Abstract
Placing instrumentation into the ilium has been shown to increase the biomechanical stability and the fusion rates, but it has some disadvantages. The diagonal S2 screw technique is an attractive surgical procedure for degenerative lumbar deformity. Between 2008 and 2010, we carried out long fusion across the lumbosacral junction in 13 patients with a degenerative lumbar deformity using the diagonal S2 screws. In 12 of these 13 patients, the lumbosacral fusion was graded as solid fusion with obvious bridging bone (92%). One patient had a rod dislodge at one S2 screw and breakage of one S1 screw and underwent revision nine months postoperatively. So, we present alternative method of lumbopelvic fixation for long fusion in degenerative lumbar deformity using diagonal S2 screw instead of iliac screw.
Placing instrumentation into the ilium or sacrum as an adjunct to S1 pedicle screws has been shown to increase the biomechanical stability of lumbosacral constructs, and high fusion rates have been reported.1,2) However, iliac fixation can require separate fascial or skin incisions or the use of offset connectors.3,4) We report an alternative method of lumbopelvic fixation to address some of these drawbacks called the diagonal S2 screw technique.
The ability to place a diagonal S2 screw requires a thorough understanding of each individual patient's anatomy. Standing anteroposterior and lateral lumbar radiographs and an anteroposterior pelvic radiograph should be obtained. The overall alignment of the spine and pelvis in deformity the coronal and sagittal plane should be evaluated carefully. Preoperative computerized tomography (CT) should be performed to evaluate for absent or small pedicles and congenital and other bony abnormalities. Depending on the experience, skill, and comfort of the operating surgeon, intraoperative fluoroscopy is recommended but not required.
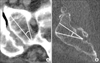
The affected area is first exposed through the posterior midline approach followed by lateral dissection as far as the transverse process. The lower medial edge of the S1 dorsal foramen and the upper medial edge of the S2 dorsal foramen was carefully exposed (Fig. 1). The entry point is on the junction of the midlines of the foramen and the bone arch between them. After choosing the entry point, marking the entry point with a small sharp owl. And confirm the trajectory to the anterior cortex with a straight probe.
The probe was angled laterally 30 to 35 degrees, and tilted cephalad 15 to 20 degrees (Fig. 2). The probe was passed through three-dimensional line to percuss the anterior cortex. On touching the cortex, the depth was measured, then 10 mm was added to the cortical thickness itself. The probe was inserted along the cortex with a mallet. It's important that maintain the probe exact trajectory to the anterior cortex hole. The probe was reinserted along the anterior cortex to assure the exact trajectory of the S2 6.0-mm-diameter screw. An attempt was then made to place the screw with the tip contacting the triangular area of cortical bone at the anterior, inferior, and lateral boundaries of the sacral ala without penetrating through these boundaries. Lateral penetration of the screw will violate the sacroiliac joint, which could result in painful arthropathy. Significant anterior penetration in this area can result in impingement of the L5 nerve root, which runs anterior to the sacrum in this area.
A portable lateral radiograph was used to confirm the exact angle in the sagittal plane. Owing to the curve of the pelvic iliopectineal line, the screw tip projected 10 to 20 mm in front of the S1 anterior cortex on the lateral radiograph. Subsequently, a 6.0-mm-diameter, 50-mm-long variable angle screw was inserted. Posterolateral fusion was accomplished using autogenous iliac bone harvested from the posterior iliac crest and with a local autograft obtained from the spinous processes of the lumbar spine, bone removed from the partial facetectomy and laminectomy. Finally, rods were applied to the pedicle screws and the screws were tightened to apply the compressive load to the bone graft.
Between 2008 and 2010, we carried out long fusion(more than 4 segments) across the lumbosacral junction in 13 patients with a degenerative lumbar deformity using the operative technique described. All procedures were performed by a single surgeon. The mean patient age at the time of the operation was 71.4 years (range, 61 to 79 years), and the mean follow-up period was 26.6 months (range, 12.9 to 40.24 months). The mean fusion level was 4.7 levels (range, 4 to 8 levels) (Table 1).
All 13 patients were evaluated with postoperative CT scans that were performed no sooner than six months postoperatively. In 12 of these 13 patients, the lumbosacral fusion was graded by an independent radiologist as solid fusion with obvious bridging bone (Fig. 3). The one patient who did not have solid fusion remained greatly improved in terms of her back pain compared with before surgery and did not have any symptoms consistent with pseudarthrosis. There were no complications that occurred as a result of the diagonal S2 screw placement during the follow-up period.
One patient was a farmer and insisted upon maintaining her rural life and farming work. She had a rod dislodge at one S2 screw and breakage of one S1 screw resulting in kyphotic deformity two months postoperatively. As a result, this patient did experience painful hardware prominence of the dislodged rod requiring removal, and underwent revision of the T10-S1 fusion nine months postoperatively.
Achieving solid fusion at the lumbosacral junction in deformity surgery is challenging.5) As is often the case, osteopenia at S1 limits the quality of fixation there; thus, only one level of fixation anchors the construct solidly at the lumbosacral junction. Using just the S1 promontory fixation in adult deformity surgery is associated with pseudarthrosis at L5-S1.6) The high incidence of pseudarthrosis at the lumbosacral junction has led authors to recommend anterior interbody fusion and supplemental fixation at the lumbosacral junction6,7) as a part of complete lumbosacral fixation.3,6)
The major advantage in sacral-pelvic fixation is the assembly the instrumented fusion segment to the ilium. There are two fundamental fixation techniques for instrumentation of lumbosacral junction-all sacral fixation and sacro-iliac fixation. The difference between these two techniques is S2 screw fixation versus iliac screw fixation.
The iliac screw fixation technique is insertion of fully- or partially-threaded iliac screws and connected with the longitudinal rod in the lumbar spine through monoaxial or polyaxial connectors and offsets. The advantage of iliac screw system is modularity, easier placement of implants, placement of more than one iliac screw on each side, and biomechanical compatibility with a proper pivot point.2) However, iliac screw fixation technique has potential risk of substantial morbidity. The technique has higher risk of infection and bleeding because of extensive surgical exposure and poor soft tissue coverage.
More practically, the iliac implants may be prominent and interfere with iliac graft harvest. In addition, there are other complications associated with iliac screw fixation including loosening, injury of neurovascular structures in the sciatic notch, violation of acetabulum, and hardware prominence.1,8) Furthermore, Kuklo et al.1) reported an infection rate of 4% associated with lumbosacral fusion using bilateral S1 and iliac screws. The sacral alar screw has been used as an alternative to the iliac screw and has been tested biomechanically. Leong et al.9) found that a construct consisting of bicortical S1 pedicle screws in combination with bicortical S2 alar screws that were inserted 30 degrees anterolaterally was significantly stronger than constructs using bicortical S1 pedicle screws alone. In a study by Zindrick et al.,10) second sacral pedicle is weakest location and screws aimed laterally into the ala at 45 degrees resist larger axial pull-put loads than straight anteriorly into the ala. But, diagonal insertion of S2 screw did not tested and S2 screw is not embedded firmly than iliac screw.
To overcome the iliac screw disadvantages, the diagonal S2 screw for lumbo-sacral fixation was described here. The diagonal S2 screw has many potential advantages compared with iliac screw fixation such as a lower profile, avoidance of extra soft tissue dissection, no competition with iliac bone graft harvest, and easier salvage if ever infected. But in patient with severe sagittal imbalance, authors thought iliac screw fixation is appropriate option for preventing pseudarthrosis.
Authors used a 6.0-mm-diameter, 50-mm-long variable angle screw in most of the patients and it was sufficient for solid lumbo-sacral fixation. More larger screw is able to provide greater stability, but further biomechanical testing would have to be accomplished to come to any firm conclusion regarding the strength of S2 screws. In our cases, a posterolateral fusion was performed in 13 patients and there was no interbody fusion case. Interbody fusion provides mechanical advantages in terms of graft compression and a large, well vascularized fusion surface. But, only posterolateral fusion with S2 screw fixation provided high fusion rate (12/13) and authors think interbody fusion doesn't need in our techniques.
Authors suggest that the S1-diagonal S2 screw construct is an appropriate alternative to the S1-iliac screw construct and it presents certain clinical advantages. However, the short- and long-term effects of the diagonal S2 screw have not been completely evaluated. Further data are needed to fully evaluate the diagonal S2 technique.
Figures and Tables
Fig. 1
Entry point of the S2 alar screw (arrow) and the midpoint of the line from the medial margin of the S1 dorsal foramen and the medial margin of the S2 dorsal foramen.

Fig. 2
(A) The lateral trajectory of the S2 alar screw varied somewhat among patients but was typically between 30 and 35 degrees in the lateral planes. It did not penetrate the sacroiliac joint laterally or the S1 ventral foramen medially. (B) The superior trajectory of the S2 alar screw was a longer screw insertion and did vary somewhat among patients, but was typically between 15 and 20 degrees in the superior planes. It did not penetrate the anterior cortex as this could cause impingement of the L5 nerve root and injury to the internal iliac vessels.
References
1. Kuklo TR, Bridwell KH, Lewis SJ, et al. Minimum 2-year analysis of sacropelvic fixation and L5-S1 fusion using S1 and iliac screws. Spine (Phila Pa 1976). 2001; 26(18):1976–1983.

2. McCord DH, Cunningham BW, Shono Y, Myers JJ, McAfee PC. Biomechanical analysis of lumbosacral fixation. Spine (Phila Pa 1976). 1992; 17:8 Suppl. S235–S243.

3. Lebwohl NH, Cunningham BW, Dmitriev A, et al. Biomechanical comparison of lumbosacral fixation techniques in a calf spine model. Spine (Phila Pa 1976). 2002; 27(21):2312–2320.

4. Tsuchiya K, Bridwell KH, Kuklo TR, Lenke LG, Baldus C. Minimum 5-year analysis of L5-S1 fusion using sacropelvic fixation (bilateral S1 and iliac screws) for spinal deformity. Spine (Phila Pa 1976). 2006; 31(3):303–308.

5. Ahn DK, Park HS, Choi DJ, Kim KS, Yang SJ. Survival and prognostic analysis of adjacent segments after spinal fusion. Clin Orthop Surg. 2010; 2(3):140–147.

6. Edwards CC 2nd, Bridwell KH, Patel A, Rinella AS, Berra A, Lenke LG. Long adult deformity fusions to L5 and the sacrum: a matched cohort analysis. Spine (Phila Pa 1976). 2004; 29(18):1996–2005.

7. Kim YJ, Bridwell KH, Lenke LG, Cho KJ, Edwards CC 2nd, Rinella AS. Pseudarthrosis in adult spinal deformity following multisegmental instrumentation and arthrodesis. J Bone Joint Surg Am. 2006; 88(4):721–728.

8. Moshirfar A, Rand FF, Sponseller PD, et al. Pelvic fixation in spine surgery: historical overview, indications, biomechanical relevance, and current techniques. J Bone Joint Surg Am. 2005; 87:Suppl 2. 89–106.




 PDF
PDF ePub
ePub Citation
Citation Print
Print




 XML Download
XML Download