Abstract
Background
During ligament balancing for severe medial contracture in varus knee total knee arthroplasty (TKA), complete distal release of the medial collateral ligament (MCL) or a medial epicondylar osteotomy can be necessary if a large amount of correction is needed.
Methods
This study retrospectively reviewed 9 cases of complete distal release of the MCL and 11 cases of medial epicondylar osteotomy which were used to correct severe medial contracture. The mean follow-up periods were 46.5 months (range, 36 to 78 months) and 39.8 months (range, 32 to 65 months), respectively.
Results
There were no significant differences in the clinical results between the two groups. However, the valgus stress radiograph revealed significant differences in medial instability. In complete distal release of the MCL, some stability was obtained by repair and bracing but the medial instability could not be removed completely.
The acquisition of proper soft tissue balance is one of the crucial factors for preventing long-term failure and obtaining successful treatment outcomes of total knee arthroplasty (TKA).1) The soft tissue is composed of not only a pathological contracture of the medial soft tissue but also the attenuation or laxity of the lateral soft tissue in a varus knee due to degenerative arthritis. The medial release in TKA relaxes the medial soft tissue with a contracture in a sequential manner, thereby attempting to obtain a balance between the medial and lateral soft tissues.1-4)
Although there is a difference in medial release depending on the surgeon, it is a procedure where osteophytes are removed and the medial soft tissue is released in a stepwise manner. In some cases, complete distal release of the tibial attachment of the superficial medial collateral ligament (MCL) should be done during this phase.5-8)
Engh and McAuley9) introduced a balancing procedure for releasing the MCL from the femur by performing a medial epicondylar osteotomy. A medial epicondylar osteotomy can prevent medial instability due to complete conventional MCL stripping. The proximal to distal continuity of the MCL and adductor magnus tendon provides knee stability.10,11)
This study compared retrospectively the results of complete distal release of the MCL with those of medial epicondylar osteotomy during ligament balancing in varus knee TKA.
A total of 290 cases (217 patients) underwent TKA between February 2001 and December 2006. Of those, nine patients (3.1%) who underwent complete distal release of the superficial MCL were assigned to group 1 (n = 9) and 11 patients (3.8%) who underwent a medial epicondylar osteotomy were assigned to group 2 (n = 11). The surgical indications for both groups were not differentiated and we used both techniques in cases with residual medial contracture after sequential release until the posterior capsule was released. However, there was a timing difference between these techniques.
We used distal release of the superficial MCL in the early period of this study and changed the surgical technique to medial epicondylar osteotomy in the latter part of the study period. In group 1, one case of lower limb paralysis, which occurred due to a spinal injury during the follow-up observation, was excluded. Retrospective analysis was performed in these two groups. The mean age in groups 1 and 2 was 71.1 years (range, 60 to 81 years) and 71.5 years (range, 53 to 83 years), respectively. The mean follow-up period in groups 1 and 2 was 46.5 months (range, 36 to 78 months) and 39.8 months (range, 32 to 65 months), respectively. In both groups, all cases were women. In group 1, the underlying diseases included seven cases of degenerative arthritis and one case of rheumatoid arthritis. In group 2, the underlying diseases included ten cases of degenerative arthritis and one case of rheumatoid arthritis. In group 1, the type of prosthesis was cruciate-retaining in one case (Advantim Knee, Wright Medical Technology, Arlington, TN, USA), posterior-sacrificing in five cases (Advantim Knee), and medial-pivot knee in two cases (Advance Medial-Pivot Knees, Wright Medical Technology). In group 2, a posterior-stabilized prosthesis was used in all cases (10 Advantim Knee; 1 Nexgen LPS, Zimmer, Warsaw, IN, USA). In group 1, the detached MCL was repaired underneath the pes anserinus using Vicryl No.1 (Ethicon, Somerville, NJ, USA) sutures.12)
In group 2, the fragment which had detached from the medial femoral epicondyle was sutured and fixed with Ethibond No.5 (Ethicon) to prevent posterior displacement of the fragment during knee flexion. Both groups had the same rehabilitation protocol after surgery, and an MCL brace was applied to both groups and range of motion (ROM) exercises were started as tolerated. The MCL brace was removed 3 months after surgery. The clinical assessment was based on the American Knee Society knee score (KS), function score (FS), and the ROM preoperatively and at the final follow-up. For the radiological assessment, the femorotibial angle was measured based on the whole lower extremity radiograph preoperatively and at the final follow-up. Three months after surgery and at the final follow-up, medial instability was assessed using the valgus stress radiographs, in which the contralateral side was compared using Telos (Telos, Weterstadt, Germany). The patients were placed in the supine position and then relaxed. A valgus force of 150 N in magnitude was then applied to the knee joint, and the joint was flexed at between 0° and 20°. In all cases, one observer measured the radiology results to reduce the interobserver variations.
The outcomes preoperatively and at the final follow-up or at three months after surgery and at the final follow-up were compared using a Wilcoxon signed ranks test (pw). The outcome in groups 1 and 2 was compared using a Mann-Whitney U-test (pM). A p-value < 0.05 was considered significant.
The clinical outcomes in groups 1 and 2 were compared. In group 1, the KS was 31.9 ± 16.3 points and 95.1 ± 3.0 points preoperatively and at the final follow-up, respectively (pw = 0.012). In group 2, the KS was 35.9 ± 12.9 points and 91.1 ± 4.4 points preoperatively and at the final follow-up, respectively (pw = 0.003). In group 1, the FS was 33.1 ± 19.6 points and 82.5 ± 8.9 points preoperatively and at the final follow-up, respectively (pw = 0.012). In group 2, the FS was 33.6 ± 14.5 points and 88.2 ± 8.7 points preoperatively and at the final follow-up, respectively (pw = 0.003). In group 1, the flexion contracture was 13.8° ± 9.5° and 0.6° ± 1.8° preoperatively and at the final follow-up, respectively (pw = 0.018). The maximal flexion was 96.3° ± 13.0° and 118.8° ± 11.3° preoperatively and at the final follow-up, respectively (pw = 0.023). In group 2, the flexion contracture was 11.8° ± 8.7° and 0.8° ± 1.5° preoperatively and at the final follow-up, respectively (pw = 0.005). The maximal flexion was 103.6° ± 19.0° and 119.1° ± 13.0° preoperatively and at the final follow-up, respectively (pw = 0.007). The clinical results such as the KS, FS, and ROM were similar in the two groups (pM = 0.301, pM = 0.479, pM = 0.965).
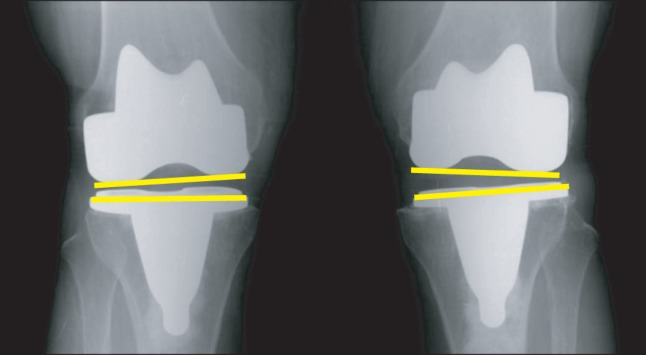
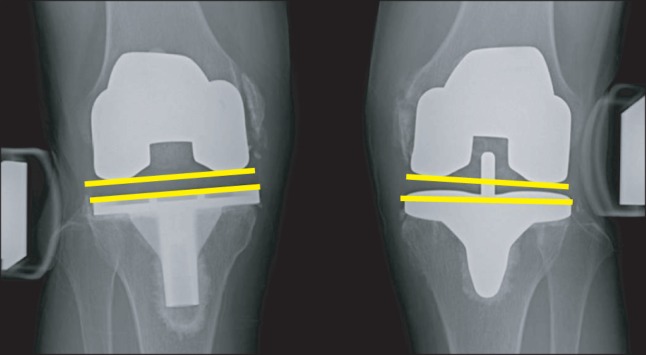
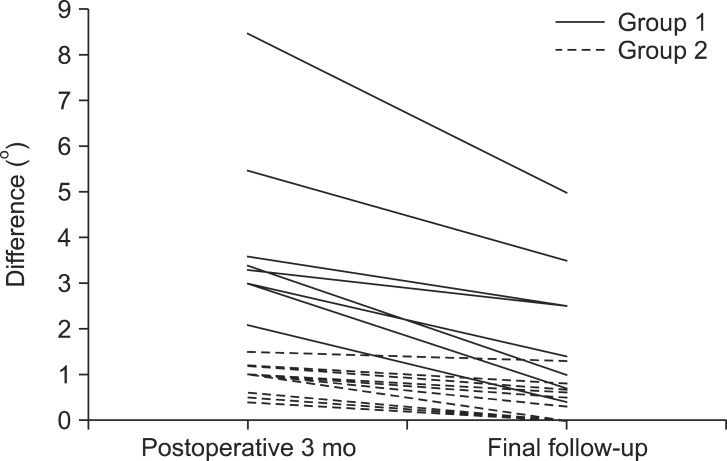
The radiological outcomes in groups 1 and 2 were compared. In group 1, the mean femorotibial angle was varus 12.8° ± 7.1° preoperatively, which was corrected to valgus 5.3° ± 1.0° at the final follow-up (pw = 0.036). In group 2, the mean femorotibial angle was varus 11.0° ± 3.8° preoperatively, which was corrected to valgus 5.9° ± 0.8° at the final follow-up (pw = 0.006). There were no significant differences between the two groups (pM = 0.160). On the valgus stress radiograph compared with the contralateral side, the difference in group 1 was 4.1° ± 2.0° at postoperative three months and 2.1° ± 1.6° at the final follow-up (pw = 0.012) (Fig. 1). In group 2, the difference was 0.9° ± 0.9° at three months and 0.4° ± 0.9° at the final follow-up (pw = 0.003) (Fig. 2). On the valgus stress radiograph, the medial stability was significantly higher in group 2 than group 1 (pM = 0.003) (Fig. 3). In group 2, seven and four cases showed bony union and fibrous union of the osteotomy site, respectively (Fig. 2). However, there were no significant differences in the degree of medial stability.
Obtaining a balance of soft tissue on the medial and lateral sides as well as a balance of soft tissue between extension and flexion is one of the critical factors that can affect the successful outcomes of TKA.1) In particular, the balance of soft tissue affects the long-term follow-up results of TKA, such as a satisfactory ROM and stability.13)
In medial release, the main structure is the superficial MCL which is a structure for which the greatest extent of the correction could be obtained.14,15) However, complete distal release of MCL has to be done at the tibial insertion if a large amount of correction is required.5-8)
Engh and McAuley9) proposed medial epicondylar osteotomy to prevent damage to the superficial MCL and obtain proper ligament balance. The osteotomy site includes the origin of the MCL and an insertion of the adductor magnus tendon. Therefore, the insertion of the adductor magnus tendon provides proximal stability to the osteotomized segment of the bone, which can maintain the continuity of the two structures while the knee is in extension. Dynamic stability of the medial structures can be provided by direct suturing of the osteotomy site and suturing of the medial retinaculum during flexion. Medial epicondylar osteotomy is advantageous in correcting the varus deformity on the coronal plane as well as flexion contracture on the sagittal plane. It is also useful for approaching severe contracture of the knee and revision TKA. Our study showed satisfactory clinical results without medial instability, too.
Conservative treatment or repair of the complete tibial detachment of the MCL is sufficient for treatment.5-8) Koo and Choi8) suggested that the intraoperative tibial detachment of the MCL does not require conversion to a constrained prosthesis, primary repair or fixation with advancement of the avulsed MCL, or postoperative application of a hinged knee brace, and can be healed favorably by conservative treatment. They reported only a 1° difference in the valgus stress angle between the MCL-intact side and MCL-off contralateral side, which might be too low to cause significant clinical instability. Leopold et al.6) reported no instability on the clinical and physical assessment after treatment with suture-anchor reattachment to the bone in four cases (0.7%). Mullaji et al.7) also reported that the distal end of a completely detached MCL was sutured to the pes insertion in two cases (1.2%).
These patients had no complaints of instability, but valgus stressing revealed minimal laxity. In this study, there were no complaints of clinical instability in the cases in which the superficial MCL was completely detached. However, the valgus stress radiograph, which was compared with the contralateral side, revealed a significant difference.
This medial instability can produce the lift-off phenomenon mentioned by Dennis et al.,16) which induces eccentric polyethylene wear. The amount of erosion increases with increasing frequency of the lift-off phenomenon. From the long-term aspect, it can lead to failure of the TKA due to several factors, such as premature loosening.17)
Several factors are considered as limitations of this study. First, the small number of enrolled cases can limit the power value of this study. Second, the follow-up duration was different between the two groups. Third, the type of implant was not the same between the groups and this difference may affect the outcome of mechanical stability. Fourth, fibrous union was observed in several cases and a more secure fixation device might offer a better chance for solid bony union. Fifth, the contralateral limb which was used as the control side had undergone TKA. Although ligament balancing of the contralateral limb was performed, including performance of conventional medial capsular release, and did not show a medial joint opening of more than 3 mm on the valgus stress radiogram, the contralateral limb was not a normal joint.
Our study showed that medial instability could not be removed completely in the complete MCL distal release group. Medial epicondylar osteotomy for a varus deformity in TKA could provide constant medial stability and be a useful ligament balancing technique.
References
1. Bottros J, Gad B, Krebs V, Barsoum WK. Gap balancing in total knee arthroplasty. J Arthroplasty. 2006; 21(4 Suppl 1):11–15. PMID: 16781420.

2. Yagishita K, Muneta T, Ikeda H. Step-by-step measurements of soft tissue balancing during total knee arthroplasty for patients with varus knees. J Arthroplasty. 2003; 18(3):313–320. PMID: 12728423.

3. Matsueda M, Gengerke TR, Murphy M, Lew WD, Gustilo RB. Soft tissue release in total knee arthroplasty: cadaver study using knees without deformities. Clin Orthop Relat Res. 1999; (366):264–273. PMID: 10627744.
4. Insall JN, Easley ME. Surgical techniques and instrumentation in total knee arthroplasty. In : Insall JN, Scott WN, editors. Surgery of the knee. 3rd ed. NewYork: Churchill Livingstone;2001. p. 1553–1620.
5. Teeny SM, Krackow KA, Hungerford DS, Jones M. Primary total knee arthroplasty in patients with severe varus deformity: a comparative study. Clin Orthop Relat Res. 1991; (273):19–31. PMID: 1959270.
6. Leopold SS, McStay C, Klafeta K, Jacobs JJ, Berger RA, Rosenberg AG. Primary repair of intraoperative disruption of the medical collateral ligament during total knee arthroplasty. J Bone Joint Surg Am. 2001; 83(1):86–91. PMID: 11205863.
7. Mullaji AB, Padmanabhan V, Jindal G. Total knee arthroplasty for profound varus deformity: technique and radiological results in 173 knees with varus of more than 20 degrees. J Arthroplasty. 2005; 20(5):550–561. PMID: 16309988.
8. Koo MH, Choi CH. Conservative treatment for the intraoperative detachment of medial collateral ligament from the tibial attachment site during primary total knee arthroplasty. J Arthroplasty. 2009; 24(8):1249–1253. PMID: 19640671.

9. Engh GA, McAuley JP. Joint line restoration and flexion extension balance with revision total knee arthroplasty. In : Engh GA, Rorabeck CH, editors. Revision total knee arthroplasty. Baltimore: Williams & Wilkins;1997. p. 235–252.
10. Engh GA, Ammeen D. Results of total knee arthroplasty with medial epicondylar osteotomy to correct varus deformity. Clin Orthop Relat Res. 1999; (367):141–148. PMID: 10546608.

11. Engh GA. The difficult knee: severe varus and valgus. Clin Orthop Relat Res. 2003; (416):58–63. PMID: 14646739.
12. Sim JA, Lee BK, Kwak JH, Yang SH. The clinical relationship between MCL complete detachment and mechanical alignment in TKA. J Korean Knee Soc. 2007; 19(1):38–43.
13. Matsuda Y, Ishii Y, Noguchi H, Ishii R. Varus-valgus balance and range of movement after total knee arthroplasty. J Bone Joint Surg Br. 2005; 87(6):804–808. PMID: 15911663.

14. Krackow KA, Mihalko WM. The effect of medial release on flexion and extension gaps in cadaveric knees: implications for soft-tissue balancing in total knee arthroplasty. Am J Knee Surg. 1999; 12(4):222–228. PMID: 10626913.
15. Mullaji A, Sharma A, Marawar S, Kanna R. Quantification of effect of sequential posteromedial release on flexion and extension gaps: a computer-assisted study in cadaveric knees. J Arthroplasty. 2009; 24(5):795–805. PMID: 18534536.
16. Dennis DA, Komistek RD, Walker SA, Cheal EJ, Stiehl JB. Femoral condylar lift-off in vivo in total knee arthroplasty. J Bone Joint Surg Br. 2001; 83(1):33–39. PMID: 11245535.

17. Jennings LM, Bell CI, Ingham E, Komistek RD, Stone MH, Fisher J. The influence of femoral condylar lift-off on the wear of artificial knee joints. Proc Inst Mech Eng H. 2007; 221(3):305–314. PMID: 17539585.





 PDF
PDF ePub
ePub Citation
Citation Print
Print


 XML Download
XML Download