Abstract
Background
A two-stage revision remains as the "gold standard" treatment for chronically infected total knee arthroplasties.
Methods
Forty-five septic knee prostheses were revised with a minimum follow-up of 5 years. Static antibiotic-impregnated cement spacers were used in all cases. Intravenous antibiotics according to sensitivity test of the culture were applied during patients' hospital stay. Oral antibiotics were given for another 5 weeks. Second-stage surgery was undertaken after control of infection with normal erythrocyte sedimentation rate and C-reactive protein values. Extensile techniques were used if needed and metallic augments were employed for bone loss in 32 femoral and 29 tibial revisions.
Results
The average interval between the first-stage resection and reimplantation was 4.4 months. Significant improvement was obtained with respect to visual analog scale pain and clinical and functional scores, and infection was eradicated in 95.6% of cases following a two-stage revision total knee arthroplasty. Radiographic evaluation showed suitable alignment without signs of mechanical loosening.
Conclusions
This technique is a reasonable procedure to eradicate chronic infection in knee arthroplasty and provides proper functional and clinical results. However, it sometimes requires extensile surgical approaches that could imply arduous surgeries. Metallic augments with cementless stems available in most of the knee revision systems are a suitable alternative to handle bone deficiencies, avoiding the use of bone allografts with its complications.
Total knee replacement is a successful surgery in terms of pain relief and functional improvement in patients with arthritis of the knee.1) Many issues could affect the optimal result of knee replacement, but infection is probably the most dreaded complication. Infection after knee replacement is a devastating scene requiring long hospital stays, multiple surgeries and repeated outpatient appointments. Its incidence ranges from 1.1% to 12.4% and different therapeutic strategies are available to resolve this problem.2)
For chronically infected total knee arthroplasty (TKA), two-stage reimplantation, which was first advocated by Insall et al.,3) is still the gold standard treatment for long-lasting infections of TKA.4,5) The technique of placing an antibiotic-impregnated cement block after debridement and removal of the infected prostheses was first described by Cohen et al.6) We routinely employ this technique to our chronically infected cases and have gotten good results in terms of infection eradication.
The purpose of this report is to retrospectively assess our results with two-stage reimplantation and confirm that this procedure is the best option to manage chronically infected knee prosthesis. Methodology is the key in verifying prosthesis infection, but in case of any suspicion of septic loosening, a two-stage performance provides a safety method to control the infection. Moreover, we analyze some of the technical problems found in the second-stage procedure as complexity of the joint approach and bone loss after using a static antibiotic-impregnated spacer.
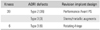
From January 2000 to January 2007, the two fellows trained in joint arthroplasty (AS and FA) performed 48 two-stage revisions with a diagnosis of chronically septic knee prostheses in 46 patients at our institution. During the same period, these surgeons performed a total of 98 TKA revisions and 634 TKAs. Demographic data of the patients are shown in Table 1.
After anesthesia, the knee was set for the surgery, and before surgical incision, the affected knee was aspirated. Joint aspiration was performed as far away as possible from the location of the draining sinus if it was present. Fluid was sent for the nucleated cell count and culture. At this moment, the anesthesiologist gave intravenous prophylactic antibiotics (first-generation cephalosporin or vancomycin in β-lactamic allergic patients as recommended by our hospital infection control committee). If infecting organism was known preoperatively, the organism-specific antibiotic was administered after knee aspiration.
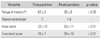
An infection was considered present if aspiration culture or deep tissue culture obtained during surgery yielded microorganisms, if purulent discharge was present during removal of the implant or if there were clinical symptoms with elevated C-reactive protein (CRP > 5), elevated erythrocyte sedimentation rate (ESR > 20) and high fluid leukocyte count with > 64% for the neutrophil differential. Preoperative joint aspiration with positive culture, high fluid leukocyte count with > 64% neutrophil differential and clinical symptoms were our references to establish septic loosening in patients with rheumatoid arthritis. Microorganisms related to these cases are shown in Table 2. Negative culture results were checked in 14 out of the 48 knees.
The first stage operation was performed through medial parapatelararthrotomy in a routine fashion. It included surgical debridement, total synovectomy and removal of all the previous implant and cement. Sets of joint swabs and synovial tissue specimen in a representative area of the membrane (bone-prostheses interface) were taken for microbiological culture (aerobic, anaerobic, mycobacterium and fungal) and pathological examination. An antibiotic-impregnated cement block (0.55 g of gentamicin sulfate; Palacos R with gentamicin, Biomet, Warsaw, IN, USA) was placed in the articular space. A splint in extension was applied to the leg after suturing the incision and a drainage output was left for 48 hours. Prophylactic low molecular weight heparin (enoxaparin) was used for the next four weeks and empirically double intravenous antibiotics (the one administered at surgery plus an amynoglucosid) were employed until the results of the culture were checked.
Once the results of the culture were obtained, intravenous antibiotics according to the sensitivity test of the culture were applied, during his/her hospital stay (range, 7 to 10 days). A leg immobilizer was prepared before patient's discharge from our institution (as soon as he/she was free of infection signs clinically and serum CRP values were decreasing). Additional oral antibiotics were given for another 5 weeks. Patients were allowed ambulation with walker support.
A follow-up was done at the outpatient office six weeks after surgery with a new assessment of ESR and CRP. Recurrent infection was defined when elevated ESR and CRP values, aspiration culture and clinical signs of infection of the knee were assessed after first-stage procedure. Four knees needed a second thorough debridement before the second-stage operation due to recurrent infection.
Second-stage surgery was not undertaken until the knees were free of any sign of clinical infection and the patient had normal ESR and CRP values. At this moment,the cement spacer block was removed and a new debridement was performed. Intraoperative deep tissues were achieved again for bacterial culture and pathological examination. A medial parapatellar approach was used with additional V-Y quadricepsplasty (17 knees), quadriceps snip (7 knees) or tibial tubercle osteotomy (2 knees), if difficult surgical exposure was encountered. Implants used for the revision TKA were the Performance Avant PS (Biomet) in 39 knees and a rotating-hinge prosthesis in the rest: Rotating Hinge Knee (RHK; Biomet) in one case, Orthopaedic Salvage system (OSS; Biomet) in one case and Endo-Model Link (Waldemar Link, Hamburg, Germany) in four cases. Tibial or femoral bone defects were substituted by metallic augments in the prostheses. Stemmed prostheses with cement only on the surface of the implant were used in all the knees in order to preserve the bone stock. Tibial offset was used in 31 revisions, but not in the femoral side asit is not available in the Performance Avant PS for revision system. The patella was resurfaced in no knee due to poor bone stock and because of our good scores not resurfacing it in the aseptic revisions.
Patients received one week of intravenous antibiotics according to the sensitive test of the first bacterial culture, followed by two weeks of oral antibiotics. They started physiotherapy of the knee 48 hours after surgery when drains were removed. Partial weight bearing on the operated limb was allowed immediately, and full weight bearing was allowed at the first follow-up. Patients returned for postoperative follow-up at 6, 12, 24 weeks and then annually for clinical and radiological evaluation of the knee. Blood tests, including ESR and CRP, were obtained at six and twelve weeks to confirm the return of these parameters to the normal values.
A deep tissue culture, after second stage procedure, yielded no bacterial growth in all the knees. No residual infection was found in the histological examination of the periarticular tissue during reimplantation surgery.
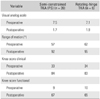
Bone defects were classified following the Anderson Orthopaedic Research Institute (AORI) system of Engh and Ammeen,7) and we divided our patients in two groups, depending on the revision implant design employed (Table 3).
Visual analog scale (VAS 0-10: 0, no pain; 10, severe pain) and Knee Society clinical rating scores8) were assessed before surgery and at the final follow-up. Standing anteroposterior and lateral radiographs of the knee were taken at each visit and assessment was performed by an orthopaedic surgeon (RL) not involved in the care of patients. Serial radiographs were reviewed retrospectively for evidence of the linear or focal osteolysis, alignment and component stability.
Normal ESR and CRP values9,10) and absence of clinical signs of infection with no progressive radiolucent line around the prostheses were used as references of suitable development.
A paired t-test was used to compare the differences between preoperative and postoperative clinical and functional outcomes, as well as range of motion (ROM). Analyses were performed using SPSSver. 13.0 (SPSS Inc., Chicago, IL, USA).
Three patients were lost to follow-up, two of them died of unrelated causes. The remaining 43 patients (45 knees) make up this series. The mean follow-up was 86 months (range, 60 to 132 months). The average interval between the first-stage resection and reimplantation was 4.4 months (range, 3.1 to 8.7 months). Four patients required a new debridement after the first-stage procedure due to lasting infection; therefore, they went through definitive surgery of more than 6 months after the first-stage surgery.
Two knees (4.44%) suffered from recurrent infection 8 months after the initial two-stage surgery. Co-morbidities in these patients were diabetes mellitus and rheumatoid arthritis, and during the follow-up, elevated ESR and CRP values and clinical signs of infection were detected. In one case, the recurrent infection was caused by the same microorganism (methicillin-resistant Staphylococcus aureus [MRSA]), and in the other one, the first culture was negative and the reinfection was caused by Staphylococcus spp. All of them were successfully treated by a new debridement, removal of the prostheses and two-stage arthrodesis with a cemented intramedullary nail (arthrodesis nail Endo Model Link). The interval between removal of the implant and definitive arthrodesis was 3 months, and a new impregnated-antibiotic cemented spacer with gentamicin (Palacos R with gentamicin) was placed for this period of time. The other 43 knees were free of infection at the final follow-up with an overall infection control rate of 95.6%.
The VAS improved from a preoperative value of 7.3 to 1.9 points, postoperatively (p < 0.05). The ROM improved from an average of 62° preoperatively (range, 10° to 85°) to 92° at the latest follow-up (range, 50° to 115°; p < 0.05). The mean knee preoperative flexion contracture of 7° (range, 0° to 25°) was found in 8 knees and improved to 1.5°, postoperatively (range, 0° to 5°) (Table 4).
The mean Knee Society clinical rating score improved in the 43 surviving knees from 33 points (range, 5 to 54 points) to 83 points (range, 43 to 95 points; 50 points increase, p < 0.01). Functional rating score improved from 10 points (range, 5 to 30 points) to 65 points (range, 10 to 85 points; 55 points increase, p < 0.01) (Table 4).
Twenty-six knees required extensile techniques to surgical exposure of the joint at the time of revision. Knee and functional scores were alike those cases, in which no extensile exposure technique was required. However, the extension lag of about 8° was observed in 7 cases of V-Y quadricepsplasty, and one of quadriceps snip and patella infera was related to these approaches in five cases.
Radiographic evaluation showed a stable component fixation with suitable alignment and no signs of mechanically loosening in all 43 knees. There were no radiolucencies around the revised prostheses in the follow-up X-rays. The use of metallic augments (32 in the femoral component and 29 at the tibial one) allowed us to compensate bone loss, avoiding the use of structural or morselized allograft, which is expensive in our environment and delay weight bearing.
No significant differences related to pain level (p = 0.45), ROM (p = 0.33), Knee Society clinical score (p = 0.25) or Knee Society functional scores (p = 0.51) were encountered between the semi-constrained knees and rotating-hinge knees used in this series; although the limited number of rotating-hinged prostheses made it difficult to obtain significant results (Table 5).
Main complications included extension lag of the knee in 7 knees, partial avulsion of the patellar tendon in four (cases in which no extensile exposure approach had been used) and flexion contracture (less than 5°) of the knee in two. The extension lag was no bigger than 8° and patients accepted the restrictions. Two of them were ambulated with a knee immobilizer to help them to block knee extension. The four partial avulsion of the patellar tendon were successfully repaired with heavy suture or staples.
Revision of chronically infected TKA remains a challenge for orthopaedic surgeons due to infection eradication and problems in recreating anatomy and restoring knee function. A two-stage reimplantation remains as the most effective treatment for eradicating infection in chronically infected TKAs.2,11) A two-stage revision TKA, a demanding procedure that should be performed by experienced surgeons,12) has a successful rate between 85% and 95%13) similar to the results in this series.
To manage the remaining space after removal of the infected prosthesis, antibiotic-impregnated cement beads, acting as static spacers or articulating spacers, can be used.11,14-16) We have used antibiotic-impregnated cement beads that act as static spacers mainly for the significance of the bone defects in most of the cases, which made us difficult to adapt mobile spacers with proper ligament and soft tissue tension. Moreover, many cases in this series were performed five to twelve years ago, when mobile spacers were not so common in our institution. For many years, two-stage revision of septic TKAs has been done with static spacers and has been associated with less satisfactory knee motion.17) However, though better postoperative ROM is associated to mobile spacers, differences are not statistically significant.15,16) Our short experience with preformed articulating knee spacers have not shown great benefits as Johnson et al.16) show in his report. In our series, we give more importance to infection eradication than to ROM after second-stage procedure. Ninety to ninety-five degrees of knee flexion after such complex scenery may be considered as a good functional result that allows the patients to do most of their daily living activities.
The cemented block has many advantages, as it serves as a local antibiotic-delivery system, and provides mechanical stability to the knee and acts as a mechanical spacer for the ligament and soft tissue tension. It can be reinforced with intramedullary nail in cases where significant bone loss and/or ligamentous instability prevent the formation of a stable joint with a conventional cemented spacer.18) Static knee spacers maintain the joint space, lessen capsular contracture around the joint, minimize debris generation and help in control of the infection. On the other hand, articulating spacers may prevent bone loss and facilitate reimplantation at the second-stage procedure,2,19) but generate debris between stages and complications due to technical errors or patient weight bearing compliance can be detected.16) We have routinely used Palacos with gentamicin as spacer and our Staphylococcus spp. infections represent the 23.5% of the cases. However, Stefansdottir et al.20) reflects his article that there is an increase in the rate of gentamicin resistance among coagulase-negative staphylococci; therefore, we will have to reconsider changing the antibiotic in the spacer.
Our final control infection rate was 95.6% as a good result, as other authors obtained with two-stage protocol on the management of neglected chronically infected knee prosthesis.12,21) We had two cases of recurrent infection in patients with obvious co-morbidities. We decided to perform a two-stage arthrodesis with an intramedullary nail because one case was produced by MRSA, a predictor of reimplantation failure,22) and in the other case, signs of significant bone loss and joint instability were presented in the harmful patient.
Barrack et al.23) reported that knees who require quadriceps snip, have equivalent results to those who underwent a standard approach and higher scores than V-Y turn-down and tibial tubercle osteotomy in a multicenter series. In the current study, knees requiring V-Y quadricepsplasty after a static spacer significantly improved ROM from 56.5° to 93.6°; however, seven patients developed an extension lag (8°) and five patients had a patella baja postoperatively. We started using this approach because it was the standard extensile incision in our media, but after analyzing our results, we will avoid V-Y quadricepsplasty in our future revisions. Nowadays, we use a standard approach (with patellar inversion method) or quadriceps snip in our last cases. Our scarce experience in tibial tubercle osteotomy and complications related to this approach make that we employed this extensile access in selected cases.24) The two patients who developed a flexion contracture had a preoperative stiffness of the knee (ROM 10° to 50°), advance age and poor general health; therefore, aggressive rehabilitation protocol was impossible.
Another so-called disadvantage of the antibiotic-impregnated cement static spacer is bone loss (around 40% on the tibial side and 44% on the femoral side), especially attributed to migration of the spacer blocks. Bone loss was associated with undersized spacers made without intramedullary stem. For that reason, we have tried to adapt the size of our spacer to the defect created after removal of the implant in the first-stage procedure. A short stem made of cement was introduced in the tibial and femoral side to minimize the cement block migration in order to preserve as much bone stock as possible (Fig. 1).
The degree of bone loss will determine the reconstructive options available, as the goals of revision TKA surgery are related to the establishment of implant stability on the host bone. Engh et al.7) described the AORI classification for bone deficiency and subdivided bone defects into three types.25) In the current report, 38 type 2 and 10 type 3 defects were found.
We managed bone deficiencies with femoral augments in 32 knees and tibial augments in 29 knees, as we have not encountered bone loss that extended beyond the scope, we could be handled by metallic augments after proper planification.26) Modular sleeves may allow stability on the host bone, while restoring the joint line. Tibial off-set was required in 31 cases to place the tibial base in proper contact with the host-bone. Diaphyseal-engaging cementless stems fixation combined with cemented metaphyseal fixation was used and showed as good results as in other series.27) During this series, we felt more comfortable using metallic augments that allow immediate weight bearing and rehabilitation to improve knee ROM and function. Rotating-hinged prostheses were our preferred implants in cases in which ligament deficiency was observed, and instability could be a problem with semi-constrained knees. Similar outcomes (ROM, VAS and Knee Society score) were achieved with these implants; however, the number of cases was inadequate to evaluate the results (Fig. 2).
Segmental knee replacement systems are designed for limb salvage after tumor resection, but massive bone loss is another indication for these systems.26,28) In one case with massive femoral bone loss after a chronically infected rotating-hinge prothesis from another institution, procedure with an OSS for the second stage surgery was performed. Lately, the patient showed an aseptic loosening of the femoral stem with pain and subsidence in the proximal femur twelve months after the surgery. In this case, a Compress Compliant Pre-Stress Device (Biomet) was used in the proximal femur. The system exemplifies Wolff's law through dynamic bone compression as it creates a stable high-pressure bone-implant interface for bone growth, preventing stress shielding.
Another female patient with distorted anatomy of the tibial canal suffered a periprosthetic tibial fracture four months after the surgery. A custom-made tibial monoblock component for RHK was our preference. A segmental tibial component with a narrow stem was designed for this case, and reattachment of the tibial tubercle was done with heavy sutures.
The retrospective nature of this series and the relative small number of patients included in the report (n = 45) comprise a limitation of this study. Moreover, scarce number of rotating-hinge prosthesis make difficult to analyze their results; although fortunately, we preserve this kind of prosthesis for significant bone losses or clinical signs of instability. Static spacers reduce risks of dislocation, instability, extrusion, overstuffing of the patellofemoral and tibiofemoral joint,13) but on the other hand, make revision surgery harder and offer a little bit of less ROM. Immobilization was believed to aid in control of joint infections, so static spacers might help to improve our pretty good rates of infection eradication.
Significant improvement was obtained in this series with respect to pain, clinical and functional scores, and infection eradication following two-stage revision TKA. We can conclude that two-stage reimplantation, using a static antibiotic-impregnated cement spacer, is an optimal procedure to eradicate infection and to restore acceptable functional results for daily patients' activities. However, the technique sometimes requires extensile surgical approaches that could imply arduous surgeries. Metallic augments with cementless stems, available in most of the knee revision systems, are a good option to treat bone deficiencies, avoiding the use of structural allografts with its complications.
Figures and Tables
Fig. 1
(A) A two-stage revision of a chronically infected knee. Antibiotic-impregnated cement beads acting as static spacer with a short cement stem to minimize cement block migration. (B) In the other images, we can see the knee after revision with a semi-constrained prosthesis with the stems (Performance Avant, Biomet).

Fig. 2
(A) A revision of multi-operated infected knee with sinus tract. First stage after removing the prosthesis. Static spacer adapted to the defect created. In this case we added Septopal-30 to increase the levels of gentamicin locally. (B) Stability was not achieved with semi-constrained prosthesis, so rotating-hinge prosthesis was employed in this case (RHK, Biomet).

References
1. Bozic KJ, Kurtz SM, Lau E, et al. The epidemiology of revision total knee arthroplasty in the United States. Clin Orthop Relat Res. 2010; 468(1):45–51.

2. Hsu CS, Hsu CC, Wang JW, Lin PC. Two-stage revision of infected total knee arthroplasty using an antibiotic-impregnated static cement-spacer. Chang Gung Med J. 2008; 31(6):583–591.
3. Insall JN, Thompson FM, Brause BD. Two-stage reimplantation for the salvage of infected total knee arthroplasty. J Bone Joint Surg Am. 1983; 65(8):1087–1098.

4. Volin SJ, Hinrichs SH, Garvin KL. Two-stage reimplantation of total joint infections: a comparison of resistant and nonresistant organisms. Clin Orthop Relat Res. 2004; (427):94–100.
5. Jamsen E, Stogiannidis I, Malmivaara A, Pajamaki J, Puolakka T, Konttinen YT. Outcome of prosthesis exchange for infected knee arthroplasty: the effect of treatment approach. Acta Orthop. 2009; 80(1):67–77.

6. Cohen JC, Hozack WJ, Cuckler JM, Booth RE Jr. Two-stage reimplantation of septic total knee arthroplasty: report of three cases using an antibiotic-PMMAspacer block. J Arthroplasty. 1988; 3(4):369–377.
7. Engh GA, Ammeen DJ. Bone loss with revision total knee arthroplasty: defect classification and alternatives for reconstruction. Instr Course Lect. 1999; 48:167–175.
8. Insall JN, Dorr LD, Scott RD, Scott WN. Rationale of the Knee Society clinical rating system. Clin Orthop Relat Res. 1989; (248):13–14.

9. Ghanem E, Azzam K, Seeley M, Joshi A, Parvizi J. Staged revision for knee arthroplasty infection: what is the role of serologic tests before reimplantation? Clin Orthop Relat Res. 2009; 467(7):1699–1705.

10. Piper KE, Fernandez-Sampedro M, Steckelberg KE, et al. C-reactive protein, erythrocyte sedimentation rate and orthopedic implant infection. PLoS One. 2010; 5(2):e9358.

11. Borowski M, Kusz D, Wojciechowski P, Cielinski L. Treatment for periprosthetic infection with two-stage revision arthroplasty with a gentamicin loaded spacer: the clinical outcomes. Ortop Traumatol Rehabil. 2012; 14(1):41–54.

12. Hardeman F, Londers J, Favril A, Witvrouw E, Bellemans J, Victor J. Predisposing factors which are relevant for the clinical outcome after revision total knee arthroplasty. Knee Surg Sports Traumatol Arthrosc. 2012; 20(6):1049–1056.

13. Burnett RS, Kelly MA, Hanssen AD, Barrack RL. Technique and timing of two-stage exchange for infection in TKA. Clin Orthop Relat Res. 2007; 464:164–178.

14. Kohl S, Evangelopoulos DS, Kohlhof H, et al. An intraoperatively moulded PMMA prostheses like spacer for two-stage revision of infected total knee arthroplasty. Knee. 2011; 18(6):464–469.

15. Qiu XS, Sun X, Chen DY, Xu ZH, Jiang Q. Application of an articulating spacer in two-stage revision for severe infection after total knee arthroplasty. Orthop Surg. 2010; 2(4):299–304.

16. Johnson AJ, Sayeed SA, Naziri Q, Khanuja HS, Mont MA. Minimizing dynamic knee spacer complications in infected revision arthroplasty. Clin Orthop Relat Res. 2012; 470(1):220–227.

17. Wang CJ, Hsieh MC, Huang TW, Wang JW, Chen HS, Liu CY. Clinical outcome and patient satisfaction in aseptic and septic revision total knee arthroplasty. Knee. 2004; 11(1):45–49.

18. Nickinson RS, Board TN, Gambhir AK, Porter ML, Kay PR. Two stage revision knee arthroplasty for infection with massive bone loss: a technique to achieve spacer stability. Knee. 2012; 19(1):24–27.

19. Hofmann AA, Goldberg TD, Tanner AM, Cook TM. Ten-year experience using an articulating antibiotic cement hip spacer for the treatment of chronically infected total hip. J Arthroplasty. 2005; 20(7):874–879.

20. Stefansdottir A, Johansson D, Knutson K, Lidgren L, Robertsson O. Microbiology of the infected knee arthroplasty: report from the Swedish Knee Arthroplasty Register on 426 surgically revised cases. Scand J Infect Dis. 2009; 41(11-12):831–840.

21. Macheras GA, Kateros K, Galanakos SP, Koutsostathis SD, Kontou E, Papadakis SA. The long-term results of a two-stage protocol for revision of an infected total knee replacement. J Bone Joint Surg Br. 2011; 93(11):1487–1492.

22. Mortazavi SM, Vegari D, Ho A, Zmistowski B, Parvizi J. Two-stage exchange arthroplasty for infected total knee arthroplasty: predictors of failure. Clin Orthop Relat Res. 2011; 469(11):3049–3054.

23. Barrack RL, Smith P, Munn B, Engh G, Rorabeck C. The Ranawat Award: comparison of surgical approaches in total knee arthroplasty. Clin Orthop Relat Res. 1998; (356):16–21.
24. Chalidis BE, Ries MD. Does repeat tibial tubercle osteotomy or intramedullary extension affect the union rate in revision total knee arthroplasty? Aretrospective study of 74 patients. Acta Orthop. 2009; 80(4):426–431.

25. Mulhall KJ, Ghomrawi HM, Engh GA, Clark CR, Lotke P, Saleh KJ. Radiographic prediction of intraoperative bone loss in knee arthroplasty revision. Clin Orthop Relat Res. 2006; 446:51–58.

26. Fehring TK, Christie MJ, Lavernia C, et al. Revision total knee arthroplasty: planning, management, and controversies. Instr Course Lect. 2008; 57:341–363.




 PDF
PDF ePub
ePub Citation
Citation Print
Print




 XML Download
XML Download