part and C2 fracture.

References
1. Bogner R, Hubner C, Matis N, Auffarth A, Lederer S, Resch H. Minimally-invasive treatment of three- and four-part fractures of the proximal humerus in elderly patients. J Bone Joint Surg Br. 2008. 90(12):1602–1607.
2. Krappinger D, Bizzotto N, Riedmann S, Kammerlander C, Hengg C, Kralinger FS. Predicting failure after surgical fixation of proximal humerus fractures. Injury. 2011. 42(11):1283–1288.
3. Lau TW, Leung F, Chan CF, Chow SP. Minimally invasive plate osteosynthesis in the treatment of proximal humeral fracture. Int Orthop. 2007. 31(5):657–664.
4. Kralinger F, Gschwentner M, Wambacher M, Smekal V, Haid C. Proximal humeral fractures: what is semi-rigid? Biomechanical properties of semi-rigid implants, a biomechanical cadaver based evaluation. Arch Orthop Trauma Surg. 2008. 128(2):205–210.
5. Rancan M, Dietrich M, Lamdark T, Can U, Platz A. Minimal invasive long PHILOS®-plate osteosynthesis in metadiaphyseal fractures of the proximal humerus. Injury. 2010. 41(12):1277–1283.
6. Neer CS 2nd. Displaced proximal humeral fractures. I Classification and evaluation. J Bone Joint Surg Am. 1970. 52(6):1077–1089.
7. Marsh JL, Slongo TF, Agel J, et al. Fracture and dislocation classification compendium-2007: Orthopaedic Trauma Association classification, database and outcomes committee. J Orthop Trauma. 2007. 21:10 Suppl. S1–S133.
8. Constant CR, Murley AH. A clinical method of functional assessment of the shoulder. Clin Orthop Relat Res. 1987. (214):160–164.
9. Paavolainen P, Bjorkenheim JM, Slatis P, Paukku P. Operative treatment of severe proximal humeral fractures. Acta Orthop Scand. 1983. 54(3):374–379.
10. Gardner MJ, Weil Y, Barker JU, Kelly BT, Helfet DL, Lorich DG. The importance of medial support in locked plating of proximal humerus fractures. J Orthop Trauma. 2007. 21(3):185–191.
11. Gardner MJ, Griffith MH, Lorich DG. Helical plating of the proximal humerus. Injury. 2005. 36(10):1197–1200.
12. Smith J, Berry G, Laflamme Y, Blain-Pare E, Reindl R, Harvey E. Percutaneous insertion of a proximal humeral locking plate: an anatomic study. Injury. 2007. 38(2):206–211.
13. Thanasas C, Kontakis G, Angoules A, Limb D, Giannoudis P. Treatment of proximal humerus fractures with locking plates: a systematic review. J Shoulder Elbow Surg. 2009. 18(6):837–844.
14. Sproul RC, Iyengar JJ, Devcic Z, Feeley BT. A systematic review of locking plate fixation of proximal humerus fractures. Injury. 2011. 42(4):408–413.
15. Kobayashi M, Watanabe Y, Matsushita T. Early full range of shoulder and elbow motion is possible after minimally invasive plate osteosynthesis for humeral shaft fractures. J Orthop Trauma. 2010. 24(4):212–216.
16. Roderer G, Erhardt J, Graf M, Kinzl L, Gebhard F. Clinical results for minimally invasive locked plating of proximal humerus fractures. J Orthop Trauma. 2010. 24(7):400–406.
17. Lill H, Hepp P, Korner J, et al. Proximal humeral fractures: how stiff should an implant be? A comparative mechanical study with new implants in human specimens. Arch Orthop Trauma Surg. 2003. 123(2-3):74–81.
18. Boileau P, Pennington SD, Alami G. Proximal humeral fractures in younger patients: fixation techniques and arthroplasty. J Shoulder Elbow Surg. 2011. 20:2 Suppl. S47–S60.
19. Rouleau DM, Laflamme GY, Berry GK, Harvey EJ, Delisle J, Girard J. Proximal humerus fractures treated by percutaneous locking plate internal fixation. Orthop Traumatol Surg Res. 2009. 95(1):56–62.
20. Resch H, Hubner C, Schwaiger R. Minimally invasive reduction and osteosynthesis of articular fractures of the humeral head. Injury. 2001. 32:Suppl 1. SA25–SA32.
21. Solberg BD, Moon CN, Franco DP, Paiement GD. Surgical treatment of three and four-part proximal humeral fractures. J Bone Joint Surg Am. 2009. 91(7):1689–1697.
22. Liu KY, Chen TH, Shyu JF, Wang ST, Liu JY, Chou PH. Anatomic study of the axillary nerve in a Chinese cadaveric population: correlation of the course of the nerve with proximal humeral fixation with intramedullary nail or external skeletal fixation. Arch Orthop Trauma Surg. 2011. 131(5):669–674.




 PDF
PDF ePub
ePub Citation
Citation Print
Print





 XML Download
XML Download