Abstract
Background
Free fat graft has been used for the treatment of congenital hand differences. However, there have been a few reports about the outcome of that treatment. In this study, the outcome of free fat grafts for congenital hand and foot differences was investigated.
Methods
Fourteen bones with longitudinal epiphyseal bracket, 3 wrists with Madelung deformity, and 5 cases of osseous syndactyly were treated with free fat graft with osteotomy, physiolysis, or separation of osseous syndactyly. Of the fourteen bones with longitudinal epiphyseal bracket, 9 were treated with open wedge osteotomy with free fat graft and 5 with physiolysis and free fat graft. The Madelung deformity was treated with physiolysis with free fat graft. For osseous syndactyly, syndactyly release with free fat graft was performed five times on four hands.
Results
In the fourteen cases with longitudinal epiphyseal bracket, lateral deviation improved in all except two cases after surgery. The average lateral deviation angle changed from 32.5 degrees before surgery to 15.2 degrees after surgery. The average improvement of the lateral deviation angle was 12.2 degrees in the osteotomy group and 20.6 degrees in the physiolysis group. The mean ratio of improvement of the lateral deviation angle to the lateral deviation angle before surgery was 39.4% in the osteotomy group and 51.2% in the physiolysis group. The Madelung deformity improved after surgery in two cases but there was no improvement in one case. For these conditions, the results were not good enough when surgery was done after age 13 or at age four for severely hypoplastic brachymesophalangy. Of the 5 cases of osseous syndactyly, reunion of the separated bones occurred in one case. The grafted free fat should be deep enough to cover the osteotomy site of the bones to prevent reunion of the separated bones.
Conclusions
Physiolysis and free fat graft performed during the growth period can correct the deviation due to longitudinal epiphyseal bracket and Madelung deformity. Free fat graft is also useful to prevent reunion of the bones after separation of osseous syndcatyly, if the grafted fat is securely filled into the space between the separated bones.
Langenskiold1,2) reported a limited excision of the bone bridge of the epiphysis, which was caused by trauma, together with the physis and its replacement with free fat graft in order to improve longitudinal growth of the long bone. Light and Ogden3) reported that when the longitudinal epiphyseal bracket was osteotomized and followed with free fat graft, it could sometimes be supplemented with a bone graft on the opposite side of the osteotomized side of the affected bone. Vickers4) applied a limited excision at the midzone of the continuous epiphysis of the longitudinal epiphyseal bracket, also called the Delta phalanx, together with the physis and its replacement, with free fat graft in order to correct the deviation of the phalanx of the clinodactyly of the little finger. Then he showed that this procedure restored growth in the inherited disorder of the delta phalanx. Vickers and Nielsen5) also applied a similar procedure for Madelung deformity and have shown that the procedure restores growth and minimizes deformity. The authors utilized free fat graft for the above mentioned conditions and also for osseous syndactyly in order to prevent reunion of the bones. However, there have been few reports about the outcome of this kind treatment.6,7) In this paper, we report our experience of free fat graft for the treatment of congenital hand differences including longitudinal epiphyseal bracket, Madelung deformity and osseous syndactyly. The purpose of this study is to investigate outcome of free fat graft with or without osteotomy for the delta phalanx, Madelung deformity and osseous syndactyly.
The authors reviewed 14 bones of 10 patients with longitudinal epiphyseal bracket, and 3 wrists of 2 patients with Madelung deformity that were treated with physiolysis followed with free fat graft, and 5 cases of osseous syndactyly treated with syndactyly release followed with free fat graft. As for the underlying condition of the longitudinal epiphyseal bracket, there were 8 cases of clinodactyly, 2 cases of congenital hallux varus, 3 cases of abnormal induction of digital rays, including 2 cases of central synpolydactyly, and one case of cleft hand.
For the longitudinal epiphyseal bracket, 9 bones were subjected to open wedge osteotomy combined with physiolysis followed with free fat graft (osteotomy group); and 5 bones were subjected to resection of the midzone of the continuous epiphysis of the longitudinal epiphyseal bracket followed with free fat graft (physiolysis group) (Fig. 1). The ages of patients at the operation ranged from 2 to 13 years with an average of 4.7 years. For these cases, the lateral deviation angle was measured. Lateral deviation angle is defined as the angle between the longitudinal axis of the metacarpal bone and the distal and proximal phalanges of the affected digit or toe (Fig. 2).8) The percentage of improvement in the lateral deviation angle was calculated as the ration of improvement lateral deviation angle to the lateral deviation angle before surgery. The lateral deviation angle at the final follow-up was compared to the lateral deviation angle before surgery. The lateral deviation angle and the percentage of improvement of lateral deviation angle to lateral deviation angle before surgery in the physiolysis group and that in osteotomy group was investigated. The follow-up period after surgery ranged from 1 to 8 years with an average of 3.6 years.
For the Madelung deformity, 3 wrists were subjected to physiolysis followed with free fat graft (Fig. 3). The ages at the time of surgery were 11, 12, and 13 years, respectively. For these cases, the inclination of the distal radius and the palmar shift of the hand were measured. The inclination of the distal radius is defined as the angle between the perpendicular line of the longitudinal axis of the radius and the line of the distal articular surface of the radius by using an anteroposterior (AP) view of the roentgenogram (Fig. 2). Palmar shift of the hand is defined as the ratio of the shortest distance between the scaphoid tubercle and the extension line of the palmar cortex of the radial shaft to the width of the radial shaft by using a lateral view of the roentgenogram (Fig. 2).9) The inclination of the distal radius and palmar shift of the hand at the final follow-up were compared with those before surgery. The follow-up period after surgery was 2.5, 1.5, and 1 year, respectively.
For the 5 cases of osseous syndactyly, free fat graft was performed after removal of the bone bridge between the adjacent united phalanges (Fig. 4). The ages of the patients at the time of surgery ranged from 3 to 13 years, with an average of 7.2 years. For these cases, the reunion of the bones involving osseous syndactyly was evaluated. The follow-up period after surgery ranged from 1 to 7 years, with an average of 3.6 years.
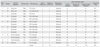
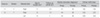
The lateral deviation angle before surgery ranged from 16 degrees to 75 degrees with an average of 32.5 degrees, and at follow-up ranged from 0 to 52 degrees with an average of 19.0 degrees (Table 1). The lateral deviation angle after surgery ranged from 0 to 31 degrees with an average of 15.2 degree. The mean ratio of improvement of the lateral deviation angle after surgery, which is the ratio of improvement angle to the lateral deviation angle before surgery, was 46.7. The deviation angle was significantly improved after surgery (p = 0.0015, Wilcoxon signed-ranks test).
Then, the authors investigated the lateral deviation angles in the osteotomy and physiolysis groups. The average improvement of the lateral deviation angle in the osteotomy group was 12.2 degrees and 20.6 degrees in the physiolysis group. The mean ratio of improvement of the lateral deviation angle to the lateral deviation angle before surgery in the osteotomy group was 39.4% and was 51.2% in the physiolysis group. Improvement and the percentage of improvement of the lateral deviation angle after surgery seemed better in the physiolysis group than in in the osteotomy group. The shape of the bone with the longitudinal epiphyseal bracket seemed to change from triangular to trapezoidal. That means the diaphysis of the affected bones became normal in appearance during the follow-up period.
There were 7 cases (Case #3, #5 [both hands], #6, #7, #9, #10), in which the percentage of the improved angle was less than 50%. Among them, cases #3 and #10 have been followed up for only one year. In cases #3 and #6 with brachymesophalangy, surgery had been done at the age of 4, and the hypoplastic middle phalanx with the longitudinal epiphyseal bracket was small. During surgery, it was difficult to put the fat graft deep enough in the space between the osteotomized bones in these cases. In case #7, surgery was done at the age of 13 and although it seemed to be too late, the patient was satisfied with the result.
The inclination of the distal radius before surgery was 41, 44, and 44 degrees in each case (Table 2). At follow-up it was 35, 36, and 48 degrees, respectively. The palmar shift of the hand before surgery in each case was 1.82, 2.50, and 3.00. At the final follow-up, it was 1.55, 2.25, and 3.43, respectively. For one case, in which the surgery was performed at the age of 13, the lateral deviation angle and the palmar shift of the hand worsened at the final follow-up.
No recurrence of bone union was observed in 4 out of 5 cases with osseous syndactyly (Table 3). In one case, in which bone union recurred after resection of the bone bridge and free fat graft, the same procedure was performed again 7 years after the first surgery, but the free fat was put in the separated space and fixed with a pull out nylon technique at the second surgery. No recurrence of bone union was observed 2 years after the second surgery.
In case #7, a 5.8-year-old girl was referred to us because of clinodactyly of the left little finger, demonstrating the longitudinal epiphyseal bracket of the middle phalanx (Fig. 5). The lateral deviation angles were 44 degrees. Epiphysiolysis followed by free fat graft was performed. The lateral deviation angle changed from 44 degrees to 27 degrees. At the age of 13, it was 13 degrees and the improvement was 31 degrees (Fig. 6). Satisfactory improvement has been achieved. The patient visited us because of the same problem of the right little finger at the age of 13. The patient seemed too old for physiolysis only (Fig. 7). The open wedge osteotomy of the middle phalanx was performed and the space was packed with free fat graft. The lateral deviation angle was 40 degrees before surgery and 30 degrees two years after surgery (Fig. 8). Only 10 degrees of improvement was achieved 2 years after surgery. Because of the soft tissue tension at the age of the surgery, complete correction could not be achieved. However, an improvement in the shape of the middle phalanx was noticed.
In case #8, a 2-year-old boy was referred to us because of right central synpolydactyly due to the abnormal induction of digital rays demonstrating the longitudinal epiphyseal bracket of the proximal phalanx of the ring finger associated with the cross bone between the middle and ring fingers (Fig. 9A and 9B). The lateral deviation angle was 25 degrees before surgery. Syndactyly release was performed, the cross bone was resected, and physiolysis followed with free fat graft at the age of 2 (Fig. 9C). The lateral deviation angle was changed from 44 degrees to 8 degrees 8 years after surgery. The shape of the proximal phalanx changed from a D shape before surgery to a trapezoidal shape at the final follow-up (Fig. 10).
In case #3, an 11-year-old girl was referred to us because of the Madelung wrist deformity (Fig. 11). During surgery, a bone bridge, formed prematurely across the physis of the ulnar side of the distal radius, was resected and the space, after removal of the bone bridge, was replaced with free fat graft (Fig. 12). The inclination of the distal radius before surgery and two and one-half years after surgery was 41 and 35 degrees, respectively. The palmar shift of the hand was 1.82 before surgery and 1.55 at follow-up. The prominence of the ulnar head was reduced and the palmar shift of the carpal bones was also reduced after surgery (Fig. 13). The appearance of the wrist deformity was improved and the patient was satisfied with the results.
In case #4, a 3-year-old boy was referred to us because of a left cleft hand and osseous syndactyly of the right hand and foot due to abnormal induction of digital rays.
For the left hand, the cleft was closed and the first web was widened with the Snow-Little procedure at the age of one year. Osseous syndactyly occurred between the distal phlanges and the proximal phalanges, but the middle phalanges were not united osseously in the right hand (Fig. 14). The width of the distal interphalangeal joints of the syndactylous fingers became wider because the direction of the growth of the distal phalanges had been changed due to the osseous union at the tip of the distal phalanges of the middle and ring fingers (Fig. 15). At the age of three, the united distal phalanges were exposed though a palmar longitudinal incision and the osseous union was separated; the space between these phalanges was filled with free fat graft. The direction of the growth of the distal phalanges was changed and no reunion was observed after surgery (Fig. 16A). Separation of the united proximal phalanges was not performed since it might worsen the hand function. At the age 6, the patient wanted to be treated with osseous syndactyly release of the middle and ring fingers. Syndactyly release was done then with a dorsal rectangular flap and a free skin graft; the united proximal phalanges were separated and the space between these phalanges was filed with free fat graft (Fig. 16B). Reunion of the separated proximal phalanges occurred two and a half years after the surgery. The patient sustained a distal phalangeal fracture at the age of 13 (Fig. 17A). The fracture was fixed with modified interosseous wiring and osseous union of the proximal phalanx of the middle and of the ring finger was performed; free fat was grafted into the separated phalanges (Fig. 17B). Reunion had not occurred 1 year after the last surgery (Fig. 17C). The patient got some arc of independent motion of the middle and ring fingers and was satisfied with the results.
The Delta phalanx is defined that the phalanx in which the epiphyseal growth plate runs longitunally, although normally, it runs perpendicular to the longitudinal axis of the phalanx.10) It was also defined as the longitudinal bracketed diaphysis or the longitudinal epiphyseal bracket.3,11) The terminology of delta phalanx is used in the International Federation of Societies for Surgery of the Hand (IFSSH) classification for congenital hand differences.12) Some investigators think that the Delta phalanx is not the appropriate terminology and recommend using the longitudinal bracketed diaphysis or the longitudinal epiphyseal bracket.3,11) The Delta phalanx often appears as a part of congenital hand differences, such as central polysyndactyly, cleft hand, thumb polydactyly, clinodactyly of the little finger, and others.8) The same kind of deformity appears in metacarpal or metatarsal bones. Therefore, the terminology of the Delta bone has been used in the Japanese modification of the IFSSH classification.13,14)
The longitudinal epiphyseal bracket causes deviation of the digits and toes. To correct the deviation caused by the Delta bone, the selection of surgical procedures, such as open wedge osteotomy, closed wedge osteotomy with or without bone graft, or fat graft with or without osteotomy is still controversial.11,15) The bone graft is often reported in the literature. But in cases for which bone graft was performed, some recurrence of deformity was reported. Kato and his colleague8) observed the early epiphyseal closure in recurrent cases. On the other hand, Light and Ogden3) reported that the longitudinal epiphyseal bracket was osteotomized and followed with free fat graft, sometimes supplemented with a bone graft on the opposite side of the affected bone. Vickers4) applied a limited excision of the midzone of the continuous epiphysis of the longitudinal epiphyseal bracket, together with the physis and its replacement with free fat graft, and showed that the procedure restored longitudinal growth of the affected bone and corrected the deviation of the phalanx of the clinodactyly of the little finger.
In this series, the authors got the same results as Vickers did, and there were no recurrence and no early epiphyseal closure after surgery. Therefore, free fat graft is useful to correct the deviation of the digits and toes due to the Delta bone.
Improvement and the percentage of improvement of the lateral deviation angle after surgery seemed better in the physiolysis group than in in the osteotomy group. The cases were too small and the statistically analysis should be done in the large groups. The ability to correct the deviation due to the Delta bone may be great after epiphyseolysis, when the deformity is severe. However, in the osteotomy group, the ability to correct the deviation might decrease, because the deviation was corrected by osteotomy during surgery.
The Madelung deformity is characterized by dorsoulnar prominence of the ulnar head, radiopalmar displacement of the hand and various degrees of shortening of the forearm bones. The deformity may appear as a part of dyschonroosteosis. The radius is bowed anteriorly and the distal radius has turned in an ulnar and palmar direction. Then the hand displaced palmarly, while the ulna proceeded straight to become prominent dorsoulnarly.
Previously, shortening osteotomy of the ulna, with or without corrective osteotomy of the radius, has been performed for wrist pain and or correction of the wrist deformity.16-18) In 1992, Vickers and Nielsen5) reported physiolysis, which includes excision of the bony bridge formed prematurely across the physis, and its replacement with fat graft. They also emphasized release of the tight ligamentous structure - the radiplunate ligament - that is attached to the proximal pole of the lunate and the radial groove and is called Vickers' ligament.
In this paper, the authors reported their experience of the same procedure reported by Vickers4) for the Madulung deformity. The improvement of the deformity was confirmed with evaluation of the roetgenogram in 2 out of 3 cases. In these two cases, the prominence of the ulnar head and palmar shift of the hand apparently improved.
One of the important factors, which influences the results of surgery for the longitudinal epiphyseal bracket and the Madelung deformity, is the age of the patient at surgery. In this series, not enough correction was achieved when the surgery was performed for girls with the Madelung deformity after the age of 12 and for girls with clinodactyly associated with the longitudinal epiphyseal bracket after the age of 13. In these cases, the growth period of the bone after surgery seemed too short. Vickers4) reported that, ideally, this procedure should be performed early before the deformity is unacceptable. He also stated that even in late presentations, with only a few years of growth remaining, physiolysis will produce a worthwhile benefit. The authors also think that the procedure might be useful for correction of the Madelung deformity, when the surgery is performed soon enough. From our results, one year of growth remaining might be too short a time. The authors think that surgery should be performed sooner than 12 years old for these conditions. However, in cases with hypoplastic brachymesophalangy with the longitudinal epiphyseal bracket, for which surgery was done at the age of 4, not enough correction of the deviation was achieved. Therefore, early surgery should also be avoided for the severely hypoplastic middle phalanx with the longitudinal epiphyseal bracket.
Free fat graft was used to prevent adhesion of the nerve to the surrounding tissue after spine surgery.19) On the other hand, vasucularized free or pedicle fat graft has been used for mobilization of congenital raioulnar synostosis.20) We used free fat graft to prevent reunion of the bone after release of the osseous syndactyly. After excision of the bone bridge in the proximal phalangeal type of the osseous syndactyly, the base of the proximal phalanx is too proximal to be separated by a skin flap. So, some kind of interposed materials, for example a silicone sheet or free fat graft, are helpful to prevent recurrence of bone union after separation.21) Free fat graft has better affinity with the body than silicone. There was no recurrence of the bone union except in one case after separation of the bone was followed with free fat graft. As for the tip of the surgical technique, the grafted free fat should be deep enough to cover the osteotomy site of the bones, or exposed raw surfaces of the bone, after physiolysis. In order to do so, a pull out nylon technique might be useful and surgery should not be performed too early.
In this study, the authors investigated the outcome of free fat grafts for congenital hand and foot differences. Free fat graft was performed after osteotomy or epiphyseolysis for the longitudinal epiphyseal bracket and the Madelung deformity, and also after separation of the osseous syndactyly. As for the longitudinal epiphyseal bracket and the Madelung deformity, spontaneous correction of the deviation after free fat graft with corrective ostronomy or physiolysis was achieved in most cases. However, the results were not good enough when surgery was done after the age of 13 or when it was done at the age of four for severely hypoplastic brachymesophalangy. As for osseous syndactyly, recurrence of bone union was not observed in any case except for one. Free fat graft seems useful to prevent reunion after removal of the bone bridge associated with congenital hand problems if it is performed before the age of 12 and the affected bone is large enough for osteotomy, physisolysis and secure free fat graft.
Figures and Tables
Fig. 1
Procedures for the longitudinal epiphyseal bracket. Two kind of procedures have been performed for the longitudinal epiphyseal bracket. (A, B) In the physiolysis group, the midzone of the longitudinal epiphyseal bracket was excised as shown with the small arrow and replaced with free fat graft as shown with the long arrow. (C, D) In the osteotomy group, an open wedge osteotomy was performed at the midzone of the phalanges as shown with the transverse line and the deviation was corrected as shown with the small arrow. Then the gap was filled with free fat graft as shown with the long arrow. Reprinted with permission from Japanese Society for Surgery of the Hand.9)

Fig. 2
Postoperative evaluation of the physiolysis for the longitudinal epiphyseal bracket and the Madelung deformity. (A) Lateral deviation angle (LDA): LDA is defined as the angle between the longitudinal axis of the metacarpal bone (a) and that of the distal and proximal phalanges (b) of the affected digit or toe. (B) Inclination of the distal radius: The inclination of the distal radius is defined as the angle between the perpendicular line (c) of the longitudinal axis of the radius and the line of the distal articular surface of the radius (d) by using an AP view of the roentgenogram. (C) Palmar shift of the hand: Palmar shift of the hand is defined as the ratio of the shortest distance (f) between the scaphoid tubercle and the extension line of the palmar cortex of the radial shaft to the width (e) of the radial shaft by using a lateral view of the roentgenogram. Reprinted with permission from Japanese Society for Surgery of the Hand.9)

Fig. 3
Physiolysis with free fat graft for the Madelung deformity according to Vickers procedure. (A) Through the palmar approach, the radiolunate ligament was removed and the bone block connecting the epiphsis across the physis to the metaphysis of the distal radius was removed an shown with the oblique long arrow. (B) A dotted area, where the bone block was removed, was packed with free fat graft and was fixed there by suturing the surrounding tissue such as periosteum or the holes of the cortex of the radius. Holes of the bone were made with a Kirshner wire. Reprinted with permission from Japanese Society for Surgery of the Hand.9)

Fig. 4
Free fat graft after separation of the osseous syndactyly. Excision of the bone bridge (A) and replacement with free fat graft (B) was performed.
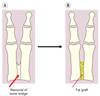
Fig. 5
Case #7, left hand: clinodactyly of the little finger due to the longitudinal epiphseal bracket of the middle phalanx. Excision of the midzone of the longitudinal epiphyseal bracket combined with free fat graft was performed on the middle phalanx at the age of 6. The lateral deviation angle was 44 degrees before surgery.

Fig. 6
Case #7, right hand at the age of 15. The lateral deviation angle was improved to 13 degrees 7 years after surgery. In this case, 31 degrees of spontaneous correction has been achieved.

Fig. 7
Case #7, right hand of a 13-year-old girl. Clinodactyly of the little finger due to the longitudinal epiphyseal bracket. The patient seemed too old to be treated with physiolysis only. The open wedge osteotomy of the middle phalanx was performed and the space was packed with free fat graft. The lateral deviation angle was 40 degrees before surgery.

Fig. 8
Case #7, left hand at the age of 13. The lateral deviation angle was corrected 10 degrees 2 years after surgery. Thirty degrees of deviation still remained, but the improvement of the shape of middle phalanx had been obtained.
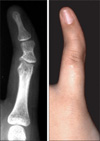
Fig. 9
Case #8, right hand of a 2-year-old boy. Synpolydactyly with a cross bone and the longitudinal epiphyseal bracket of the ring finger. (A) There was cutaneous syndactyly and overlapping of the middle and ring fingers due to deviation of the ring finger. (B) Roentgenogram revealed the longitudinal epiphyseal bracket of the proximal phalanx of the ring finger and a cross bone between the middle and ring fingers. (C) The roentgenogram after removal of the cross bone and physiolysis followed with free fat graft.

Fig. 10
Case #8, the appearance and roentgenogram 8 years after surgery. (A) The ring finger was short, but the deviation at follow-up was improved compared to before surgery. (B) The shape of proximal phalanx changed from a D shape before surgery to trapezoidal shape at follow-up.

Fig. 11
Case #11, the Madelung deformity treated with physiolysis and free fat graft. (A) The appearance of the wrist deformity was typical of the Madelung deformity. (B) AP view roentgenogram of the wrist revealed a bone bridge formed prematurely across the physis of the ulnar side of the distal radius. The ulnar head was overlapped with the lunate and triquetrum. (C) Lateral view roentgenogram of the wrist revealed dorsal subluxation of the ulnar head and a palmar shift of the carpal bones.

Fig. 12
Case #11, postoperative roentgenograms. (A) Two months after surgery. (B, C) Five months after surgery. No bony bride formation was observed across the physis of the distal radius.

Fig. 13
Case #11, the appearance and roentgenograms 12 months after surgery. (A) The appearance of the wrist deformity was improved. (B) The prominence of the ulnar head was reduced. (C) Ulnar inclination was reduced and the overlapping between the ulnar head and carpal bones disappeared. (D) Dorsal subluxation of the ulnar head seemed to be reduced. The palmar shift of the carpal bones was improved.

Fig. 14
Case #14, a one-year-old boy with osseous syndactyly of the right hand. (A) The appearance: there is a common nail of the middle and ring fingers. (B) Roentgenogram: the distal ends of the distal phalanges fused osseously. The proximal phalanges of these fingers fused completely.

Fig. 15
Case #14, the appearance and roentgenogram at the age of three. The width of the distal interphalangeal joints of the syndactylous fingers became wider, because the direction of the growth of the distal phalanges were changed due to the osseous union of the tip of the distal phalanges of the middle and ring fingers.

Fig. 16
Case #14, roentgenogram at the age of six. (A) The united distal phalanges were separated and the space between these phalanges was filled with free fat graft at the age of three, but there was no recurrence of the bone union. (B) This was a roentgenogram 7 weeks after the syndactyly release of the middle and ring fingers. The united proximal phalanges were separated and the space between these phalanges was filled with free fat graft. The distal interphalangeal joint of the middle finger was unstable and it was fixed with a Kirschner wire for 8 weeks.
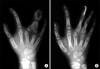
Fig. 17
Case #14, roentgenograms at the age of 13. (A) The reunion of the proximal part of the proximal phalanx occurred at the age of 8 (two and one-half years after the syndactyly release), but it was not treated surgically. The patient sustained a distal phalangeal fracture at the age of 13. (B) The fracture was fixed with modified interosseous wiring and the osseous union of the proximal phalanges of the middle and ring fingers was removed and free fat was grafted into the separated phalanges. (C) One year after the last surgery, there was no bony union of the phalanges.

References
1. Langenskiold A. The possibilities of eliminating premature partial closure of an epiphyseal plate caused by trauma or disease. Acta Orthop Scand. 1967. 38(1-4):267–279.

2. Langenskiold A. An operation for partial closure of an epiphysial plate in children, and its experimental basis. J Bone Joint Surg Br. 1975. 57(3):325–330.
3. Light TR, Ogden JA. The longitudinal epiphyseal bracket: implications for surgical correction. J Pediatr Orthop. 1981. 1(3):299–305.

4. Vickers D. Clinodactyly of the little finger: a simple operative technique for reversal of the growth abnormality. J Hand Surg Br. 1987. 12(3):335–342.

5. Vickers D, Nielsen G. Madelung deformity: surgical prophylaxis (physiolysis) during the late growth period by resection of the dyschondrosteosis lesion. J Hand Surg Br. 1992. 17(4):401–407.

6. Zhang G, Kato H, Yamazaki H. Physiolysis for correction of the delta phalanx in clinodactyly of the bilateral little fingers. Hand Surg. 2005. 10(2-3):297–302.

7. Bednar MS, Bindra RR, Light TR. Epiphyseal bar resection and fat interposition for clinodactyly. J Hand Surg Am. 2010. 35(5):834–837.

8. Kato H, Ogino T, Minami A, Sugimoto Y, Nakatsuchi Y. Delta pahalnax: roetntgenographic findings and surgical treatment. J Jpn Soc Surg Hand. 1990. 6(6):1031–1041.
9. Ishigaki D, Ogino T, Takahara M, Kikuchi N, Watanabe T. Pysiolysis and free fat graft for congenital growth plate disorders. J Jpn Soc Surg Hand. 2007. 24(3):306–311.
10. Jonew GB. Delta phalanx. J Bone Joint Surg Br. 1964. 46(2):226–228.
11. Carstam N, Theander G. Surgical treatment of clinodactyly caused by longitudinally bracketed diaphysis ("delta phalanx"). Scand J Plast Reconstr Surg. 1975. 9(3):199–202.

12. Swanson AB, Swanson GD, Tada K. A classification for congenital limb malformation. J Hand Surg Am. 1983. 8(5 Pt 2):693–702.

13. Jaeger M, Refior HJ. The congenital triangular deformity of the tubular bones of hand and foot. Clin Orthop Relat Res. 1971. 81:139–150.

14. Congenital Committee of the Japanese Society for Surgery of the Hand. A manual for classification of congenital hand deformities. J Jpn Soc Surg Hand. 2000. 17(3):353–365.
16. White GM, Weiland AJ. Madelung's deformity: treatment by osteotomy of the radius and Lauenstein procedure. J Hand Surg Am. 1987. 12(2):202–204.

17. Sakuma T, Ogino T, Minami A, Fukuda K, Muramatsu I. Clinical features of Madelung's deformity and functional results after surgery. J Jpn Soc Surg Hand. 1987. 4(2):586–592.
18. Watson HK, Pitts EC, Herber S. Madelung's deformity: a surgical technique. J Hand Surg Br. 1993. 18(5):601–605.
19. Langenskiold A, Kiviluoto O. Prevention of epidural scar formation after operations on the lumbar spine by means of free fat transplants: a preliminary report. Clin Orthop Relat Res. 1976. (115):92–95.
20. Kanaya F, Ibaraki K. Mobilization of a congenital proximal radioulnar synostosis with use of a free vascularized fascio-fat graft. J Bone Joint Surg Am. 1998. 80(8):1186–1192.

21. Ueba Y, Nishijima N, Takada H. Congenital synostosis of the fourth and fifth metacarpal. Seikei Geka. 1983. 34(12):1810–1812.




 PDF
PDF ePub
ePub Citation
Citation Print
Print



 XML Download
XML Download