Abstract
Background
A retrospective study was conducted to review the overall survival and treatment outcomes of high grade melanoma in the extremity to explore the clinical features of malignant melanoma of the hand and foot, and the therapeutic efficacies and survival rate after amputation.
Methods
The clinical data of 30 patients with malignant melanoma of the hand and foot (confirmed by pathological examination), who were admitted and treated in our hospital between 2001 and 2010, were analyzed retrospectively. We analyzed variables affecting overall and disease-free survival.
Results
Thirty patients (18 men and 12 women) treated with an amputation procedure for malignant melanoma in the hand or foot constituted the study cohort. The average age of the patients at the time of diagnosis was 58.7 years. Univariate analysis for overall melanoma survival revealed that diagnosis at over 70 years of age, postoperative lymph node metastasis, and location of the tumor were significant prognostic factors. And on the Kaplan-Meier survival curve, old age, American Joint Committee on Cancer stage and postoperative lymph node metastasis showed statistically significant differences in the 5-year survival rate. Also, amputation with aggressive lymph node dissection showed improved long term survival in advanced stage melanoma.
Conclusions
In Korean melanoma patients, for the treatment of high grade melanomas in the extremities after amputation, early diagnosis and postoperative follow-up for evaluation of lymph node metastasis are critical factors for long-term survival. And by performing lymph node dissection during amputation, we may improve the survival rate in advanced stage melanoma patients.
Malignant melanoma is a class of malignant tumors derived from neural crest cells. Its rate of occurrence is low, accounting for 1%-3% of all malignant tumors. Cutaneous melanoma is the most common cause of mortality amongst skin cancers in Caucasian populations1,2) and incidence rates per 100,000 patient years vary between 21.9 in the United States to 55.9 in Australian males.3) In contrast, the incidence of melanoma in Asia is significantly lower with incidence rates of 0.2 to 0.5 per 100,000 patient years.4,5) However, in Asian populations, there are only a few published reports since the incidence is much lower.6-8) In comparison to the cutaneous melanomas arising in Caucasians, they occur more commonly in unusual sites (e.g., hands and feet) in Asians in the form of acral melanomas.3-6) Due to the rarity of their occurrences and acral presentations, diagnosis is often delayed, resulting in more advanced stages of disease at presentation.9) Therefore, advanced stage melanomas on the extremities frequently require wide surgical excision, such as amputation. It is generally believed that melanomas arising in acral locations are initially diagnosed at a more advanced stage and that this may account for its grave prognosis.9) To confirm this, we reviewed our experience in the management of advanced stage melanoma, especially melanoma occurring on the hands and feet, after wide surgical excision, including amputation.
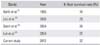
The cases were collected from our melanoma database, and 30 patients who were treated from January 2001 to December 2010 were retrospectively reviewed. Medical records were reviewed for demographics, clinical and pathological information, immediate as well as remote postoperative events and outcomes, with a minimal follow-up of 2 years or death. All patients were advanced stage (American Joint Committee on Cancer [AJCC] stage II and III) melanoma patients, and for the operative treatment, we performed wide marginal surgery, which sometimes involved removal of the bone and surrounding tissue. And without considering the stage of the melanoma, we routinely performed sentinel lymph node dissection in all patients. Therefore, we performed amputation with lymph node dissection for all patients who had melanoma of AJCC stage III (Table 1). After the surgery, we monitored patients for recurrence and metastasis every 3 months for the first 2 years and then gradually lengthened the interval between visits to yearly by the fifth year if no relapse of disease was observed. Patients underwent history, physical examination, chest radiography, and radiography of the affected region at each visit. Computed tomography, magnetic resonance imaging, and whole-body bone scans were obtained selectively, depending on whether there was evidence from the history, physical examination, and radiographs to warrant further study. Data extracted included early diagnosis, sex, location of the tumor (hand or foot), and for the clinical evaluation, we used the AJCC classification.10) Also, patient's mortality, follow-up duration, the date of the first operation, and metastasis to the sentinel lymph node were assessed. Data on survival (from the date of diagnosis to the date of last follow-up or death) for the survival analysis was acquired from our database.
For the statistical analysis, the Kaplan-Meier product was used to estimate curves for survival rate, and the log-rank test was used to evaluate differences between the survival curves. Patients who were lost to follow-up or who were alive at the time of the last follow-up were censored at the date of their last follow-up. A p-value < 0.05 was considered statistically significant. Univariate t-test analysis was used to calculate the relative risk of each parameter. We used the SPSS ver. 18.0 (SPSS Inc., Chicago, IL, USA) to perform statistical calculations and calculated confidence intervals of 95% for the statistical parameters.
Table 1 summarizes the clinical and pathologic data for our patients. Eighteen of the 30 patients (60%) were men and 12 patients (40%) were women, for a male-to-female ratio of 1.5:1. Most were diagnosed while in the sixth or seventh decade of life, with a mean age of 58.7 years (range, 35 to 78 years). All of the patients had AJCC stage II or III disease at initial examination, and lesions were located predominantly on the sole and thumb (Fig. 1).
Thirty patients who were diagnosed with high-grade malignant melanoma, underwent amputation of the tumor-involving extremity. The overall survival of patients after amputation of the malignant melanoma was 93% at 1 year, 76% at 2 years, and 67% at 5 years (Fig. 2). Fourteen of 30 patients were alive without disease, and six patients were dead with the disease at the end of the study (Table 2).
On the univariate analysis, diagnosis when over 70 years of age, tumor located on the lower extremity, and postoperative lymph node metastasis were found to predict poorer survival; and this result was statistically significant (p < 0.05) (Table 3). And on the Kaplan-Meier analysis, patient's gender and location of the tumor did not affect long term survival, whereas age at diagnosis, AJCC stage, and postoperative lymph node metastasis did impact the survival (p < 0.05) (Table 4).
The overall survival curve was plotted according to age, sex, location, AJCC stage, and postoperative lymph node metastasis (Fig. 3). And as mentioned above, there were significant differences in early diagnosis, AJCC stage, and postoperative lymph node metastasis of malignant melanoma (p < 0.05). We also found amputation with aggressive lymph node dissection improved the 5-year overall survival of AJCC stage III patients, with a survival rate of up to 32.1%.
Malignant melanoma is a relatively rare occurrence in the Asian population compared to fair-skinned populations. Limited data are available on skin cancer in Asians, including information on the prevalence rates of malignant melanoma in different Asian populations.11) In Korea, the incidence of malignant melanoma increased from 1.02% of all skin malignancies in the 1980s to 15.6% in the 1990s.12,13) The mean age of diagnosis of melanoma was 58.7 years in our study, which was similar to other studies.14) In Asian populations, malignant melanoma tends to occur 1.5 times more often in males than females, as in our study.14) Unlike other studies, all of our patients were consulted from the dermatologic department with more than AJCC stage II, which is advanced stage malignant melaoma. The difficulty in making the diagnosis of these malignant melanomas and the subsequent delay in proper treatment are factors likely to contribute to the preponderance of advanced lesions seen at the initial presentation.15-17) In this study, all of the patients presented with either AJCC stage II or III, and all cases were more than 1.5 mm thick. These factors (stage, thickness, and level of invasion) are important prognostic parameters in patients with advanced stage melanoma.18-21) After diagnosis of the melanoma, the affected digit must be amputated promptly. Confirming a previous report,17) most studies of subungual melanoma have used amputation with or without lymph node dissection, yielding 5-year survival rates of 16% to 32%,22,23) whereas others using amputation with lymph node dissection or regional limb perfusion have reported 5-year survival rates of 25% to 32%, with minimal morbidity and no mortality.24,25) In addition to amputation, most patients underwent lymph node dissection and regional limb perfusion. Although the use of these treatment modalities did not affect patient survival, perfusion may reduce the incidence of local disease recurrence. There is still controversy about the significance of the anatomical site of origin in prognosis. In our study, 85% of the melanomas were located on the acral area (palm, sole, and subungal area). However, when compared with melanomas arising in other locations, sex and thickness of tumor were not significantly different. According to the location of the tumor, our institution performed wide marginal resection of the tumor, that is, amputation. The principle treatment for primary malignant melanoma is wide marginal excision. But, treatment of melanomas on the hands and feet is particularly challenging for surgeons due to the functional uses of these body parts and the difficulty of obtaining the conventionally recommended margins. However, in cases of advanced stage melanoma as in our studies, amputation is usually required due to the paucity of soft tissue between the tumor and the bone. Therefore, although amputation is not commonly recommended in general, it should be the first recommendation in cases of advanced stage melanomas that have insufficient safety margins. Balch et al.26) reported 5-year survival rates of 13% to 37% in patients who showed lymph node metastasis at the time of diagnosis. Although, in our study, patients who were diagnosed as AJCC stage III showed a poorer survival rate than stage II patients, with aggressive lymph node dissection during the amputation, we found an improved survival rate of AJCC stage III patients of up to 32.1%, higher than in other reports (Table 5).27-30)
In Korean melanoma patients, for the treatment of high grade melanomas on the extremities after amputation, early diagnosis and postoperative follow-up for evaluation of lymph node metastasis are critical factors for long term survival. By performing lymph node dissection during amputation, we may improve the survival rate in advanced stage melanoma patients.
Figures and Tables
Fig. 1
Percentage of malignant melanomas at each site (n = 30). Lesions were most commonly located either on the sole (20%) or thumb (16.7%).

Fig. 2
Kaplan-Meier analysis for overall survival shows long-term survival of 93% at 1 years, 76% at 2 years, and 67% at 5 years.

Fig. 3
Graphs show the effect of potential prognostic factors on survival after amputation. Survival curves of patients divided into two groups according to age at diagnosis (A), gender (B), location of the melanoma (C), American Joint Committee on Cancer (AJCC) stage (D), and postoperative lymph node metastasis (E).

References
1. Jemal A, Siegel R, Ward E, Murray T, Xu J, Thun MJ. Cancer statistics, 2007. CA Cancer J Clin. 2007; 57(1):43–66.

2. Geller AC, Swetter SM, Brooks K, Demierre MF, Yaroch AL. Screening, early detection, and trends for melanoma: current status (2000-2006) and future directions. J Am Acad Dermatol. 2007; 57(4):555–572.

3. Garbe C, McLeod GR, Buettner PG. Time trends of cutaneous melanoma in Queensland, Australia and Central Europe. Cancer. 2000; 89(6):1269–1278.
4. Tanaka H, Tsukuma H, Tomita S, et al. Time trends of incidence for cutaneous melanoma among the Japanese population: an analysis of Osaka Cancer Registry data, 1964-95. J Epidemiol. 1999; 9:6 Suppl. S129–S135.
5. Sng J, Koh D, Siong WC, Choo TB. Skin cancer trends among Asians living in Singapore from 1968 to 2006. J Am Acad Dermatol. 2009; 61(3):426–432.
6. Berwick M, Begg CB, Armstrong BK, et al. Interaction of CDKN2A and sun exposure in the etiology of melanoma in the general population. J Invest Dermatol. 2011; 131(12):2500–2503.
7. Reed JA, Shea CR. Lentigo maligna: melanoma in situ on chronically sun-damaged skin. Arch Pathol Lab Med. 2011; 135(7):838–841.
8. Waster P, Rosdahl I, Gilmore BF, Seifert O. Ultraviolet exposure of melanoma cells induces fibroblast activation protein-α in fibroblasts: implications for melanoma invasion. Int J Oncol. 2011; 39(1):193–202.
9. Bae JM, Kim HO, Park YM. Progression from acral lentiginous melanoma in situ to invasive acral lentiginous melanoma. Ann Dermatol. 2009; 21(2):185–188.
10. Balch CM, Gershenwald JE, Soong SJ, et al. Final version of 2009 AJCC melanoma staging and classification. J Clin Oncol. 2009; 27(36):6199–6206.
11. Bellew S, Del Rosso JQ, Kim GK. Skin cancer in asians: part 2: melanoma. J Clin Aesthet Dermatol. 2009; 2(10):34–36.
12. Lee MW, Koh JK, Kwon KS, et al. Clinical and histopathological study of cutaneous melanoma in Korea. Korean J Dermatol. 2003; 41(1):43–47.
13. Moon SE, Cho KH, Hwang JH, Kim JA, Youn JI. A statistical study of cutaneous malignant tumors. Korean J Dermatol. 1998; 36(1):7–15.
14. Ries LA, Wingo PA, Miller DS, et al. The annual report to the nation on the status of cancer, 1973-1997, with a special section on colorectal cancer. Cancer. 2000; 88(10):2398–2424.
15. Takematsu H, Obata M, Tomita Y, Kato T, Takahashi M, Abe R. Subungual melanoma: a clinicopathologic study of 16 Japanese cases. Cancer. 1985; 55(11):2725–2731.
16. Collins RJ. Melanoma in the Chinese of Hong Kong: emphasis on volar and subungual sites. Cancer. 1984; 54(7):1482–1488.
17. Park KG, Blessing K, Kernohan NM. Surgical aspects of subungual malignant melanomas: the Scottish Melanoma Group. Ann Surg. 1992; 216(6):692–695.
18. Blessing K, Kernohan NM, Park KG. Subungual malignant melanoma: clinicopathological features of 100 cases. Histopathology. 1991; 19(5):425–429.
19. Slingluff CL Jr, Vollmer R, Seigler HF. Acral melanoma: a review of 185 patients with identification of prognostic variables. J Surg Oncol. 1990; 45(2):91–98.
20. Balch CM, Murad TM, Soong SJ, Ingalls AL, Richards PC, Maddox WA. Tumor thickness as a guide to surgical management of clinical stage I melanoma patients. Cancer. 1979; 43(3):883–888.
21. Balch CM, Soong SJ, Milton GW, et al. A comparison of prognostic factors and surgical results in 1,786 patients with localized (stage I) melanoma treated in Alabama, USA, and New South Wales, Australia. Ann Surg. 1982; 196(6):677–684.
22. Pack GT, Oropeza R. Subungual melanoma. Surg Gynecol Obstet. 1967; 124(3):571–582.
23. Papachristou DN, Fortner JG. Melanoma arising under the nail. J Surg Oncol. 1982; 21(4):219–222.
24. Muchmore JH, Krementz ET, Carter RD, Sutherland CM, Godfrey RS. Regional perfusion for the treatment of subungual melanoma. Am Surg. 1990; 56(2):114–118.
25. Baas PC, Hoekstra HJ, Schraffordt Koops H, Oosterhuis JW, Oldhoff J. Isolated regional perfusion in the treatment of subungual melanoma. Arch Surg. 1989; 124(3):373–376.
26. Balch CM, Soong SJ, Gershenwald JE, et al. Prognostic factors analysis of 17,600 melanoma patients: validation of the American Joint Committee on Cancer melanoma staging system. J Clin Oncol. 2001; 19(16):3622–3634.
27. Barth A, Wanek LA, Morton DL. Prognostic factors in 1,521 melanoma patients with distant metastases. J Am Coll Surg. 1995; 181(3):193–201.
28. Leo F, Cagini L, Rocmans P, et al. Lung metastases from melanoma: when is surgical treatment warranted? Br J Cancer. 2000; 83(5):569–572.
29. Balch CM, Soong SJ, Atkins MB, et al. An evidence-based staging system for cutaneous melanoma. CA Cancer J Clin. 2004; 54(3):131–149.
30. Luk NM, Ho LC, Choi CL, Wong KH, Yu KH, Yeung WK. Clinicopathological features and prognostic factors of cutaneous melanoma among Hong Kong Chinese. Clin Exp Dermatol. 2004; 29(6):600–604.




 PDF
PDF ePub
ePub Citation
Citation Print
Print






 XML Download
XML Download