Abstract
Background
Total hip arthroplasty (THA) for severe developmental dysplasia of the hip (DDH) is a technically demanding procedure for arthroplasty surgeons, and it is often difficult to reduce the hip joint without soft tissue release due to severe flexion contracture. We performed two-stage THAs in irreducible hips with expected lengthening of the affected limb after THA of over 2.5 cm or with flexion contractures of greater than 30 degrees in order to place the acetabular cup in the true acetabulum and to prevent neurologic deficits associated with acute elongation of the limb. The purpose of this study is to evaluate the outcomes of cementless THA in patients with severe DDH with a special focus on the results of two-stage THA.
Methods
Retrospective clinical and radiological evaluations were done on 17 patients with Crowe type III or IV developmental DDH treated by THA. There were 14 women and 3 men with a mean age of 52.3 years. Follow-ups averaged 52 months. Six cases were treated with two-stage THA followed by surgical hip liberalization and skeletal traction for 2 weeks.
Results
The mean Harris hip score improved from 40.9 to 89.1, and mean leg length discrepancy (LLD) in 13 unilateral cases was reduced from 2.95 to 0.8 cm. In the patients who underwent two-stage surgery, no nerve palsy was observed, and the single one-stage patient with incomplete peroneal nerve palsy recovered fully 4 weeks postoperatively.
Conclusions
The short-term clinical and radiographic outcomes of primary cementless THA for patients with Crowe type III or IV DDH were encouraging. Two-stage THA followed by skeletal traction after soft tissue release could provide alternative solutions to the minimization of limb shortenings or LLD without neurologic deficits in highly selected patients.
Total hip arthroplasty (THA) for severe developmental dysplasia of the hip (DDH) is a technically demanding procedure for arthroplasty surgeons due to the presence of anatomical abnormalities such as, a small, narrow femoral canal, increased anteversion, and a hypoplastic acetabulum.1,2) Some authors have suggested that irreducible high hip dislocations should be considered a contraindication for THA due to higher rates of failure and complications than standard procedures.2-5) However, recent reports have described successful outcomes of THA in severe DDH after securing fixation of the acetabular cup placed in the true acetabulum and reducing neurologic traction injury by subtrochanteric shortening osteotomy.6-15) Incongruences between proximal and distal canal diameters after shortening lead to problems regarding the achievements of secure fixation between osteotomy sites, and might increase the risk of nonunion.8) In Crowe type IV DDH, it is often difficult to reduce the hip joint without soft tissue release due to severe flexion contracture; furthermore, remaining soft tissue contractures may lead to gait disturbance after surgery. Therefore, we performed two-stage THAs in irreducible hips with expected lengthening of the affected limb after THA of over 2.5 cm or with flexion contractures of greater than 30 degrees in order to place the acetabular cup in the true acetabulum and to prevent neurologic deficits associated with acute elongation of the limb. The purpose of this study is to evaluate the outcomes of cementless THA in patients with severe DDH with a special focus on the results of two-stage THA.
The study protocol was approved by the institutional review board of our hospital, and informed consents were obtained from all patients. Between 2004 and 2008, the THA was performed in 52 patients (58 hips) with DDH. According to Crowe's classification,11) 21 hips (17 patients) with severe DDH (15 hips of Crowe type III and 6 hips of type IV) were retrospectively identified and reviewed. There were 14 women and 3 men with the mean age of 52.3 years (range, 34 to 72 years). All patients were followed for an average of 52 months (range, 38 to 72 months). Thirteen patients had unilateral involvements and 4 patients had bilateral involvements. No patient had a history of prior surgeries for DDH.
All operations were performed by a single senior surgeon using a modified Hardinge's lateral approach in the lateral decubitus position. Two-stage operations were planned in 6 irreducible hips with expected lengthening of the affected limb after THA of > 2.5 cm or with flexion contracture of > 30 degrees. In the 6 staged operations, surgical hip liberalization with abductor slide was performed through two skin incisions during the first stage (Fig. 1). Through a curvilinear incision over the iliac crest, abductors were detached from the ilium by subperiosteal dissections. This dissection was then continued inferiorly to the acetabular rim and posteriorly to the sciatic notch and the posterior superior iliac spine. The entire abductor origin was then mobilized from the pelvis without any tensions. After the femoral head had been resected through a modified Hardinge's lateral approach, the tensor fascia lata, sartorius muscle, iliopsoas tendon, and rectus femoris were sequentially released. Adductor tenotomy was additionally performed in cases with adductor contractures. After resecting the elongated hypertrophic joint capsule, the true acetabulum was identified and prepared using a small reamer. The trial acetabular component was then placed in the acetabulum to evaluate the bone stock. The resected femoral head was stored at our institutional bone bank for possible uses as a bulk autogenous bone graft to augment the acetabulum in the event of inadequate acetabular bone coverage for cup fixation. After the first operations, gradual skeletal traction was applied to the operated limb by placing a metal pin through the proximal tibia for 2 weeks. Traction weight was gradually increased to a maximum of one fourth of body weight, but reduced or removed when a patient complained of symptoms suspicious of neuralgia. A portable radiograph was taken to confirm that the greater trochanter tip retracted inferiorly to the center of the true acetabulum. During second operations, one hip was successfully reduced without femoral shortening, but 5 hips were difficult to reduce with trial components, and therefore, subtrochanteric shortening osteotomies were performed to prevent neurologic traction injuries. After subtrochanteric osteotomy, the onlay cortical bone graft with resected bone was affixed to the osteotomy site with cerclage cable (Fig. 2). The remaining 15 hips were treated by one-stage THA with soft-tissue release alone (Fig. 3). During the operative procedures, we did not explore nor palpate the sciatic nerve to evaluate tensions.
The acetabular cup was placed in the true acetabulum in all hips. Secure fixation of the cup was achieved in 11 of the 21 hips without bone grafting, while a bulk autogenous or allogenous femoral head bone graft was augmented to the acetabulum in 4 hips with unreliable fixation and insufficient bone coverage. Augmentation of the superolateral rim with cancellous bone graft was performed to increase the bone stock for future revisions in 6 hips with reliable fixation, despite insufficient bone coverage.
The cementless Duraloc acetabular component (DePuy, Warsaw, IN, USA) and Biolox forte (CeramTec, Plochingen, Germany) alumina-on-alumina bearing system was used in all hips. Femoral component fixation was uncemented in all hips. A straight, tapered, titanium Summit stem (DePuy) was used in 14 of the 21 hips, and the remaining 7 femoral components were S-ROM modular stems (DePuy). Femoral head size was 28 mm in all hips. Acetabular cups in the outer diameter ranged from 46 to 54 mm.
All patients were mobilized on the third day after THA. After one-stage THA, partial weight bearing with crutches was allowed from 5 days to 6 weeks, postoperatively. Thereafter, weight bearing was progressively increased. An abductor brace was applied to patients that underwent two-stage THA, and partial weight bearing with crutches was allowed from 7 days to 6 weeks. Full weight bearing was started based on radiographically evident osteotomy site consolidation.
In unilateral DDH cases, leg length discrepancy (LLD) was defined as the difference between the distances from the interteardrop line and the greater trochanter tip in affected and contralateral hips on anteroposterior hip radiographs, and was measured before and after surgery (Fig. 4). Clinical assessments were performed using Harris hip scores. The level of activities of the patients was assessed using the University of California, Los Angeles (UCLA) activity score at the latest follow-up.
All patients were reviewed radiologically at 6 weeks, 3 months and 6 months after surgery, and annually thereafter, and the presence of radiolucent lines around the acetabular component in the three zones defined by DeLee and Charnley16) was noted. Mode of fixation of the femoral component was classified as bone ingrowth, stable fibrous fixation, or unstable, as described by Engh et al.17) Osteolytic lesions were documented and classified by size and location.11) Serial radiographs were assessed to evaluate bony union at femoral osteotomy sites and at acetabular bone grafted sites. Data processing and statistical analyses were performed using SPSS ver. 17.0 (SPSS, Chicago, IL, USA). The Wilcoxon signed rank-sum test was used to compare preoperative and postoperative Harris hip scores. A p-value below 0.05 was considered significant.
Mean LLD significantly decreased from 3.0 cm (range, 1.5 to 7.0 cm) before surgery to 0.8 cm (range, 0 to 2.2 cm) at final follow-up evaluations. Postoperatively, mean leg lengthening was 2.4 cm (range 1.2 to 4.8 cm). The mean Harris hip score significantly increased from 40.9 (range, 21 to 73) to of 89.1 (range, 62 to 98) at the final follow-up (p < 0.01). At the latest follow-up, the mean UCLA activity score was 6.8 (range, 4 to 9) in all patients, 5.8 (range, 4 to 8) in 5 patients treated with two-stage THA, and 7.4 (range, 5 to 9) in 12 patients with one-stage THA. Preoperatively, all patients had a moderate to severe limp, but at the final follow-up, nine patients were limp free, one had a moderate limp, and seven had a slight limp. The Trendelenburg test was positive in one of the 15 hips that underwent one-stage THA and in three of the six hips treated by two-stage THA. Out of 7 patients with a postoperative slight limp, five patients did not use any ambulatory aids and the remaining two patients used a cane just for long distance ambulation at final follow-up evaluations. Only one patient with a moderate limp who was treated with two-stage THA required a cane for daily walking.
No acetabular cup migration or periacetabular radiolucent line was observed, and there were no evidences of osteolytic lesions. All bone grafts used to augment the acetabulum unified. No femoral stem subsided. Four hips exhibited a radiolucent line in Gruen zones 1, 4, or 7 of less than 2-mm thick. Twenty hips eventually showed bony ingrowth of femoral component and one hip showed stable fibrous fixation (Fig. 5). The mean length of resected bone by subtrochanteric shortening osteotomy in five hips was 1.6 cm (range, 1.2 to 2.0 cm), and solid bony union of the femoral osteotomy was achieved in all cases. Heterotopic ossification was found in three cases, but without any functional limitations.
No nerve palsy occurred in the six cases that underwent two-stage THA, and the single case of incomplete peroneal nerve palsy after one-stage THA, fully recovered at 4 weeks postoperatively. No patients experienced other major complications, such as a postoperative dislocation, infection, or periprosthetic fracture.
The outcomes of THA in severe DDH has been reported to be poorer than that in hips without DDH,1,2) because the anatomy in DDH is distorted by soft tissue contracture, inadequate bone stock, an abnormal hip center location, abnormalities of neurovascular structures, and LLD.10) Several authors have reported that acetabular cups positioned at a high hip center tend to exhibit early loosening because bone stock provides limited component support,18,19) and thus, most authors agree that the acetabular component should be positioned at the level of the true acetabulum. However, this produces excessive leg lengthening and increases the risk of sciatic or femoral nerve palsy. On the other hand, appropriate shortening of the femur avoids these adverse effects.
One of several osteotomy and fixation techniques described in the literature involves metaphyseal femoral shortening and distal advancement of the trochanter technique, but it has been reported to introduce the risk of reducing abductor power due to inadequate trochanter reattachment or nonunion.3,20) Subtrochanteric shortening osteotomy has been demonstrated to allow control of leg length, preservation of the abductor mechanism, and the correction of anteversion.6-11) However, incongruence between the canal diameters of apposed fragments is exacerbated by excessive resection of the diaphyseal segment and this might interfere with secure fixation, and thus, solid union at the osteotomy site8) (Fig. 6). For this reason, we attempted to minimize the length of femoral resection by subtrochanteric shortening osteotomy. In the six hips requiring excessive femoral shortening to enable the acetabular component to be placed in the true acetabulum, two-stage THA was performed after surgical hip liberalization with abductor slide and skeletal traction. One of these hips was successfully reduced without subtrochanteric osteotomy, and the largest length of femoral resection in the remaining hips was only 2 cm, even in the case with an LLD of 7 cm. In the current study, the mean length of resected bone by subtrochanteric osteotomy in five hips was 1.6 cm (range, 1.2 to 2.0 cm), and solid bony union of the femoral osteotomy was achieved in all cases without neurologic deficits.
Although it is difficult to compare our results directly with those of others, due to the small number of patients recruited, the amount of bone resected in this study was relatively small as compared with other studies using a similar technique (Table 1). It is generally accepted that lengthening of the leg by more than 4 cm can result in sciatic or femoral nerve palsy.21) However, Jasty et al.22) suggested that over-lengthening by more than 2 cm may lead to sciatic nerve palsy, if the shortening has occurred in childhood. Therefore, we performed staged THAs after gradual skeletal traction with soft tissue release and used the abductor slide technique to avoid neurologic traction injury when the affected limb was considered to require lengthening by more than 2.5 cm. In the present study, no nerve palsy occurred after two-stage THA, even in one case requiring 4.8 cm of limb lengthening.
Harley and Wilkinson23) introduced an extensive release technique for shortened abductors and flexors through a separate skin incision over the iliac crest in unreduced DDH, and reported that all prosthetic joints were reduced without undue tensions because released muscles slid inferiorly with femur. The third upper ilium was excised to allow resuturing of released muscles without tensions, and all patients underwent one-stage THA. However, we did not osteotomize the ilium to avoid associated morbidity, and performed two-stage THAs after gradual skeletal traction because Harley and Wilkinson reported two cases of neuropraxia of the femoral nerve. Chin and Brick24) also introduced a similar abductor slide technique in the revision THA that does not involve resuturing of released muscles, and reported a mild or moderate postoperative limp in two of the 4 cases without functional limitations. They suggested that abductor muscle weakness can be minimized in the absence of injury to the neural branches if patients are enrolled in a strengthening and endurance rehabilitation program postoperatively. In the current study, we did not resuture released abductors to allow sliding on the ilium at second operations; three of the 6 hips had a positive Trendelenburg test postoperatively.
Cemented femoral components are unsuitable for patients with osteoarthritis secondary to DDH, due to metal fatigue of small-sized stems or failure of the narrow cement mantle; and because the cement leakage into the osteotomy site can interfere with bone unions.3,8,19) Therefore, we used cementless femoral stems in all hips (the S-ROM modular stem in 7 hips with excessive anteversion and the straight, tapered Summit stem in the other 14 hips).
The limitations of this study include its retrospective nature, the relatively short follow-ups used to determine THA outcomes, and the small number of patients enrolled. The expected advantages of the described two-stage THA technique are: 1) Neurologic traction injury caused by acute elongation of the limb can be prevented by gradual skeletal tractions; 2) Limb shortening can be minimized by reducing the length of femoral bone resection or by avoiding trochanteric shortening osteotomy; and 3) Secure fixation of subtrochanteric osteotomy sites can be achieved and the risk of nonunion might be reduced by minimizing incongruence between canal diameters after subtrochanteric shortening. However, large-scale, long-term follow-up studies are needed to confirm these benefits.
In conclusion, the short-term clinical and radiographic outcomes of primary cementless THA for patients with Crowe type III or IV DDH were encouraging. Two-stage THA followed by skeletal traction after soft tissue release could provide an alternative solution to the minimization of limb shortening or LLD without neurologic deficit in highly selected patients.
Figures and Tables
Fig. 1
A curvilinear incision over the iliac crest was used to elevate abductor muscles off the ilium subperiosteally (A). The hip was exposed through a modified Hardinge's approach (B).

Fig. 2
Preoperative plain radiograph showing Crowe type IV developmental dysplasia of the hip (A). During the first stage, surgical hip liberalization with abductor slide and skeletal traction for 2 weeks were performed (B, C). During the second stage, a total hip arthroplasty and subtrochanteric shortening osteotomy were performed due to difficult reduction (D).
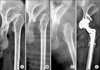
Fig. 3
Preoperative radiograph showing Crowe type III developmental dysplasia of the hip (A). One-stage total hip arthroplasty was performed and the superolateral aspect of the acetabulum was augmented with an autogenous femoral head bone graft (arrow, B). Solid union was confirmed by plain radiography at 3 years after surgery (arrowhead, C).

Fig. 4
In cases of unilateral developmental dysplasia of the hip, leg length discrepancy was defined as the difference between the distances from the interteardrop line and the greater trochanter tip in the affected and contralateral hips on anteroposterior hip radiographs and was measured before and after surgery (b - a).

Fig. 5
Postoperative plain radiograph taken at 2 years after surgery showing a diffuse radiolucent line of less than 2 mm in Gruen zones 1 and 7 (A). This was considered to indicate stable fibrous fixation because no change was observed 1 year later (B).

References
1. Argenson JN, Flecher X, Parratte S, Aubaniac JM. Anatomy of the dysplastic hip and consequences for total hip arthroplasty. Clin Orthop Relat Res. 2007; 465:40–45.

2. Crowe JF, Mani VJ, Ranawat CS. Total hip replacement in congenital dislocation and dysplasia of the hip. J Bone Joint Surg Am. 1979; 61(1):15–23.

3. Anwar MM, Sugano N, Masuhara K, Kadowaki T, Takaoka K, Ono K. Total hip arthroplasty in the neglected congenital dislocation of the hip: a five- to 14-year follow-up study. Clin Orthop Relat Res. 1993; (295):127–134.
4. Cameron HU, Botsford DJ, Park YS. Influence of the Crowe rating on the outcome of total hip arthroplasty in congenital hip dysplasia. J Arthroplasty. 1996; 11(5):582–587.

5. Charnley J, Feagin JA. Low-friction arthroplasty in congenital subluxation of the hip. Clin Orthop Relat Res. 1973; (91):98–113.

6. Eskelinen A, Helenius I, Remes V, Ylinen P, Tallroth K, Paavilainen T. Cementless total hip arthroplasty in patients with high congenital hip dislocation. J Bone Joint Surg Am. 2006; 88(1):80–91.

7. Takao M, Ohzono K, Nishii T, Miki H, Nakamura N, Sugano N. Cementless modular total hip arthroplasty with subtrochanteric shortening osteotomy for hips with developmental dysplasia. J Bone Joint Surg Am. 2011; 93(6):548–555.

8. Togrul E, Ozkan C, Kalaci A, Gulsen M. A new technique of subtrochanteric shortening in total hip replacement for Crowe type 3 to 4 dysplasia of the hip. J Arthroplasty. 2010; 25(3):465–470.

9. Biant LC, Bruce WJ, Assini JB, Walker PM, Walsh WR. Primary total hip arthroplasty in severe developmental dysplasia of the hip: ten-year results using a cementless modular stem. J Arthroplasty. 2009; 24(1):27–32.

10. Reikeras O, Haaland JE, Lereim P. Femoral shortening in total hip arthroplasty for high developmental dysplasia of the hip. Clin Orthop Relat Res. 2010; 468(7):1949–1955.

11. Nagoya S, Kaya M, Sasaki M, Tateda K, Kosukegawa I, Yamashita T. Cementless total hip replacement with subtrochanteric femoral shortening for severe developmental dysplasia of the hip. J Bone Joint Surg Br. 2009; 91(9):1142–1147.

12. Krych AJ, Howard JL, Trousdale RT, Cabanela ME, Berry DJ. Total hip arthroplasty with shortening subtrochanteric osteotomy in Crowe type-IV developmental dysplasia. J Bone Joint Surg Am. 2009; 91(9):2213–2221.

13. Makita H, Inaba Y, Hirakawa K, Saito T. Results on total hip arthroplasties with femoral shortening for Crowe's group IV dislocated hips. J Arthroplasty. 2007; 22(1):32–38.

14. Masonis JL, Patel JV, Miu A, et al. Subtrochanteric shortening and derotational osteotomy in primary total hip arthroplasty for patients with severe hip dysplasia: 5-year follow-up. J Arthroplasty. 2003; 18:3 Suppl 1. 68–73.

15. Park MS, Kim KH, Jeong WC. Transverse subtrochanteric shortening osteotomy in primary total hip arthroplasty for patients with severe hip developmental dysplasia. J Arthroplasty. 2007; 22(7):1031–1036.

16. DeLee JG, Charnley J. Radiological demarcation of cemented sockets in total hip replacement. Clin Orthop Relat Res. 1976; (121):20–32.

17. Engh CA, Bobyn JD, Glassman AH. Porous-coated hip replacement: the factors governing bone ingrowth, stress shielding, and clinical results. J Bone Joint Surg Br. 1987; 69(1):45–55.

18. Linde F, Jensen J, Pilgaard S. Charnley arthroplasty in osteoarthritis secondary to congenital dislocation or subluxation of the hip. Clin Orthop Relat Res. 1988; 227:164–171.

19. Pagnano W, Hanssen AD, Lewallen DG, Shaughnessy WJ. The effect of superior placement of the acetabular component on the rate of loosening after total hip arthroplasty. J Bone Joint Surg Am. 1996; 78(7):1004–1014.
20. Paavilainen T. Total hip replacement for developmental dysplasia of the hip. Acta Orthop Scand. 1997; 68(1):77–84.
21. Edwards BN, Tullos HS, Noble PC. Contributory factors and etiology of sciatic nerve palsy in total hip arthroplasty. Clin Orthop Relat Res. 1987; (218):136–141.

22. Jasty M, Webster W, Harris W. Management of limb length inequality during total hip replacement. Clin Orthop Relat Res. 1996; (333):165–171.





 PDF
PDF ePub
ePub Citation
Citation Print
Print




 XML Download
XML Download