Abstract
Background
In cervical anterior approach, transverse skin incision is preferred due to cosmetic reasons. Precise skin incision is required to reach the surgery segment while minimizing soft tissue injury. Skin incision site is frequently identified using C-arm fluoroscopy or the carotid tubercle. Accordingly, this study was conducted to investigate the efficacy of skin incision using the carotid tubercle as a marker.
Methods
This study was retrospectively conducted on 114 patients who underwent anterior cervical surgery by the same surgeon from April 2004 to June 2012. The rate of the appropriate insertion of K-wire, which was inserted into the disc after anterior approach, into the surgery segment was compared between 62 patients where skin incision site was identified using C-arm fluoroscopy before skin incision and 52 patients where skin incision site was identified using carotid tubercle palpitation before surgery.
Results
The needle was shown to have been inserted into the planned site in 106 patients out of the total 114 patients. The appropriate insertion of the needle was shown in 59 patients of group I (95.2%) and in 47 patients of group II (90.4%). Although the success rate was higher in group I than group II, it was statistically insignificant. The success rate of one-segment surgery was shown to be 89.7% in group I and 82.6% in group II. Although the success rate was higher in group I than group II, it was statistically insignificant. The success rate of two-segment surgery was shown to be 100% in group I, and 96.4% in group II due to one case of the failure at C3-4 and C5-6. The success rate of three- and four-segment surgeries was shown to be 100% in both groups.
Conclusions
The identification of skin incision site via carotid tubercle palpation was useful for surgeries involving two or more segments. Furthermore, it could be useful for one-segment surgery if surgical site is identified using vertebral body or soft tissues such as longus collis rather than insertion into the disc.
Anterior cervical surgery has been widely used to treat various conditions of the spine, including cervical disc herniation, fracture, ossification of posterior longitudinal ligament, and radiculopathy caused by joint of Luschka hypertrophy. This surgical approach has been used since Cloward1) and Smith and Robinson2) introduced an approach using transverse skin incision.3) In general, the anterior cervical approach is mainly used for short-level motion segment lesions, such as one- or two-motion segment, whereas the posterior approach is mainly used to treat lesions that involve multi-levels and motion segments. However, the anterior approach is also used for four-motion segment or multi-level corpectomy. Unlike a posterior approach, the anterior cervical approach can retract soft tissues located anterior to the vertebral body or disc. Thus, a skin incision site may be unimportant. However, as incision length becomes gradually shorter, the exact identification of a skin incision site becomes more important as soft tissue injury can be minimized and the decompression and instrumentation of the surgery segment can be performed more easily.
Anatomical landmarks can be used for skin incisions, which include cricoid cartilage, thyroid cartilage, angle of the mandible, cricothyroid membrane, or carotid tubercle. Some studies have reported that it was relatively easier to identify the angle of the mandible than the carotid tubercle.4) However, among the anatomical landmarks, the cricoid cartilages, thyroid cartilage, and lower margin of mandible have the disadvantage of change to the skin incision site when the cervical spine is extended. Meanwhile, the carotid tubercle has an advantage of consistency in skin incision site independent from the position and extension of the cervical spine as it is located at the transverse process of the sixth cervical vertebra.
Accordingly, this study was conducted to investigate the usefulness of the carotid tubercle in the identification of a skin incision site for anterior cervical surgery. The exact identification of a skin incision site was compared between the group that had their skin incision site determined using C-arm fluoroscopy prior to skin incision and the second group determined that had their skin incision site determined via carotid tubercle palpitation.
This study was conducted retrospectively on 114 patients who underwent anterior cervical surgery from April 2004 to June 2012, for one of several reasons: radiculopathy caused by cervical disc hernation or degenerative spondylosis; myelopathy caused by cervical disc herniation or ossification of posterior longitudinal ligament; or instability caused by cervical spine fracture, infectious spondylitis, or metastasis. The study was conducted after the approval from the Institutional Review Board of Seoul Metropolitan Government Seoul National University Boramae Medical Center (06-2012-135). The patients were divided into groups I and II. For group I that consisted of 62 patients from April 2005 to August 2008, the skin incision site was identified from a lateral view using C-arm fluoroscopy after draping. Meanwhile, for group II, this consisted of 52 patients from September 2009 to June 2012, skin incision site was identified by measuring the distance between the sixth cervical vertebra and the center of the planned surgery range in a preoperative plain X-ray after determining the location of the sixth cervical vertebra by palpating the left transverse tubercle (group II). In a supine position under systemic anesthesia, the cervical spine was positioned anteroposteriorly and thin padding was put on the posterior cervical spine, and both upper extremities were pulled longitudinally to maintain normal cervical lordosis (Fig. 1). If autogenous bone graft was required, thin padding was put on below the unilateral pelvis, and the bilateral knee was flexed 15°.
The platysma muscle was incised transversely and the superficial fascia was incised longitudinally via the Smith-Robinson approach. After the carotid sheath was pulled laterally and the trachea and esophagus were pulled medially, the deep fascia was incised longitudinally to reach the disc level. A 24-gauge needle was inserted into the disc (Fig. 1) or #1 K-wire was inserted into the vertebral body (Fig. 2) that was the closest to the skin incision site, and the correct level was identified using C-arm fluoroscopy. If the needle or K-wire was positioned within the range of the planned surgery, it was considered successful. Meanwhile, if not, it was considered unsuccessful.
The success rate of one-segment surgery, two-segments surgery, and multiple segment surgery with three-segments or more was compared between the groups, and the success rate was also compared according to segment position. The Fisher's exact probability test was conducted to compare the success rate of the surgery with and without C-arm fluoroscopy. Statistical significance was set at p < 0.05.
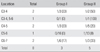
A total of 114 patients participated in the study. Their mean age was 53 ± 11 years. Of the 114 patients, there were 72 cases of cervical herniated intervertebral disc, 31 cases of myelopathy, 6 cases of fracture, 2 cases of infection, 2 cases of revision, and 1 case of metastasis. There was no significant difference in the patient characteristics (mean age, gender ratio, and symptom distribution by diagnosis) between group I and group II at baseline (Table 1).
The surgery consisted of 52 one-segment fusion surgeries, 57 two-segment fusion surgeries, and five three-segment fusion surgeries (Table 1). The segments involved in the surgeries consisted of 29 cases of C5-6, 24 cases of C5-6-7, 21 cases of C4-5-6, 9 cases of C6-7, 8 cases of C4-5, and 5 cases of C3-4-5 (Table 2). Among the 114 patients, a plate was used in 49 patients, the cage or intervertebral spacer was used in 57 patients, and the autograft or allograft was inserted in 8 patients. No significant difference was found between the two groups according to the surgery segments.
The needle was inserted into the predicted position in 106 patients among the 114 patients, who consisted of 59 patients (95.2%) of group I and 47 patients (90.4%) of group II. The success rate was higher in group I than group II, but it was statistically insignificant (p = 0.47). The success rate of surgery segment prediction was shown to be 89.7% (26/29 cases) in group I and 82.6% (19/23 cases) in group II for one-segment surgery. The success rate was higher in group I than group II, but it was statistically insignificant. The success rate of surgery segment prediction was shown to be 100.0% (29/29 cases) in group I and 96.4% (27/28 cases) in group II for two-segment surgery. It was shown to be 100.0% in both groups I and II for three- and four-segment surgeries.
Among the 8 cases where the needle failed to be positioned in the planned surgery segment, 2 cases occurred at the C3-4. The failure rate of surgery segment prediction was shown to be high in both groups I and II (33.3%, and 50%, respectively) (Table 3). One case of the failure of positioning the needle in the planned surgery segment occurred in both groups I and II for the C4-5 and C6-7, respectively. One case in the failure of positioning the needle in the planned surgery segment occurred in group II for C5-6, C3-4, and 5-6, respectively (Table 3). Among the 8 cases, 7 cases occurred for one-segment surgery. For the cases that occurred at the C3-4 and C5-6 in group II, they were non-continuous segments, and assessed unsuccessful as the needle was positioned at the C4-5.
Anterior cervical fusion is widely used for treating cervical spondylosis or fracture because of this procedures good clinical results and high fusion rate. Although anterior surgical approach has various modifications depending on position of the lesion, the Smith-Robinson approach is the most commonly used. In particular, Smith-Robinson approach is very effective in the treatment of cervical disc herniation, ossification of posterior longitudinal ligament, radiculopathy caused by spondylosis, and decompression, and instrumentation of myelopathy. In this study, for the anatomical positioning of the instrumentation, the cervical spine was positioned at the true anteroposterior area without rotation in all the cases, and normal lordosis was maintained without hyperextension. Although this cervical spine position is unlikely to significantly affect the identification of skin incision site by manually palpating the carotid tubercle, it is likely to be helpful for instrumentation at an appropriate position during plating. In particular, it is very important for artificial disc replacement.
In this study, no statistically significant difference was found in success rate of surgery segment prediction between the groups where skin incision site was identified using C-arm before the surgery and the group where skin incision site was identified via carotid tubercle palpation. In particular, inappropriate positioning was shown in 3 patients of the group using C-arm, which shows that radiologic determination does not guarantee the exact identification of the skin incision site. This is likely to be attributable to the fact that incision site can be positioned at other disc levels for cervical anterior soft tissues, as one segment upper and lower the incision level is easily approached via the retraction of cervical anterior soft tissues. The needle that was inserted after skin incision was positioned at the planned surgery segment in both the C-arm group and carotid tubercle palpation group for two or more surgery segments. However, inappropriate positioning was shown in both groups for one-segment fusion. The inappropriate positioning more occurred at segments other than C5-7, all of which occurred for one-segment surgery or isolated two-segment surgery. Radiologic examination is generally conducted by inserting K-wire or needle into the disc to identify the exact position during the surgery. However, as the insertion of the needle into the disc may deteriorate the degenerative changes of the disc,5-7) for one-segment surgery, as shown in the results of the study, it would be rather safer to insert the K-wire into the vertebral body.
Incision site identification using C-arm fluoroscopy has the advantage of less X-ray emission,8) but has disadvantages of delayed operation time and increased contamination. However, palpation of the carotid tubercle may not be so easy in some patients, particularly in those patients with a thicker neck. In the latter cases, we can palpate the protruded bony structure of C6 level by palpating the transverse process, one by one from the transverse process of C4-5 level, where the thyroid cartilage can be palpated superficially. If the carotid tubercle is difficult to identify by manual palpation due to the enlarged cervical spine soft tissue in a physical examination, C-arm fluoroscopy would be required to identify skin incision site. However, if a surgery involving two or more segments is required, skin incision via carotid tubercle palpation could be reliable. As skin incision site is positioned at the middle of the surgery site for surgeries involving two or more segments, the possibility of the inaccurate detection of the disc is very low. In fact, the omohyoid muscle is found during muscle dissection by exposing the C5-6 disc. The inferior belly of the omohyoid muscle mainly crosses the sternocleidomastoid muscle at the C5-6 disc level, and is positioned at the anterior area of the C6 vertebral body.9) Thus, it is also helpful in predicting the disc level. In addition, as no significant difference in the identification of skin incision site was found between the carotid tubercle palpation group and the C-arm fluoroscopy group for one-segment surgery, carotid tubercle palpation would be useful during the surgery. In this study, skin incision site was identified using C-arm in 62 patients in the early phase of the study, whereas it was identified via carotid tubercle palpation in 52 patients during the late phase of the study. As surgical performance could have been improved during the late phase of the study, the disc level of surgery segments could have been identified more skillfully. Nonetheless, the results of this study are meaningful as no disc level can be identified by an inaccurate incision.
In conclusion, the identification of skin incision site via carotid tubercle palpation is useful for surgeries to treat two or more segments. Furthermore, it could be useful for the treatment of one segment surgery if skin incision site is identified using the vertebral body or soft tissues, such as the longus collis, without insertion into the disc.
Figures and Tables
ACKNOWLEDGEMENTS
This work was supported by a clinical research grant-in-aid from the SMG-SNU Boramae Medical Center (03-2011-4).
References
1. Cloward RB. The anterior approach for removal of ruptured cervical disks. J Neurosurg. 1958; 15(6):602–617.

2. Smith GW, Robinson RA. The treatment of certain cervical-spine disorders by anterior removal of the intervertebral disc and interbody fusion. J Bone Joint Surg Am. 1958; 40(3):607–624.

3. Song KJ, Choi BW, Kim HY, Jeon TS, Chang H. Efficacy of postoperative radiograph for evaluating the prevertebral soft tissue swelling after anterior cervical discectomy and fusion. Clin Orthop Surg. 2012; 4(1):77–82.

4. Auerbach JD, Weidner Z, Pill SG, Mehta S, Chin KR. The mandibular angle as a landmark for identification of cervical spinal level. Spine (Phila Pa 1976). 2009; 34(10):1006–1011.

5. Zhang H, Yang S, Wang L, et al. Time course investigation of intervertebral disc degeneration produced by needle-stab injury of the rat caudal spine: laboratory investigation. J Neurosurg Spine. 2011; 15(4):404–413.

6. Michalek AJ, Buckley MR, Bonassar LJ, Cohen I, Iatridis JC. The effects of needle puncture injury on microscale shear strain in the intervertebral disc annulus fibrosus. Spine J. 2010; 10(12):1098–1105.

7. Zhang H, La Marca F, Hollister SJ, Goldstein SA, Lin CY. Developing consistently reproducible intervertebral disc degeneration at rat caudal spine by using needle puncture. J Neurosurg Spine. 2009; 10(6):522–530.





 PDF
PDF ePub
ePub Citation
Citation Print
Print






 XML Download
XML Download