Abstract
Background
Intertrochanteric fractures of the femur are the most common type of fracture, and are an increasing occurrence due to the aging of the population. The objectives of our study are to predict the fate of intertrochanteric fractures treated with intramedullary hip nails by assessing the postoperative fracture stability utilizing the newly developed scoring system, and to help rehabilitate these patients.
Methods
Eighty-two patients with intertrochanteric fractures that were treated with intramedullary hip nails between December, 2004 and January, 2011 were subjected to this study. The patients who could be followed for a minimum of one year postoperatively were enrolled. The immediate postoperative conditions were determined by radiograms: reduction status (3 parameters/4 points: contact accuracy of posteromedial cortex, severity of angulation, and distraction), fixation status (3 parameters/3 points: tip-apex distance, location of tip of the lag screw, entry point of the intramedullary nail), and fracture type (1 parameter/1 point: stable or unstable type by the Kyle's classification). Postoperative reduction loss and fixation failure were checked by radiograms taken at a minimum 3 months postoperative.
Results
Reduction loss and fixation failure were observed in 14 consecutive patients (17%). The fixation failure rate was 100% (2 patients) in score 1, 60% (3 out of the 5 patients) in score 2, 39% (3 out of the 8 patients) in score 3, and 50% (4 out of the 8 patients) in score 4 groups. There were fixation failures only in 1 out of 13 patients with score 5, and in 1 out of 18 patients with score 6. There was no fixation failure in 17 patients with score 7 and 11 patients with score 8.
Intertrochanteric fractures of the femur are the most common type of fracture and are an increasing occurrence in an aging population.1) Unstable peritrochanteric fractures are difficult to fix and present problems in management. We advocate the Arbeitsgemeinschaft für Osteosynthesefragen (AO)/Association for the Study of Internal Fixation (ASIF) principle of accurate anatomic reduction and stable internal fixation in the management of intertrochanteric fractures and apply this principle in the management of these cases in our practice. Based on previously reported high morbidity and management-related complications in patients with this fracture, various internal fixation devices and operative techniques have been developed to reduce management-associated complications.2-4) Currently, the most frequent devices used to manage this condition have been sliding compression hip screws with side plate assemblies including dynamic hip screw (DHS; Synthes, Paoli, PA, USA) and intramedullary fixation devices including proximal femur nail (PFN; Synthes) and gamma nail (GN; Stryker, Mahwah, NJ, USA). Although there have been controversies in the selection of the preferred fixation device, the intramedullary fixation devices have become increasingly popular due to the proven biomechanical and biological advantages.5-9) Numerous improved operative techniques with the newer intramedullary fixation devices have been introduced as well.10) That is, in an effort to reduce the incidence of intra- and/or postoperative complications, the 2 basic approaches that have been taken: design modification of the implant and modified reduction technique to achieve greater stability. The device must stabilize the fracture against deforming forces until union establishment.
The fracture pattern, bone density and comorbidities in the patients were the uncontrollable factors in reducing the surgery-related complication rate. However, the surgery-related complications could be reduced by the advanced surgical management utilizing the new fixation devices and improved operative techniques, and consequently the hospitalization period also could be reduced.
To assess the immediate postfixation fracture stability and to provide the favored early postoperative safe and reliable patient's mobilization, a new fixation stability score system was developed on basis of the immediate postoperative radiographic findings. But the permissible degree of postoperative weight-bearing was depended entirely on the accuracy of the reduction and the stability of the fixation. Therefore, the objective of this study was to assess the validity of a newly developed fixation stability score system in managing postoperatively the patients with these fractures, and secondly to help rehabilitate the patients earlier without complications.
On a retrospective basis, we analyzed the records of 129 patients who had undergone osteosynthesis with combined intramedullary nail and a sliding hip screw (GN3, PFN and proximal femoral nail anti-rotation [PFNA], Synthes) for the management of the intertrochanteric fractures between December 2004 and January 2011. The exclusion criteria were: 1) patients that were not ambulatory on a pre- and postoperative basis; 2) patients that did not have a postoperative radiogram by 3 months postoperative; and 3) patients associated with concurrent femoral shaft fracture including intraoperative iatrogenic occurrence. In final, we enrolled 82 patients overall after excluding 47 of the 129 consecutive intertrochanteric fracture patients screened for study eligibility. Patient mean age was 71 years and 3 months (range, 33 to 91 years). Of patients enrolled into the study, 48 patients (59%) were female and 34 patients (41%) were male. The mean follow-up period was 17 months (range, 12 to 67 months).
The fractures were classified after the Kyle's classification into the stable (type I, II) or unstable fractures (type III, IV); 39 stable and 43 unstable fractures. Each of all patients had closed reduction and internal fixation, and all patients were postoperatively permitted to sit up in bed within a week, to stand and walk from postoperative 1 to 4 weeks, based on the patient's postoperative general and/or fracture stability.
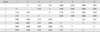
Postoperative fixation stability was assessed by the authors' surgical technique-oriented fixation stability score system. A total of 7 parameters were selected from the fracture type and the various operative techniques with the selected intramedullary fixation devices to assess the postosteosynthesis fracture stability. Six of the 7 parameters were selected as the surgical technique-oriented factors, based on the AO/ASIF principle: anatomical reduction and stable fixation. The parameters for assessing anatomical reduction were: 1) bony contact of posteromedial cortex of trochanteric portion, 2) angulation and 3) distraction, and the parameters for assessing the stable fixation were 4) tip-to-apex distance (TAD), 5) entry point of the intramedullary nail, and 6) location of the tip of the lag screw. To record the position of the tip of the lag screw in the femoral head, the head was divided into 9 regions according to "the Cleveland index".11) These parameters were analyzed utilizing immediate postoperative anteroposterior (AP) and lateral radiograms (Fig. 1). The seventh parameter was the fracture type by the Kyle's classification. This final parameter analysis was derived from preoperative AP and lateral radiograms (Table 1).
One point was set at the each parameter, with the exception of the contact pattern of posteromedial cortex for which 2 points were given because of its mechanical importance. One point was given to each remaining factor: a TAD less than 25 mm, location of entry point at slight medial or the exact tip of the greater trochanter, location of the tip of the lag screw at Cleveland index 5, 6, 8, 9 region, non-permissible distraction, angulation less than 5 degrees, and stable fracture type (Kyle's classification type I or II). Two points were given when posteromedial cortical contact was completely obtained in the AP and lateral radiographs, while zero points were given when the contact was not obtained. When even minimal longitudinal gaps of all 4 cortices were seen on the immediate postoperative plan AP and lateral radiograms, the fracture was defined to be distracted.
The fracture union was assessed by the sealing callus on all around the cortices including anterior, posterior, medial, and lateral surfaces. The presence of calluses on 3 cortices was deemed as evidence of union. The fracture was considered to have failed fixation when there was over 5° varus collapse of the neck-shaft angle or cut-out of lag screw through the femoral head, downward lag screw back-out or reduction loss of the posteromedial cortex, or the internal fixation device failure. The definition of early and late collapse was made when the fixation failed before and after postoperative 3 months on basis of the other previously reported average union time of 3 months. The bone mineral density (BMD) was measured in the 9 fixation failure patients (mean age, 76 years), and as control, 29 patients without fixation failure (mean age, 75 years) were used. We failed to obtain BMD data in the rest of patients due to missing radiogram studies or examination refusal. Another reason was that the study was not used in patients of a young age. An additional limitation of this study was that it was performed on a retrospective basis.
The data analysis was performed using SPSS ver. 19 (IBM Co., Armonk, NY, USA). The fixation failure rate at each score was calculated, and correlations between the rate and each score were analyzed using Spearman's correlation. The Spearman's correlation coefficient (r) was interpreted as poor if < 0.30, fair if 0.31-0.50, moderate if 0.51-0.60, moderately strong if 0.61-0.80, and very strong if ≥ 0.81. The fixation failure rate, based on the assessed scores in subgroups was compared using Fisher's exact test. T-score of the bone mass density between the fixation failure patients and the others were compared using independent samples t-test.
In addition, the current authors analyzed the difference in the stability score using one-way ANOVA and failure rate using Fisher's exact test among 3 types of implants, and analyzed each parameter if that independently affected the fixation failure using Fisher's exact test. An intraclass correlation coefficient (ICC) was calculated for assessment of the intraobserver and interobserver reliability. The scores of all 82 patients were measured in one month intervals by 3 orthopaedic surgeons for the evaluation of interobserver and intraobserver reliability. A p-value less than 0.05 was considered statistically significant.
This study was approved by the Institutional Review Board of the author's institute.
Fixation failures were observed in 14 out of total 82 patients (17%). The fixation failed in only 1 out of 39 patients (3%) with the Kyle's stable type I and II fractures, whereas the fixation failed in 13 out of 43 patients (30%) with the unstable type III and IV fractures. Among 4 out of the 11 patients with early collapse, only varus angulation of neck-shaft angle over 5° was observed. The loss of posteromedial cortical contact by sliding of the lag screw in 4 patients, and the femoral head cut-out by lag screw in 3 patients were complicated, respectively (Fig. 2). The late collapses was complicated in the 3 patients; failure of intramedullary nail in one patient (Fig. 3), the femoral head cut-out by lag screw in one patient, and back-out of the lag screw in one (Fig. 4, Table 2). The early collapse occurred at mean postoperative 3.5 weeks in the 11 out of the 14 fixation-failed patients. The late collapse occurred at postoperative 6, 9, and 10 months in 3 patients, respectively.
The fixation failure rates were 100% in score 1 group (2 patients), 60% in score 2 group (3 out of 5 patients), 39% in score 3 group (3 out of 8 patients), and 50% in score 4 group (4 out of 8 patients). There was fixation failure only in 1 out of 13 patients (8%) with score 5, only 1 out of 18 patients (5.6%) with score 6, and no fixation failure in the 17 patients with score 7 and the 11 patients with score 8 (Fig. 5).
The stability score had a very strong correlation with the fixation failure rate (r = -0.970, p = 0.000, Spearman's correlation). The fixation failure became less in parallel with a significant increase in the stability score. There were significant differences between the groups with scores 1, 2, 4 and the groups with scores over 5 (p < 0.05, Fisher's exact test) (Table 3).
The mean T-score of BMD in 9 cases of the fixation failure was -3.47, and that of the 29 control patients also was -3.00. There were no significant differences in the bone mineral density between the two groups (p = 0.264). There was no significant difference of the stability score at 3 implant types (p = 0.310). The failure rate was also not different among 3 implant types (p = 0.749 between GN and PFN, p = 1.0 between GN and PFNA, and p = 1.0 between PFN and PFNA).
Four out of 7 parameters such as the entry point of the intramedullary nail, contact of posteromedial cortex of trochanteric portion, angulation, and fracture type affected the fixation failure independently. The p-values can be found in Table 4.
Intra- and interobserver reliability were calculated with an ICC. The ICCs for intra- and interobserver reliability were 0.954 and 0.919, respectively. Mean fracture union time was 13 weeks on an average. Diagnosis of delayed union was made in 2 cases at postoperative 6 and 9 months, respectively. A patient who had nonunion at postoperative 10 months underwent a second replacement with a bipolar prosthesis. There was no case of surgical site infection or avascular necrosis of the femoral head.
The incidence of hip fractures has increased with the aging of the population.1) Unstable fractures are difficult to fix, and consequently can present problems in management. To provide better treatment for the hip fracture in the elderly, many newer implants and operative techniques have been developed primarily to make successful osteosynthesis, and secondarily to reduce the surgery-related complications such as fixation failure. Proper selection of the implants for the fracture management has been a controversial issue.12) Some authors insist to perform a primary bipolar hemiarthroplasty instead of osteosynthesis for early mobilization, and to provide the resumption of the comfortable activity of the daily living to the elderly patients postoperatively.13-15)
Even though a meta-analysis disclosed no evidence for a reduced failure rate with intramedullary nails for the unstable intertrochanteric fractures,16) other studies reported that the intramedullary nailing was more advantageous for the fixation of the unstable fracture than extramedullary implants. Thus, in recent years it has become the preferred treatment option.3-7) Based on this information, the importance of operative skills including the anatomical reduction, proper positioning of the intramedullary nail, and the lag screw in bone was emphasized.
There are the known 4 major postoperative complications. Most authors define the fixation failure when the following findings are observed: 1) penetration of the joint by the screw tip associated with concomitant impaction of the fracture fragment, 2) loss of reduction with varus angulation, 3) cutting out of the screw through the head and neck superiorly associated with varus angulation, and 4) device failure (bending or breaking).
Based on the analysis of fixation failure cases, we sought the solutions for successful osteosynthesis. Although the fracture classification varied, most authors used the familiar term "unstable" fracture to imply loss of posteromedial cortical contact. In the current study, anatomical reduction was assessed on the basis of accuracy of posteromedial-cortical buttress contact, angulation of the proximal fragment, and distracted fracture gap. For the establishment of fracture stability, the accurate apposition of the posteromedial cortical buttress was considered to be the most important factor.17,18) At the intertrochanteric level, the resultant joint force acting on the femoral head has 2 major effects; axial compression and bending. The angulated proximal fragment of the femur cannot provide effective force transport on weight-bearing.19-21) Therefore, accurate anatomical reduction through the accurate contact of the posteromedial cortex, restoration of normal neck-shaft angle including coronal, and sagittal planes of the fractured femur are important factors for maintaining the fracture stability until union. The distracted fracture gap is also a risk factor that leads to nonunion and eventual back-out of screw and/or failure of the nail.10)
Proper implant position in bone was determined from the TAD, location of the lag screw tip in the femoral head, and entry point of intramedullary nail. Schipper et al.22) reported that the most common postoperative complication in the PFN and GN osteosynthesis was the femoral head cut-out by the lag screw, which was seemingly caused by the malpositioned lag screw in the head. Such an example was also demonstrated in the current series (Fig. 2). Baumgaertner et al.23) and Baumgaertner and Solberg24) described that TAD is a useful intraoperative indicator, and that a TAD of less than 25 mm had been shown to be generally predictive of a successful result. However, in the current study, there was no significant difference in the fixation failure between the group of the TAD less than 25 mm (4 failed in 27 patients) and the other group (10 failed in 55 patients, p = 1.000). The reported complication rate was low when a lag screw tip was located at 5, 6, 8, 9 regions of Cleveland index.11) Unlike previous reports, there was no significant difference in the fixation failure according to the parameter of the location of the tip of the lag screw (p = 1.000). The fixation failure occurred in 6 out of the 51 patients (12%) with a lag screw in Cleveland index 5, 6, 8, 9 location, whereas 8 out of the 31 patients (26%) of the other regions failed (Table 4). We could not obtain all the other 6 parameters except studied parameter as same condition in this study. This was considered to be the reason for the difference from previously reported results. Each parameter cannot be the sufficient factor, but the necessary factor for success. For example the patient who had stable fracture types, anatomical reduction, and stable fixation, except for only one parameter (location of a lag screw) would not fail, although a lag screw was placed at Cleveland lesion 1.
A starting point slightly medial to the exact tip of the greater trochanter was recommended because reaming of proximal portion could lead to more lateral position of the intramedullary nail.25) Lateral position of the nail at the proximal portion can influence the formation of the varus angulation of the fracture site due to loss of buttress effect of the intramedullary nail and leads to the increased lateral lever arm of the hip joint.
In the Kyle's classification, type I, II fractures are defined as stable; type III and IV fractures with comminution of the posteromedial cortex are defined as unstable.17) In the current authors' series, the Kyle's classification was utilized in initial assessment, and contact of the posteromedial cortex was set as the most important factor from the viewpoint of fracture stability. It is true that obtaining good anatomical reduction and stable fixation are more difficult to achieve in unstable fractures than in stable fractures, and it could lead to fixation failure. For this reason, the fracture type was included in the stability score system as one of the parameters.
With regard to BMD, Jeong et al.26) reported that the BMD in elderly patients with proximal femur fracture was significantly lower than that of the control group. In the current series, most patients had osteoporosis, but there were no significant differences in T-scores of the BMD between the fixation failure group and the other non-failure group (p = 0.264). It was thought that subdivision of the group based on the T-score could lead our stability score system to be more complicated. Therefore, the T-score of the BMD was not referenced in assessing the fracture fixation stability in our scoring system.
The current study has several limitations. First, this was a retrospective study and could not present the exact rehabilitation programs, such as the proper time to stand and walk. We could not obtain the result of BMD for all patients because one of the retrospective nature of the current study. A second limitation is the small number of the fixation failure cases as part of the study. For this reason, the failure rate at the group of score 3 was not significantly different from that of the group over score 5. A prospective study with a large number of participants and well-formulated postoperative rehabilitation program using this stability score system would help establish the postoperative management program of this type of fractures. However, it must be remembered that the definition of failure is not universal. The newly devised fixation stability score correlated strongly with the fixation failure rate, and the groups with score over 5 had significantly decreased the fixation failure rate.
In conclusion, the fixation stability score of the intertrochanteric fracture treated with intramedullary nails is a useful tool for the clinicians to predict accurately, the maintenance of the fracture fixation until the union and to prescribe the most suitable postoperative rehabilitation program.
Figures and Tables
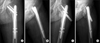
Fig. 1
The 6 parameters of the stability score system except fracture type parameter. Immediate postoperative anteroposterior (A) and lateral (B) radiographs show a total stability score of 7. (1) Bony contact of posteromedial cortex of trochanteric portion was obtained. There was no (2) angulation or (3) distraction. (4) Tip-to-apex distance was 22 mm. (5) Entry point of intramedullary nail was located at the tip of the greater trochanter and (6) the lag screw tip was located at the Cleveland 5.

Fig. 2
Fixation failure case 1. (A, B) Immediate postoperative radiographs at Kyle's type III fracture show a total stability score 1. Tip-to-apex distance 35 mm, superolateral location of the lag screw tip, lateral entry point, and varus angulation were noted with loss of posteromedial cortex contact. (C, D) After 1 month, cut-out of the lag screw through the femoral head and varus collapse were noticed.

Fig. 3
Fixation failure case 2. (A, B) Immediate postoperative radiographs at Kyle's type III fracture show a total stability score of 3. Valgus angulation and distraction were noted with loss of contact of posteromedial cortex. (C, D) After 10 months, the intramedullary nail was broken and the hip joint was treated with hemiarthroplasty.

Fig. 4
Fixation failure case 3. (A, B) Immediate postoperative radiographs at Kyle's type III fracture show a total stability score of 2. Tip-to-apex distance 45 mm, valgus angulation and anterior location of the lag screw tip are noted with loss of posteromedial cortex contact. (C, D) Postoperative 6 months radiographs show back-out of the sliding hip screw and cut-out of anti-rotational pin in the head with varus collapse.
References
1. Kim DH, Lee SH, Ha SH, You JW. Changes in patient pattern and operation methods for intertrochanteric fractures. J Korean Orthop Assoc. 2011. 46(1):49–53.

2. Richmond J, Aharonoff GB, Zuckerman JD, Koval KJ. Mortality risk after hip fracture. J Orthop Trauma. 2003. 17(1):53–56.

3. Albareda J, Laderiga A, Palanca D, Paniagua L, Seral F. Complications and technical problems with the gamma nail. Int Orthop. 1996. 20(1):47–50.

4. Friedl W, Colombo-Benkmann M, Dockter S, Machens HG, Mieck U. Gamma nail osteosynthesis of per- and subtrochanteric femoral fractures: 4 years experiences and their consequences for further implant development. Chirurg. 1994. 65(11):953–963.
5. Utrilla AL, Reig JS, Muñoz FM, Tufanisco CB. Trochanteric gamma nail and compression hip screw for trochanteric fractures: a randomized, prospective, comparative study in 210 elderly patients with a new design of the gamma nail. J Orthop Trauma. 2005. 19(4):229–233.

6. Curtis MJ, Jinnah RH, Wilson V, Cunningham BW. Proximal femoral fractures: a biomechanical study to compare intramedullary and extramedullary fixation. Injury. 1994. 25(2):99–104.

7. Hardy DC, Descamps PY, Krallis P, et al. Use of an intramedullary hip-screw compared with a compression hip-screw with a plate for intertrochanteric femoral fractures: a prospective, randomized study of one hundred patients. J Bone Joint Surg Am. 1998. 80(5):618–630.

8. Bojan AJ, Beimel C, Speitling A, Taglang G, Ekholm C, Jonsson A. 3066 consecutive gamma nails: 12 years experience at a single centre. BMC Musculoskelet Disord. 2010. 11:133.

9. Anglen JO, Weinstein JN. American Board of Orthopaedic Surgery Research Committee. Nail or plate fixation of intertrochanteric hip fractures: changing pattern of practice. A review of the American Board of Orthopaedic Surgery Database. J Bone Joint Surg Am. 2008. 90(4):700–707.

10. Haidukewych GJ. Intertrochanteric fractures: ten tips to improve results. Instr Course Lect. 2010. 59:503–509.
11. Cleveland M, Bosworth DM, Thompson FR, Wilson HJ Jr, Ishizuka T. A ten-year analysis of intertrochanteric fractures of the femur. J Bone Joint Surg Am. 1959. 41-A(8):1399–1408.

12. Lorich DG, Geller DS, Nielson JH. Osteoporotic pertrochanteric hip fractures: management and current controversies. Instr Course Lect. 2004. 53:441–454.
13. Jung HJ, Choi JY, Shin HK, et al. Comparison between results of internal fixation and hemiarthroplasty in unstable intertrochanter fracture of osteoporotic bone. J Korean Fract Soc. 2007. 20(4):291–296.

14. Green S, Moore T, Proano F. Bipolar prosthetic replacement for the management of unstable intertrochanteric hip fractures in the elderly. Clin Orthop Relat Res. 1987. (224):169–177.

15. Haentjens P, Casteleyn PP, Opdecam P. Primary bipolar arthroplasty or total hip arthroplasty for the treatment of unstable intertrochanteric and subtrochanteric fractures in elderly patients. Acta Orthop Belg. 1994. 60:Suppl 1. 124–128.
16. Jones HW, Johnston P, Parker M. Are short femoral nails superior to the sliding hip screw? A meta-analysis of 24 studies involving 3,279 fractures. Int Orthop. 2006. 30(2):69–78.

17. Kyle RF, Gustilo RB, Premer RF. Analysis of six hundred and twenty-two intertrochanteric hip fractures. J Bone Joint Surg Am. 1979. 61(2):216–221.

18. Park SY, Yang KH, Yoo JH, Yoon HK, Park HW. The treatment of reverse obliquity intertrochanteric fractures with the intramedullary hip nail. J Trauma. 2008. 65(4):852–857.

19. Harrington IJ. Gozna ER, Harrington IJ, Evans DC, editors. Biomechanics of joint injuries. Biomechanics of musculoskeletal injury. 1982. Baltimore, MD: Williams & Wilkins;39–51.
20. Lindskog DM, Baumgaertner MR. Unstable intertrochanteric hip fractures in the elderly. J Am Acad Orthop Surg. 2004. 12(3):179–190.

21. Shukla S, Johnston P, Ahmad MA, Wynn-Jones H, Patel AD, Walton NP. Outcome of traumatic subtrochanteric femoral fractures fixed using cephalo-medullary nails. Injury. 2007. 38(11):1286–1293.

22. Schipper IB, Steyerberg EW, Castelein RM, et al. Treatment of unstable trochanteric fractures: randomised comparison of the gamma nail and the proximal femoral nail. J Bone Joint Surg Br. 2004. 86(1):86–94.
23. Baumgaertner MR, Curtin SL, Lindskog DM, Keggi JM. The value of the tip-apex distance in predicting failure of fixation of peritrochanteric fractures of the hip. J Bone Joint Surg Am. 1995. 77(7):1058–1064.

24. Baumgaertner MR, Solberg BD. Awareness of tip-apex distance reduces failure of fixation of trochanteric fractures of the hip. J Bone Joint Surg Br. 1997. 79(6):969–971.





 PDF
PDF ePub
ePub Citation
Citation Print
Print






 XML Download
XML Download