Abstract
We present a rare case of glomus tumor of Hoffa's fat pad in a 42-year-old woman. Magnetic resonance imaging findings along with the characteristic clinical picture led us to suspect a glomus tumor as the possible etiology. An ischemia test was found to be positive and this further substantiated our diagnosis. An arthroscopic excision was performed and the histology confirmed the diagnosis of glomus tumor of Hoffa's fat pad. The patient responded well to the excision with immediate complete resolution of pain and she remains asymptomatic at the last follow-up after 15 months. To our knowledge, this is the second reported case of glomus tumor of Hoffa's fat pad and the first ever to be managed by simple arthroscopic excision. The tumor poses a great challenge to an orthopedic surgeon. However, knowledge of its characteristic clinical presentation and the recognition of such a rare entity can help achieve an early diagnosis and timely management.
A glomus tumor is a rare benign hamartoma arising from a neuromyoarterial glomus body.1) Glomus tumors account for only 1.6% of soft tissue tumors occurring in the extremities.2) These tumors are typically found in the subungual region, but several case reports of glomus tumors around the knee have been published.3) These tumors have been reported in subcutaneous tissue,4) the patellar ligament5) and beneath the plica synovialis in the knee.3) There is only one previous case report describing a glomus tumor in Hoffa's fat pad,6) which was managed by open excision. These ectopic locations are difficult to diagnose, especially when the lesion is situated in a deep anatomic structure. Despite the patient's presentation with dramatic pain, lack of awareness of these tumors results in a delay in diagnosis and treatment.4) We present a case of a glomus tumor of Hoffa's fat pad in a 42-year-old woman, managed by arthroscopic excision.
A 42-year-old woman presented to us with a history of pain in her right knee for the past one year. The trigger spot for the pain was located just medial to the ligamentum patellae at the level of the joint line. The pain was sharp and shooting in nature and was precipitated by pressure over the trigger spot. The patient was very apprehensive and would not allow repeated examination due to the fear of precipitating the severe pain. The patient was also unable to squat or sit cross legged since deep knee bending would also precipitate the pain. There was no history of aggravation of pain with change in the temperature. She had visited numerous local physicians for the past one year, but despite the dramatic presentation, no diagnosis had been made in the patient till then. Her inflammatory parameters (cell counts, 7,800; erythrocyte sedimentation rate [ESR], 10 mm 1st hour) were normal. A radiograph of the knee was normal. Magnetic resonance imaging (MRI) of the knee revealed a 1 × 1 cm nodule at the inferior aspect of the patella in Hoffa's fat pad. This nodule was hyperintense on T2-weighted images and hypointense on T1-weighted images (Fig. 1). A characteristic clinical picture along with supportive MRI findings led us to suspect glomus tumor as a possible diagnosis. An ischemia test was done at this stage and was found to be positive, and it substantiated our diagnosis. Due to the intraarticular nature of the nodule, no attempt was made to infiltrate it with local anaesthetic.
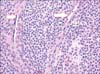
The patient was taken up for arthroscopy of the right knee under a tourniquet. Standard anterolateral and anteromedial portals were used. Intraoperatively, a pedunculated 0.8 × 0.5 cm reddish brown nodule arising from Hoffa's fat pad was seen. A 70° scope was also used to inspect the fat pad. The reddish brown color of the nodule made it easy to differentiate from the surrounding yellow fat pad (Fig. 2). The fat around the pedunculated nodule was carefully shaved to reveal the base. The nodule was excised from the base and the tissue sent for histopathological examination. No separate incision or portal was required to remove the nodule. The fat pad was inspected again and parts of the surrounding synovium were removed to ensure complete removal and decrease the chances of recurrence.
The histological evaluation confirmed the diagnosis of glomus tumor. H&E staining (Fig. 3) revealed a well-circumscribed, encapsulated lesion composed of hyalinized variably sized blood vessels lined by flattened endothelium with the perivascular region showing a solid proliferation of monomorphic round to oval cells with fine chromatin, inconspicuous nucleoli and moderate cytoplasm. A further confirmation was made using immunohistochemisty for smooth muscle actin which showed diffuse cytoplasmic positivity (Fig. 4).
Postoperatively the patient had dramatic total relief from pain and she remains asymptomatic at the last follow-up after 15 months.
Glomus tumors are generally accepted to be uncommon benign soft tissue tumors accounting for 1.6% of all soft tissue tumors occurring in the extremities.2) The normal glomus is an arterio-venous anastomosis which has a role in cutaneous temperature regulation. The first description of a glomus tumor was made in 1872 by Wood.7) However it was Masson 8) in 1924 who described glomus tumor as a benign tumor arising from the neuromyoarterial canal system called the Sucquet-Hoyer canals of the glomus body in the skin.
These tumors are typically found in the subungual region, but several case reports of glomus tumors around the knee have been published.3) When the glomus tumor is in a subcutaneous location, it causes a characteristic reddish-blue discolouration of the skin.4) The tumor has high contact and temperature sensitivity, but in deep and ectopic locations, this temperature sensitivity is not exhibited.6) In our case, the patient did not exhibit temperature sensitivity.
The size of the glomus tumor is small, usually less than 10 mm6) although larger sizes of up to 6 cm in ectopic locations have been reported.9) In our case, the size of the tumor was 8 mm as assessed intraoperatively under a tourniquet. The MRI image suggested a slightly larger size (approximately 1 cm) which makes us believe that these tumors possibly shrink a little once the vascular supply gets cut off.
The quality of the pain and the ability to pinpoint the site are strong indicators of the diagnosis. However, there is frequently a delay in diagnosing tumors in deep and ectopic locations. This may be due to a low index of suspicion. In our case, the patient was not diagnosed for over a year despite presenting with characteristic symptoms.
Clark et al.4) described local infiltration of the glomus tumor, which resulted in relief from pain for a few hours. In our patient, due to the intra-articular nature of the tumor, no such infiltrations were given. An ischemia test however can be done even in intraarticular locations.10) The ischemia test (Hildreth sign) is the disappearance of pain after a tourniquet is placed on the extremity proximal to the lesion. The pain resolves probably because of the vascular nature of the tumor. The positivity of an ischemia test, as in our case, further supports the diagnosis of glomus tumor.
The use of an MRI has been described as the investigation of choice.4) However it does not yield a detailed image of the tumor and remains an adjunct to allow more accurate localization of the tumor.4) Nevertheless the well-circumscribed nature of the lesion and its exact localization, as seen on the MRI, helps rule out other conditions like prepatellar or infrapatellar bursitis, Hoffa's fat pad inflammation, pigmented villonodular synovitis and synovial osteochondromatosis which could all be potential differential diagnoses after clinical assessment in such cases.
The treatment of glomus tumor is complete surgical excision. Dramatic resolution of symptoms occurs. There is only one previous case report describing a glomus tumor in Hoffa's fat pad,5) which was managed by open excision. To our knowledge, ours is the only case in which complete arthroscopic excision of a glomus tumor of Hoffa's fat pad has been carried out with complete resolution of the symptoms.
To conclude, an intraarticular glomus tumor poses a great challenge to an orthopedic surgeon. However, knowledge of its characteristic clinical presentation and the recognition of such a rare entity can help achieve early diagnosis and timely management.
Figures and Tables
Fig. 1
Magnetic resonance imaging of the right knee showing a subcentimeter nodule at the inferior aspect of patella in the Hoffa's fat pad. The nodule was hypointense on T1-weighted images (A) and hyperintense on T2-weighted images (B). (C) Axial image confirmed location in the substance of fat pad.

Fig. 2
(A) Intraoperative arthroscopic view showing a pedunculated reddish brown nodule arising from Hoffa's fat pad. (B) The base of the nodule was revealed after careful shaving of part of fat pad.
References
1. Amillo S, Arriola FJ, Munoz G. Extradigital glomus tumour causing thigh pain: a case report. J Bone Joint Surg Br. 1997; 79(1):104–106.
2. Caughey DE, Highton TC. Glomus tumour of the knee: report of a case. J Bone Joint Surg Br. 1966; 48(1):134–137.
3. Kato S, Fujii H, Yoshida A, Hinoki S. Glomus tumor beneath the plica synovialis in the knee: a case report. Knee. 2007; 14(2):164–166.
4. Clark ML, O'Hara C, Dobson PJ, Smith AL. Glomus tumor and knee pain: a report of four cases. Knee. 2009; 16(3):231–234.
5. Mabit C, Pecout C, Arnaud JP. Glomus tumor in the patellar ligament: a case report. J Bone Joint Surg Am. 1995; 77(1):140–141.
6. Hardy P, Muller GP, Got C, Lortat-Jacob A, Benoit J. Glomus tumor of the fat pad. Arthroscopy. 1998; 14(3):325–328.
7. Wood W. On painful subcutaneous tubercles. Edinb Med J. 1812; 8(5):283–291.
8. Masson P. Le glomus neuro-myo-arteriel des regions tactiles et ses tumeurs. Lyon Chir. 1924; 21:257–280.
9. Kohout E, Stout AP. The glomus tumor in children. Cancer. 1961; 14(3):555–566.
10. Hildreth DH. The ischemia test for glomus tumor: a new diagnostic test. Rev Surg. 1970; 27(2):147–148.




 PDF
PDF ePub
ePub Citation
Citation Print
Print


 XML Download
XML Download