Abstract
Background
Dynamic radiographs are recommended to investigate non-healing evidence such as the dynamic mobility or intravertebral clefts in osteoporotic vertebral compression fractures (VCFs). However, it is difficult to examine standing flexion and extension lateral radiographs due to severe pain. The use of prone cross-table lateral radiographs (PrLRs) as a diagnostic tool has never been proposed to our knowledge. The purpose of this study is to clarify the usefulness of PrLRs in diagnosis and treatment of VCFs.
Methods
We reviewed 62 VCF patients examined with PrLRs between January 1, 2008 and June 30, 2011. To compare the degree of pain provoked between standing extension lateral radiographs (StLRs) and PrLRs, numeric rating scale (NRS) scores were assessed and compared by a paired t-test. Vertebroplasty was done for 40 patients and kyphoplasty was done for 9 patients with routine manners. To assess the degree of postural reduction, vertebral wedge angles (VWA) and vertebral height ratios (VHR) were calculated by using preoperative StLRs, PrLRs, and postoperative lateral radiographs. Two variables derived from changes in VWA and VHR between preoperative and postoperative radiographs were compared by a paired t-test.
Results
The average NRS scores were 6.23 ± 1.67 in StLRs and 5.18 ± 1.47 in PrLRs. The degree of pain provocation was lower in using PrLRs than StLRs (p < 0.001). The average changes of VWA between preoperative and postoperative status were 5.24° ± 6.16° with PrLRs and 3.46° ± 3.47° with StLRs. The average changes of VHR were 0.248 ± 0.178 with PrLRs and 0.148 ± 0.161 with StLRs. The comparisons by two variables showed significant differences for both parameters (p = 0.021 and p < 0.001, respectively). The postoperative radiological status was reflected more precisely when using PrLRs than StLRs.
Conclusions
In comparison with StLR, the PrLR was more accurate in predicting the degree of restoration of postoperative vertebral heights and wedge angles, and provoked less pain during examination. The PrLR could be a useful diagnostic tool to detect intravertebral cleft or intravertebral dynamic instability.
Vertebral compression fractures (VCFs) are relatively common among the elderly with osteoporosis. However, the diagnosis of compression fractures is sometimes not easy with plain radiographs and selecting a proper treatment option is somewhat difficult.
In acute VCFs, conservative management including pain medication or immobilization with braces has been considered to be a first-line treatment option. The pain from acute VCFs is usually alleviated significantly with conservative therapy. However, a number of patients still have severe pain after several months. Klazen et al.1) showed a third of patients still had severe pain, necessitating pain medication and physical therapy 2 years after the onset of acute VCFs. In some cases, surgical treatment may be helpful for patients with long-standing back pain. Dynamic mobility or intravertebral clefts shown in plain radiographs are included in those cases. Dynamic mobility means delay of fracture healing, which eventually progresses to nonunion or so called Kummell's disease.2) It has been known that the chances of union declined when there were intravertebral clefts.3) Therefore, it is important to investigate the evidence of dynamic mobility, and dynamic radiographs have been recommended as a first-line radiographic tool for suspicious cases.
However, it is difficult to examine standing flexion and extension lateral radiographs in cases of VCFs because the patients cannot follow the exact position due to severe pain. The possible aggravation of collapse during the examination is another problem. In this regard, McKiernan et al.4) suggested the usefulness of supine cross-table lateral radiographs (SuLRs) and recommended examination for evaluating dynamic mobility. Several authors followed these methods and confirmed its usefulness.5,6) However, there are several problems in the methods including possible pain stimulations and different positions with real operative settings.
For this reason, the authors examined prone cross-table lateral radiographs (PrLRs) instead of SuLRs. The use of PrLRs in VCFs as a diagnostic tool for dynamic instability has never been proposed to our knowledge. Our aim was to clarify the usefulness of PrLRs in diagnosis and treatment planning of VCFs with dynamic instability.
This study was a retrospective case series and was approved by our Institutional Review Board. We reviewed 62 compression fracture patients examined by PrLRs and standing extension lateral radiographs (StLRs) between January 1, 2008 and June 30, 2011. Inclusion and exclusion criteria were as follows. The compression fracture patients with minor trauma such as slip down or coughing were included. The inclusive cases were limited to one or two non-contiguous fractures which were examined by PrLRs to assess dynamic mobility or intravertebral clefts. In cases where the quality of film was not good enough to measure, it was excluded (1 case). Two or more level compression fractures which were contiguous were also excluded because the vertebral height ratio (VHR) could not be measured (8 cases).
The fractures were classified by time periods from onset. Acute fractures were defined as those having fewer than 3 months of symptom durations; and chronic fractures were defined as those having 3 or more months of symptom durations. The reason the authors selected 3 months as a criteria was that the duration of normal healing process was about 3 months and several reports adopted 3 to 4 months as a practical standard to classify.7,8) Forty-five cases (49 levels) were acute and 17 cases (18 levels) were chronic. Demographic data including age, gender, diagnosis and treatment protocols were obtained from electronic medical records. The degrees of osteoporosis derived from dual energy X-ray absorptiometry (DEXA; Lunar Prodigy Advance, GE Healthcare, Milwaukee, WI, US) scores.
All patients were initially treated conservatively, which included bracing with Thoracolumbosacral orthosis (TLSO) or Knight-Taylor orthosisin acute cases, and pain medications in both acute and chronic cases. If symptoms were not alleviated after 2 to 3 weeks of conservative therapy, the authors then considered whether surgical treatments would be helpful and which surgical options would be better. However, the authors usually performed vertebroplasty whenever there was evidence of postural reduction. If the degree of re-expansion was insufficient, kyphoplasty became the choice.
To compare the degree of pain provoked between StLRs and PrLRs, numeric rating scale (NRS) scores were checked and compared with a paired t-test. PrLRs were checked in natural prone positions in a flat table without pillows, which was completely the same with real operative status (Fig. 1). Vertebroplasty or kyphoplasty was done with routine manners on a flat operation table and in the prone position.
To assess the degree of postural reduction by prone position, preoperative StLRs, PrLRs, and postoperative lateral radiographs were used for analysis. The target cases for radiologic evaluation on the degree of postural reduction between PrLRs and StLRs were limited to the patients who underwent vertebroplasty because there was concern that the degree of reduction was exaggerated if kyphoplasty cases were included. Radiological parameters were measured individually by using picture archiving and communication system (PACS; Infinitt Co., Seoul, Korea): vertebral wedge angle (VWA) was defined by the angle between upper endplate and lower endplate of involved vertebra, and VHR was calculated as the vertebral height of middle column in the fractured vertebra divided by the average of vertebral of middle column at one level above and below the fractured vertebra to adjust magnification errors of vertebral height (Fig. 2).9) The differences of VWA between postoperative lateral radiographs and preoperative StLRs were calculated and marked as VWA_1. The differences in VWA between postoperative lateral radiographs and preoperative PrLRs were calculated and marked as VWA_2. In the same way, VHR_1 and VHR_2 were calculated. To assess each preoperative radiograph's degree of reflection to postoperative status, a paired t-test was used between VWA_1 and VWA_2. In the same way, comparison between VHR_1 and VHR_2 was done, respectively.
To compare the predictability of postoperative radiologic status between vertebroplasty and kyphoplasty, student t-test was done using VWA_2 and VHR_2. Statistical significance was defined as p-value <0.05.
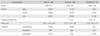
The average age was 73.9 ± 8.3 years old. The symptom duration was 1.1 ± 0.3 months in acute cases and 10.9 ± 1.9 months in chronic cases. The average DEXA score was -2.44 ± 1.15. The demographic features including gender distributions and treatment protocols are described in Table 1. The most commonly involved level was L1 (20 cases) followed by T12 (18 cases). The number of acute VCF patients who were operated on was 42 (10 male and 32 female). The other 3 acute VCF patients were reluctant to undergo operations so they were continued to be managed conservatively. Vertebroplasty was done in 36 patients (40 levels) and kyphoplasty was done in 6 patients (6 levels).
The average NRS score in StLRs was 6.23 ± 1.67. The average NRS score in PrLRs was 5.18 ± 1.47. The degree of pain provocation was lower in PrLRs than in StLRs and the difference was statistically significant (p < 0.001).
The mean and standard deviation of measured VWA and VHR in patients who underwent vertebroplasty are summarized in Table 2. The mean of VWA_1 was 5.24 ± 6.16° and that of VWA_2 was 3.46 ± 3.47°. There was a significant difference between VWA_1 and VWA_2 by paired t-test (p = 0.021). In the same way, the means of VHR_1 and VHR_2 were calculated. The comparisons between VHR_1 and VHR_2 are shown in Table 2 and it revealed significant difference (p < 0.001).
The VWA_2 was 3.36° ± 3.65° in vertebroplasty group and 7.58° ± 4.09° in kyphoplasty group. The difference between each group was statistically significant (p = 0.015). The VHR_2 in vertebroplasty group was 0.150 ± 0.161 and that in kyphoplasty group was 0.156 ± 0.110. The differences between them was not statistically significant (p = 0.930).
Our results showed less pain provocation in prone positions than standing extension positions. Furthermore, preoperative PrLRs reflected the degrees of reduction more precisely than preoperative StLRs. In VCF patients, proper flexion and extension of lateral films are difficult to obtain due to severe pain. In addition, the risk of further collapse during the flexion and extension positions is also a limitation of standing dynamic radiographs. Thus, there have been several reports on the usefulness of SuLRs as an alternative. McKiernan et al.4) showed dynamic mobility in 44% of 41 patients who underwent vertebroplasty to compare preoperative standing lateral radiographs and SuLRs. Following these methods, two other reports were published; one showed the value of sitting and supine with bolster lateral radiographs in painful osteoporotic VCFs.5) The other evaluated the efficacy of SuLRs to detect intravertebral clefts and assess dynamic mobility in osteoporotic VCFs.6) All authors proposed that SuLRs were effective at showing dynamic mobility and helped to decide whether to operate without further evaluations like the MRI.
However, there are several problems not being mentioned. First, they frequently used bolsters (pillows) under the patient's back to stretch the compressed vertebral body. However, this maneuver may aggravate back pain because excessive stretching could stimulate pain by motion of fractured vertebral body. The fact that the supine position cannot reflect a real operative position, which is prone, is also one of their limitations.
In this regard, we examined the PrLRs preoperatively. Using this protocol, it was relatively easy to position patients without severe back pain. This was supported by our assessment of pain through the checking radiographs. Furthermore, it was evident that PrLRs reflect postoperative radiological status more precisely than StLRs according to our results. Authors considered the prone positioning as being more preferable to predict radiological outcome which is the reason for checking radiographs under the same operative positions.
PrLRs have several advantages in the decision-making process for VCFs. Firstly, if dynamic mobility of fractured vertebral bodies or intravertebral clefts existed in those radiographs, vertebroplasty or kyphoplasty can be demonstrated because those lesions are considered to be highly probable pain origins. Secondly, they could help in deciding whether to perform vertebroplasty or kyphoplasty. Both procedures can be used for painful osteoporotic VCF refractory to medical treatments.10) Although there were several reports on the comparison of clinical outcomes between percutaneous vertebroplasty and kyphoplasty,11-13) few reports discussed the differences in between them. Kyphoplasty can be performed in any case. However, pain provocations during the procedure and more junctional vertebral collapse have been known as the demerits of kyphoplasty.14) In this reason, vertebroplasty can be the option if the degree of postural reduction is satisfactory. Although the merits of kyphoplasty including the reduction of the risk of cement extrusion exist in that case, vertebroplasty could be sufficient to restore the height. However, if the degree of restoration is not enough, then kyphoplasty may be useful since it has been known to offer a higher degree of spinal deformity correction than vertebroplasty.12) In fact, the extent of postoperative vertebral height restoration would be different depending on the types of surgery. Because ballooning makes vertebral height to be more elevated, the difference of vertebral heights between preoperative and postoperative radiographs in kyphoplasty groups could be higher than that in vertebroplasty groups. However, our data indicated no differences in postoperative height restorations between two procedures even though the restoration of VWA was significantly higher in the kyphoplasty group. Thirdly, PrLRs can be helpful when searching for non-healing evidences in VCF patients with chronic back pain (Kummell disease). Intravertebral cleft owing to nonunion could be seen more definitely with this procedure. The example case was presented in Fig. 3. Brown et al.15) proposed that percutaneous vertebroplasty improved symptoms in 80% of their chronic VCF patients who had pain over 1 year. But, they did not mention the indications related to radiographic findings. In fact, our results did not support the association between postoperative results and the extent of fracture instability. However, PrLR could be considered as one diagnostic option for chronic VCF patients with back pain.
This study has some limitations. Firstly, our study is retrospective and the data related with follow-up were also insufficient, the authors could not evaluate the postoperative clinical courses including adjacent vertebral body fractures or recompressions.16,17) Secondly, sample size was relatively small, especially the numbers of patients who underwent kyphoplasty and who had chronic symptoms. Thirdly, because we used the severity of trauma as inclusion criteria, the degree of osteoporosis, which was measured in DEXA scores, was not to be considered as inclusion criteria. Fourthly, there will be problems relating to differences of patient positions in checking PrLRs. In fact, the authors thought there would not be so much variance because the films were checked in natural prone positions without pillows. However, there would be some chances of errors if the patients were obese or deformed. Unfortunately, appropriate correction methods for these situations could not be found. Finally, the parameters can vary depending on the fracture configuration. For example, the VHR would be estimated to be lower in concave type than in wedge type, and the wedge angle would be more meaningful for wedge type fractures. This is also the reason why both VHR and VWA were considered as degrees of compression.
Regardless of these limitations, this study was meaningful in the following aspects. This study demonstrated the new concept of PrLRs which were useful in VCFs with dynamic instability. Kyphoplasty can be performed with many reasons including safe height elevations without cement leakages. Furthermore, predictable postoperative status is only one of the factors for selecting the type of surgery. Considering the possible problems related to kyphoplasty, the vertebroplasty could be a considerable option under specific conditions. In addition, they also suggest whether operative treatments are helpful in chronic symptomatic VCFs. There appears to be less limitation with PrLRs than SuLRs. However, a prospective comparative study between the two examinations will be needed to reach a conclusion.
In comparison with StLR, the PrLR was more accurate in predicting the degree of restoration for postoperative vertebral heights and wedge angles even in vertebroplasty, which has less height elevation effects as compared with kyphoplasty, and showed less provoked pain during examination. PrLR could be the useful diagnostic tool to detect intravertebral cleft or intravertebral dynamic instability.
Figures and Tables
Fig. 1
The illustration of the diagnostic position for prone cross-table lateral radiographs (PrLR). The direction of arrow means trajectory of x-ray beam.

Fig. 2
The parameters and calculating method from lateral radiographs. VWA (vertebral wedge angle) = Cobb's angle between Line 1 and Line 2, VHR (vertebral height ratio) = a / (b + c) × 2.

Fig. 3
The illustration of intravertebral instability for T12 compression fracture in a 76-year-old man who suffered from back pain for 6 months. (A) A standing extension lateral radiograph showed severe compression fracture at T12 vertebra. (B) A prone cross-table lateral radiograph revealed a vacuum cleft (arrow) in the body and slight reduction of vertebral height. (C) Vertebroplasty was done and the pain was alleviated.

References
1. Klazen CA, Verhaar HJ, Lohle PN, et al. Clinical course of pain in acute osteoporotic vertebral compression fractures. J Vasc Interv Radiol. 2010; 21(9):1405–1409.

2. Freedman BA, Heller JG. Kummel disease: a not-so-rare complication of osteoporotic vertebral compression fractures. J Am Board Fam Med. 2009; 22(1):75–78.

3. McKiernan F, Faciszewski T. Intravertebral clefts in osteoporotic vertebral compression fractures. Arthritis Rheum. 2003; 48(5):1414–1419.

4. McKiernan F, Jensen R, Faciszewski T. The dynamic mobility of vertebral compression fractures. J Bone Miner Res. 2003; 18(1):24–29.

5. Wu MH, Huang TJ, Cheng CC, Li YY, Hsu RW. Role of the supine lateral radiograph of the spine in vertebroplasty for osteoporotic vertebral compression fracture: a prospective study. BMC Musculoskelet Disord. 2010; 11:164.

6. Chen YJ, Lo DF, Chang CH, Chen HT, Hsu HC. The value of dynamic radiographs in diagnosing painful vertebrae in osteoporotic compression fractures. AJNR Am J Neuroradiol. 2011; 32(1):121–124.

7. Crandall D, Slaughter D, Hankins PJ, Moore C, Jerman J. Acute versus chronic vertebral compression fractures treated with kyphoplasty: early results. Spine J. 2004; 4(4):418–424.

8. Erkan S, Ozalp TR, Yercan HS, Okcu G. Does timing matter in performing kyphoplasty? Acute versus chronic compression fractures. Acta Orthop Belg. 2009; 75(3):396–404.
9. McKiernan F, Faciszewski T, Jensen R. Reporting height restoration in vertebral compression fractures. Spine (Phila Pa 1976). 2003; 28(22):2517–2521.

10. Gangi A, Sabharwal T, Irani FG, et al. Quality assurance guidelines for percutaneous vertebroplasty. Cardiovasc Intervent Radiol. 2006; 29(2):173–178.

11. Eck JC, Nachtigall D, Humphreys SC, Hodges SD. Comparison of vertebroplasty and balloon kyphoplasty for treatment of vertebral compression fractures: a meta-analysis of the literature. Spine J. 2008; 8(3):488–497.

12. Li X, Yang H, Tang T, Qian Z, Chen L, Zhang Z. Comparison of kyphoplasty and vertebroplasty for treatment of painful osteoporotic vertebral compression fractures: twelve-month follow-up in a prospective nonrandomized comparative study. J Spinal Disord Tech. 2012; 25(3):142–149.

13. Mathis JM, Ortiz AO, Zoarski GH. Vertebroplasty versus kyphoplasty: a comparison and contrast. AJNR Am J Neuroradiol. 2004; 25(5):840–845.

14. Frankel BM, Monroe T, Wang C. Percutaneous vertebral augmentation: an elevation in adjacent-level fracture risk in kyphoplasty as compared with vertebroplasty. Spine J. 2007; 7(5):575–582.

15. Brown DB, Gilula LA, Sehgal M, Shimony JS. Treatment of chronic symptomatic vertebral compression fractures with percutaneous vertebroplasty. AJR Am J Roentgenol. 2004; 182(2):319–322.





 PDF
PDF ePub
ePub Citation
Citation Print
Print



 XML Download
XML Download