Abstract
Background
There has been controversy whether methylmethacrylate precoating of the cemented femoral stem is a solution for aseptic loosening or rather contributes to increased failure rates in cemented total hip arthroplasties.
Methods
On a retrospective basis, we analyzed 76 primary hybrid total hip arthroplasties from 63 patients with precoated, cemented femoral stems between October 1990 and December 1995. The mean age of the patients was 46.8 years (range, 22 to 77 years) with a minimum follow-up of 14 years (mean, 15.5 years; range, 14 to 19.5 years). Third generation cementing techniques were employed in all cases.
Results
Twenty-four out of 76 cases (31.6%) showed aseptic loosening of the femoral stems, of which 23 stems were revised at an average revision time of 8 years (range, 3 to 14.8 years). The main mode of loosening was cement-stem interface failure in 22 hips (91.7%). Twenty-one out of 24 failed hips (87.5%) demonstrated C2 cementing grades (p < 0.001). Kaplan-Meier survivorship analysis using radiographic aseptic loosening of the femoral stem as the endpoint for failure showed survival rates of 76.5% at 10 years (95% confidence interval [CI], 71.4 to 81.6) and 63.2% at 19 years (95% CI, 57.3 to 69.1).
The most common cause of femoral stem failure after cemented total hip arthroplasty is aseptic loosening. Laboratory studies of postmortem specimens and finite element analysis revealed that loosening of the femoral stem is initiated by debonding at the cement-prosthesis interface. Therefore, it was postulated that enhancements in the cement-stem bond and a decrease in stress at the cement-stem interface by precoating and roughening the proximal stem may contribute to the long-term survival of the cemented femoral component. However, the clinical results of precoated femoral stem have been reported diversely. One such example is Harris Precoat femoral stem (Zimmer, Warsaw, IN, USA) with good medium-term results by few investigators,1) but high failure rates are reported in some studies.2)
Clohisy and Harris3) reported in their study of 100 hips with precoat stem that only one hip had C1 cement mantle which was revised due to aseptic loosening after a mean follow-up of 10 years. Ito et al.1) demonstrated excellent results with 127 Precoat Plus (Zimmer) and CDH Precoat stems (Zimmer) with none showing any loosening at a mean follow-up of 11 years and of which 45 hips had C2 cement mantle.
In a study by Dowd et al.,4) there were 23 stem failures of 154 Harris Precoat stems (Zimmer) during 4 to 11 years with C2 cement mantle in 17 of 51 failed femoral stems. Sylvain et al.2) reported an average failure of 10 (12%) Centralign stems (Zimmer) at 35.8 months' follow-up and the mode of failure was debonding at the cement-prosthesis interface in all 10 stems. However, the researchers found no statistical difference in the cement grades between the failure group and the non-failure group.
The purpose of this study was to report the long-term outcome of precoated femoral stem and to investigate the factors contributing to survivorship.
On a retrospective basis, we reviewed 136 primary hybrid total hip arthroplasties performed in 121 patients (mean age, 58.6 years; range, 22 to 86 years) between October 1990 and December 1995 by a single senior surgeon. Thirty-nine patients died, but they did not require any additional operation during the follow-up period. Seventeen patients were lost to follow-up; 5 of the patients that died were older than 70 years at the time of their primary surgery. Two patients underwent revision for postoperative infection and hence were excluded from the study. Therefore, collectively 76 cases of 63 patients were available for clinical and radiological reviews until the most recent follow-up.
The mean age of the available group was 46.8 years (range, 22 to 77 years) with a mean follow-up of 15.5 years (range, 14 to 19.5 years). Male to female ratio was 44:19 (54 and 22 hips). All hips were implanted with precoated stems (Harris Precoat Plus in 33 cases and Centralign in 43 cases). The acetabular components in these 76 hips comprised of 70 Harris-Galante Prosthesis (HGP) acetabular cups (58 patients; Zimmer) and 6 cementless CLS Spotorno expansion cups (5 patients, Zimmer). The diagnosis of the patients at the time of surgery was osteonecrosis of femoral head in 46 patients (58 cases), degenerative osteoarthritis in 8 patients (8 cases), developmental hip dysplasia in 3 patients (4 cases), rheumatoid arthritis in 3 patients (3 cases), Legg-Calve-Perthes disease sequelae in 2 patients (2 cases) and post-septic hip sequelae in one patient (1 case).
A single surgeon operated on all of the hips by use of a postero-lateral incision. Acetabular bed preparation was done with 0-2 mm concentric under-reaming. HGP acetabular cups (HGP I and HGP II) were implanted using 1-3 screws and expansion cups were implanted without screw. In 69 cases, 28 mm cobalt chrome alloy metal heads were used, and 22 mm metal heads were used in 7 female cases with ultra-high molecular polyethylene liners. The surgeon employed a third generation cementing technique using Palacos cement mixed with a vacuum mixing system that was employed with cement inserted and pressurized using a cement gun. Stem centralizers were not used. Postoperative rehabilitation involved having patients stand from the second or third postoperative day and walk with crutch support for 3 to 4 weeks after the operation.
In our institution, all primary total hip arthroplasty patients are followed-up in the postoperative period at the following time points: 1 month, 3 months, 6 months, 12 months, and yearly thereafter. We evaluated the cementing technique in the follow-up radiographs in accordance with the system proposed by Barrack et al.5) and modified by Mulroy et al.6) Anteroposterior and translateral radiographs taken during the follow-up period were reviewed to analyze the stem failure by the mode of loosening, as delineated by Gruen et al.7) A periprosthetic fracture or osteolysis around the stem were recorded as well. We defined radiographic loosening according to the criteria proposed by Harris et al.8)
Statistical analysis was performed using the SPSS ver. 12 (SPSS Inc., Chicago, IL, USA). Pearson's chi-square test and Fisher's exact test were used for determining the association of patient variables (age and gender) with aseptic loosening of the femoral stem. In addition, the prevalence of aseptic loosening according to cement grade was evaluated. The Kaplan-Meier survivorship method was employed to evaluate the survival of the femoral stem with radiographic aseptic loosening as the endpoint for stem failure. In addition, acetabular component survival was assessed using the same method with a standard endpoint being isolated liner exchange due to severe wear and osteolysis or reoperation for any reason except infection.
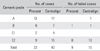
Analysis of the postoperative radiographs taken after the initial surgical procedure in 76 hips showed 30 stems with cement grade A (39.5%), 16 stems with cement grade B (21.1%), 6 stems with cement grade C1 (7.9%) and 24 stems with cement grade C2 (31.6%) and no stem with cement grade D. Twenty-one of the 24 failed stems had C2 cement mantle in the postoperative radiograph (Table 1). We compared stems with cement grade A and B to those with cement grade C1 and C2.
Twenty-four femoral stems of 23 patients showed failure in the form of aseptic loosening as seen on radiographs (10 cases of Precoat Plus and 14 cases of Centralign). Twenty-three failed stems were revised at an average revision time of 8 years (range, 3 to 14.8 years) after initial surgery. The average revision time for Precoat Plus stem was 9.2 years (range, 4.3 to 14.8 years) and for Centralign stem was 7.3 years (range, 3 to 12.3 years). There was no statistical difference of stem loosening between Precoat Plus and Centralign stems (p = 0.13). There were 3 cases of periprosthetic fractures with severe osteolysis (1 case of Precoat Plus and 2 cases of Centralign). There was no hip that showed lysis around femoral stem in the remaining hips. The remaining 52 hips in the study showed no evidence of aseptic loosening of the femoral component or lysis around the stem. One failed stem was not revised.
Twenty-two of the 24 loosened stems demonstrated a course of failure in accordance with the Harris' criteria with initial radiographic evidence of debonding at the cement-stem interface in zone 1 followed by radiographic loosening of the femoral stem with osteolysis around cement mantle (Fig. 1). Two stems showed true cement-bone interface failure.
Twenty-three acetabular reoperations were reported in this study. Twelve of these were isolated acetabular liner exchange due to severe wear and osteolysis. In the remaining 11 reoperations, 5 revisions were due to aseptic loosening (5 HGP cups), 4 were due to severe lysis or metallosis (4 HGP cups), one case of liner dissociation with acetabular cup was noted (1 HGP cup), and one case of revision was due to fracture of the metal shell of acetabular cup (1 expansion cup). The average duration for the revision of the acetabular components was 11.8 years (range, 6.5 to 19.1 years) and for isolated liner exchange was 11.3 years (range, 7.3 to 16.9 years).
There were two patients who underwent revision for both femoral and acetabular components, though the femoral components were well fixed at the time of acetabular reoperation.
No significant difference in the cement grades between Precoat Plus and Centralign femoral stems was found in our study (Fisher's exact test, p = 0.757). However, a significant association was found between cementing grade and aseptic loosening of the cemented femoral stem (Fisher's exact test, p < 0.001).
The prevalence of stem loosening in the age under 49 years old were 34.8% (15 out of 43 cases), and that in the age over 50 years was 27.3% (9 out of 33 cases). Age was not found to be significantly associated with aseptic loosening of the stem (Fisher's exact test, p = 0.47), even though majority of the cases with aseptic loosening aged below 60 years at the time of surgery. However, there was a statistical association of gender with aseptic loosening of the cemented femoral stem (Pearson's chi-square test, p = 0.005). There were two stem loosening cases (9.1%) in female patients (22 cases in total), but 22 cases (40.7%) in male patients (54 cases in total). Stem loosening was more frequent in male patients.
Kaplan-Meier survivorship analysis of femoral stem using radiographic aseptic loosening as the endpoint for failure showed survival rate for Precoat Plus stem as 76.9% at 10 years (95% confidence interval [CI], 68.6 to 85.2) and 61.5% at 19 years (95% CI, 51.7 to 71.3). The mean survival of Precoat Plus stem was 15.8 years (95% CI, 13.7 to 18.0). Survival rate for Centralign stem was 76.2% at 10 years (95% CI, 69.6 to 82.8) and 64.3% at 19 years (95% CI, 56.9 to 71.7) (Fig. 2). The mean survival of Centralign stem was 14.5 years (95% CI, 12.9 to 16.0). There was no statistical difference of survival between two stems (log rank test, p = 0.88).
The survival rate for combined Precoat Plus and Centralign femoral stems was 76.5% at 10 years (95% CI, 71.4 to 81.6) and 63.2% at 19 years (95% CI, 57.3 to 69.1). The mean survival time of two stems was 15.8 years (95% CI, 14.5 to 17.2).
The survival rate of HGP acetabular component using acetabular reoperation for any reason including isolated liner exchange was 91.5% at 10 years (95% CI, 88.2 to 94.8) and 56.7% at 19 years (95% CI, 45.2 to 68.2) (Fig. 3). The mean survival time of acetabular component was 17.3 years (95% CI, 16.4 to 18.4).
The concept of precoating was evolved from the fact that cement-metal interface is substantially weaker than the bulk cement itself and precoating the stem will result in increasing the strength of this weak interface. But controversy still exists on the optimal surface finish of the femoral stem in cemented total hip arthroplasty. We are still finding an answer to whether rough surfaces with precoated stem function better in terms of survival or in fact may contribute to the loosening of femoral stems. The purpose of this discussion is to address this issue.
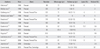
Past several studies1-4,9-16) suggest excellent short- to mid-term survival rates of precoated stem (Table 2). In case of early loosening it becomes important to assess all the causes pertinent to failure because of the well-known fact that aseptic loosening is multi-factorial and includes cementing techniques, stem design, surface roughness, neck length, patient factors like age, gender, and activity level.
Ong et al.14) used both uncoated and precoated stems with a second-generation cementing technique in the similar patient groups and reported a lower failure rate of 3.9% (10 in 256 stems) at a mean of 9.9 years in the uncoated stem (Harris Design II, Howmedica, East Rutherford, NJ, USA) and suggested the design and surface treatment of the femoral stem, including the increased surface roughness and precoating as an important element in causing failure. Another study reported approximately the same failure rate (4% failure) of Harris Design II stem at 20 to 25 years of follow-up.17) Several clinical studies have shown an increased rate of aseptic loosening with proximally roughened cemented stems as compared to that of smooth surface stems with the same design.18)
Harrias Design II stem bears the similar geometry as Precoat or Precoat Plus, but it is neither textured nor precoated, and it has a surface roughness of 33 micro-inch Ra. Ra, the most commonly used roughness parameters, is the arithmetic mean and represents the average of all peaks and valleys. Lower numbers indicate a smooth finish. Up to 30-40 micro-inch Ra of matte surface finishing can be classified as smooth surface19) which is quite distinct from 80-87 micro-inch Ra of precoated stem.
Sylvain et al.2) found in their study that small sized stems with inadequate length progress towards failure. Harrington et al.20) observed stem size is an important factor in reducing the peak tensile strains, in the proximal cement mantle. In addition, Thien and Karrholm21) noted that smallest sized hips are at a higher risk for requiring additional revision. Davey et al.22) suggested that with the less femoral stem offset a higher muscular forces are required theoretically, which may lead to higher hip joint loads and stresses at the cement-stem and cement-bone interfaces and increased risk of loosening subsequently. In addition, Bourne et al.23) observed a decrease in the bone cement pressure on moving to a small stem from a large stem and concluded that this decrease in bone cement pressure may in turn influence the fixation. In our series, smaller size stems were used since most of the patients were younger with a narrow femoral canal, as found with a type-A morphology, as described by Dorr et al.24) Hence it can be assumed that small sized stems may prove to be one of the reasons for a high failure rate reported with the precoated femoral stem in our series.
Cannestra et al.25) compared standard straight stem with cobra-shaped Iowa stem and it was suggested that stem geometry and shape are important with the curved stem showing greater tendency for malposition due to increased offset and this creates an inadequate cement mantle in Gruen zone 3 or 5. In addition, we observed inadequate cement mantle defect on anteroposterior radiographs in our series in both Precoat Plus and Centralign stems, as these are more curved (increased offset compared to their length of stem) which can be compared with Omnifit (Stryker, New Brunswick, NJ, USA) stems which showed better clinical results even with rough surface.
Mohler et al.10) found a unique pattern of loosening in their study of Iowa stem, whereby the implant debonded from its cement mantle as manifested by enlarging radioluceny in Gruen zone 1 and hypothesized that the circular cross-section was less resistant; the authors concluded that this lead to the debonding of the stem-cement interface. A similar pattern of loosening in our series was witnessed in the Harris Precoated stem in the form of debonding in Gruen zone 1 developing several years after total hip arthroplasty followed by appearance of osteolysis a few years later, as an enlarging radiolucency between cement-stem interface in the area of thin cement mantle. Finally, lysis progressed enough to induce stem loosening or fracture of the cortical bone surrounding the stem (Fig. 3). It can be suggested that radiographic evidence of debonding in the precoated femoral stem is an indication towards the beginning of an initial failure between cement-stem interface with subsequent high risk for failure of fixation especially in the femoral stem that had proximal macrotexturing.
The quality of the cement mantle is important for stem fixation. Kawate et al.13) reported that loosening and lysis of Precoat stem occurred in thin cement mantle. However, several studies reported that there is no correlation between the radiographic grade of the cement mantle and the risk of failure of the Harris matte-finish and precoated femoral stems. Woolson and Haber12) in their study of 6 years follow-up reported good results with a low failure rate in the presence of thin cement mantle. Although, experimental studies point to the fact that thin cement mantle is a contributory factor for failure of the femoral component or lysis. We agree strongly with the observations of Olofsson et al.26) that the patients classified as having C2 cement grade had more subsidence than the patients who had other grades of cement mantle. Furthermore, it has been suggested that patients with C2 cement grade had stems that debond more easily from the mantle. In addition, we witnessed a C2 cement mantle in all except 3 cases of failed hips.
Ebramzadeh et al.27) described errors in radiographic assessment for cementing grade. They indicated that even with strict adherence to radiographic techniques, radiographs may include some distortion due to rotation of the stem, or due to variations in the amount of the limb relative to the anteversion of the femoral neck. Hank et al.28) stressed the importance of lateral radiographs in analysing cement mantle with a probability of underestimating thin and deficient cement mantles on plain AP films. Based on our experience, we found that measurement of the cement thickness was affected more in cases of a rectangular shaped Precoat Plus or Centralign femoral stem in general cross-sectional geometry than a round shaped even with little rotation. In our study, subtle change in hip rotation resulted in changes in the thickness of cement mantle in zones 9 and 13 on lateral view.
Precoat Plus and Centralign femoral stem are not anatomic stems and thus carry an intrinsic risk of a thin cement mantle, especially in Gruen zones 8 and 9 or zone 12 in absence of a centralizer. We observed C2 cement mantle occasionally in Gruen zone 2, 3, or 5 on antero-posterior radiographs and in zone 9 or 12 on lateral radiographs. The presence of a Centralign femoral stem did not reduce the thin cement mantle in the femoral canal, which was in contrast with other series.21) Breusch et al.29) also demonstrated that centralizers were efficient to prevent thin cement mantle in distal part but no effect proximally and Kawate et al.30) reported ineffective design of the distal centralizer to be responsible for insufficient cement mantles.
There is some controversy about the influence of gender on stem loosening. Some studies reported that male gender is one of risk factors for the development of osteolysis, but others found no such association. In our study, stem loosening was approximately three times more frequent in male patients. Activity level plays a significant role in prosthesis survival. In addition, higher muscular forces in men and anatomic differences should be taken into consideration, as well as the influence of higher mean body mass index.
In the end, it can be concluded that Harris Precoat stem (Precoat Plus and Centralign) demonstrated early failure in presence of inadequate cement mantle in our study. All the failed stems that were found on radiology to be loose in our study definitely had a deficient cement mantle that led to debonding at the cement-stem interface and subsequent failure, even though the cement-bone interface was intact in all the failed cases. Few non-failed stems had C2 cement mantle (only 3 in 52), hence a statistical correlation was not possible between C2 cement grade and the non-failed stems in our study.
The main limitation in our study was the less number of available hips (76 of 136 cases, 55%) in the final follow-up, since almost 30% (39 patients, 40 hips) were not available for final follow-up due to deaths (mostly more than 65 years at the time of primary surgery), which is a common situation in this country in older patients; however, none of these underwent any reoperation of either the femoral or acetabular component in the available short- to medium-term follow-up and 17 patients (18 cases, 13%) were lost to follow-up.
Our results suggest that a well performed cementing technique can result in successful long-term survival of precoated femoral stem designs as evident in our study in which 38 of 51 hips (74.5%) having a good cement mantle (either grade A or grade B) showed no evidence of loosening or failure at 15 years mean follow-up. It can be said that precoated stem designs may be different from other cemented stems in terms of increased sensitivity to thin cement mantle mainly because of its geometry, which increases the strain at the cement mantle leading to eventual loosening. Finally, we should also consider the exact mechanism of failure of precoat stems as well as the contributing factors before coming to a conclusion.
Figures and Tables
Fig. 1
Follow-up radiographic images of a 32-year-old male with osteonecrosis of femoral head. (A) Postoperative radiograph of C2 cement mantle in Gruen zone 3. (B) Radiograph at 3 years follow-up demonstrating debonding in Gruen zone 1. (C) Radiographs at 6.2 years follow-up showing definitive loosening and lysis around C2 cement mantle (Gruen zones 3, 5, and 12). On translateral view, debonding was seen in Gruen zone 10, and osteolysis in Gruen zone 12.

Fig. 2
Kaplan-Meier survival rate for Precoat Plus and Centralign femoral stem was calculated using revision of the femoral stem for aseptic loosening as the endpoint. The survival rate at 19 years was 61.5% (95% confidence interval [CI], 51.7 to 71.3) in Precoat Plus stem and 64.3% (95% CI, 56.9 to 71.7) in Centralign stem.
References
1. Ito H, Matsuno T, Minami A. Pre-coated femoral components in hybrid total hip arthroplasty: results at 11 years. J Bone Joint Surg Br. 2005. 87(3):306–309.
2. Sylvain GM, Kassab S, Coutts R, Santore R. Early failure of a roughened surface, precoated femoral component in total hip arthroplasty. J Arthroplasty. 2001. 16(2):141–148.

3. Clohisy JC, Harris WH. Primary hybrid total hip replacement, performed with insertion of the acetabular component without cement and a precoat femoral component with cement: an average ten-year follow-up study. J Bone Joint Surg Am. 1999. 81(2):247–255.

4. Dowd JE, Cha CW, Trakru S, Kim SY, Yang IH, Rubash HE. Failure of total hip arthroplasty with a precoated prosthesis: 4- to 11-year results. Clin Orthop Relat Res. 1998. (355):123–136.
5. Barrack RL, Mulroy RD Jr, Harris WH. Improved cementing techniques and femoral component loosening in young patients with hip arthroplasty: a 12-year radiographic review. J Bone Joint Surg Br. 1992. 74(3):385–389.

6. Mulroy WF, Estok DM, Harris WH. Total hip arthroplasty with use of so-called second-generation cementing techniques: a fifteen-year-average follow-up study. J Bone Joint Surg Am. 1995. 77(12):1845–1852.

7. Gruen TA, McNeice GM, Amstutz HC. "Modes of failure" of cemented stem-type femoral components: a radiographic analysis of loosening. Clin Orthop Relat Res. 1979. (141):17–27.
8. Harris WH, McCarthy JC Jr, O'Neill DA. Femoral component loosening using contemporary techniques of femoral cement fixation. J Bone Joint Surg Am. 1982. 64(7):1063–1067.

9. Oishi CS, Walker RH, Colwell CW Jr. The femoral component in total hip arthroplasty: six to eight-year follow-up of one hundred consecutive patients after use of a third-generation cementing technique. J Bone Joint Surg Am. 1994. 76(8):1130–1136.

10. Mohler CG, Callaghan JJ, Collis DK, Johnston RC. Early loosening of the femoral component at the cement-prosthesis interface after total hip replacement. J Bone Joint Surg Am. 1995. 77(9):1315–1322.

11. Goldberg VM, Ninomiya J, Kelly G, Kraay M. Hybrid total hip arthroplasty: a 7- to 11-year followup. Clin Orthop Relat Res. 1996. (333):147–154.
12. Woolson ST, Haber DF. Primary total hip replacement with insertion of an acetabular component without cement and a femoral component with cement: follow-up study at an average of six years. J Bone Joint Surg Am. 1996. 78(5):698–705.

13. Kawate K, Ohmura T, Nakajima H, Takakura Y. Distal cement mantle thickness with a triangular distal centralizer inserted into the stem tip in cemented total hip arthroplasty. J Arthroplasty. 2001. 16(8):998–1003.

14. Ong A, Wong KL, Lai M, Garino JP, Steinberg ME. Early failure of precoated femoral components in primary total hip arthroplasty. J Bone Joint Surg Am. 2002. 84(5):786–792.

15. Lachiewicz PF, Messick P. Precoated femoral component in primary hybrid total hip arthroplasty: results at a mean 10-year follow-up. J Arthroplasty. 2003. 18(1):1–5.

16. Jarrett SD, Lachiewicz PF. Precoated femoral component with proximal and distal centralizers: results at 5 to 12 years. J Arthroplasty. 2005. 20(3):309–315.
17. Skutek M, Bourne RB, Rorabeck CH, Burns A, Kearns S, Krishna G. The twenty to twenty-five-year outcomes of the Harris design-2 matte-finished cemented total hip replacement: a concise follow-up of a previous report. J Bone Joint Surg Am. 2007. 89(4):814–818.

18. Grose A, Gonzalez Della, Bullough P, Lyman S, Tomek I, Pellicci P. High failure rate of a modern, proximally roughened, cemented stem for total hip arthroplasty. Int Orthop. 2006. 30(4):243–247.

19. Crowninshield RD, Jennings JD, Laurent ML, Maloney WJ. Cemented femoral component surface finish mechanics. Clin Orthop Relat Res. 1998. (355):90–102.

20. Harrington MA Jr, O'Connor DO, Lozynsky AJ, Kovach I, Harris WH. Effects of femoral neck length, stem size, and body weight on strains in the proximal cement mantle. J Bone Joint Surg Am. 2002. 84(4):573–579.

21. Thien TM, Karrholm J. Design-related risk factors for revision of primary cemented stems. Acta Orthop. 2010. 81(4):407–412.

22. Davey JR, O'Connor DO, Burke DW, Harris WH. Femoral component offset: its effect on strain in bone-cement. J Arthroplasty. 1993. 8(1):23–26.
23. Bourne RB, Oh I, Harris WH. Femoral cement pressurization during total hip arthroplasty: the role of different femoral stems with reference to stem size and shape. Clin Orthop Relat Res. 1984. (183):12–16.

24. Dorr LD, Faugere MC, Mackel AM, Gruen TA, Bognar B, Malluche HH. Structural and cellular assessment of bone quality of proximal femur. Bone. 1993. 14(3):231–242.

25. Cannestra VP, Berger RA, Quigley LR, Jacobs JJ, Rosenberg AG, Galante JO. Hybrid total hip arthroplasty with a precoated offset stem: four to nine-year results. J Bone Joint Surg Am. 2000. 82(9):1291–1299.
26. Olofsson K, Digas G, Karrholm J. Influence of design variations on early migration of a cemented stem in THA. Clin Orthop Relat Res. 2006. 448:67–72.

27. Ebramzadeh E, Sarmiento A, McKellop HA, Llinas A, Gogan W. The cement mantle in total hip arthroplasty: analysis of long-term radiographic results. J Bone Joint Surg Am. 1994. 76(1):77–87.

28. Hank C, Schneider M, Achary CS, Smith L, Breusch SJ. Anatomic stem design reduces risk of thin cement mantles in primary hip replacement. Arch Orthop Trauma Surg. 2010. 130(1):17–22.





 PDF
PDF ePub
ePub Citation
Citation Print
Print


 XML Download
XML Download