Abstract
Background
Chronic lateral ankle instability often accompanies intra-articular lesions, and arthroscopy is often useful in diagnosis and treatment of intra-articular lesions.
Methods
Preoperative magnetic resonance imaging (MRI) examinations and arthroscopic findings were reviewed retrospectively and compared in 65 patients who underwent surgery for chronic lateral ankle instability from January 2006 to January 2010. MR images obtained were assessed by two radiologists, and the inter- and intra-observer reliability was calculated. American Orthopedic Foot and Ankle Society (AOFAS) and visual analogue scale (VAS) scores were evaluated.
Results
Abnormalities of the anterior talofibular ligament (ATFL) were found in all 65 (100%) cases. In arthroscopy examinations, 33 (51%) cases had talar cartilage lesions, and 3 (5%) cases had 'tram-track' cartilage lesion. Additionally, 39 (60%) cases of synovitis, 9 (14%) cases of anterior impingement syndrome caused by osteophyte, 14 (22%) cases of impingement syndrome caused by fibrotic band and tissue were found. Sensitivity of MRI examination for each abnormality was: ATFL, 60%; osteochondral lesion of talus (OLT), 46%; syndesmosis injury, 21%; synovitis, 21%; anterior impingement syndrome caused by osteophyte, 22%. Paired intra-observer reliability was measured by a kappa statistic of 0.787 (95% confidence interval [CI], 0.641 to 0.864) for ATFL injury, 0.818 (95% CI, 0.743 to 0.908) for OLT, 0.713 (95% CI, 0.605 to 0.821) for synovitis, and 0.739 (95% CI, 0.642 to 0.817) for impingement. Paired inter-observer reliability was measured by a kappa statistic of 0.381 (95% CI, 0.241 to 0.463) for ATFL injury, 0.613 (95% CI, 0.541 to 0.721) for OLT, 0.324 (95% CI, 0.217 to 0.441) for synovitis, and 0.394 (95% CI, 0.249 to 0.471) for impingement. Mean AOFAS score increased from 64.5 to 87.92 (p < 0.001) when there was no intra-articular lesion, from 61.07 to 89.04 (p < 0.001) in patients who had one intra-articular lesion, and from 61.12 to 87.6 (p < 0.001) in patients who had more than two intra-articular lesions.
Conclusions
Although intra-articular lesion in patients with chronic lateral ankle instability is usually diagnosed with MRI, its sensitivity and inter-observer reliability are low. Therefore, arthroscopic examination is strongly recommended because it improved patients' residual symptoms and significantly increased patient satisfaction.
Ligamentous injury of the lateral ankle is a common ligamentous injury occurring in sports activities. Most ankle ligament injuries show good results with conservative treatments, while patients with continuous pain and instability are treated surgically. Repair or reconstruction of the injured lateral ligament should be considered for these patients, and many surgical methods have been introduced.1,2)
In many cases, intra-articular lesions are concomitant with chronic lateral ankle instability. Therefore, arthroscopy has been recognized as having an important role as a direct approach to intra-articular lesions. In this study, we tried to assess the diagnostic capacity of preoperative magnetic resonance imaging (MRI) examination by comparing the MRI findings with those of arthroscopic examination observed during surgery. Thus we report the clinical results with a review of the literatures.
Sixty-five patients who received preoperative MRI and arthroscopic examination were selected retrospectively from 97 patients who were physically and radiologically examined and diagnosed with chronic lateral ankle instability, and finally underwent surgery by the modified Brostrom procedure from January 2006 to January 2010. There were 39 males and 26 females. Forty-one cases involved the right ankle and 24 involved the left. Every patient had experienced an ankle sprain more than twice and complained of discomfort and swelling at the lateral side of the ankle joint occurring on or after walking and sports activities. Diagnosis of chronic lateral instability was made by considering each patient's past history and results of physical examination, simple radiographs, and MRI findings. Patients who had not undergone MRI examination or who had been diagnosed with other ankle fractures and rheumatic diseases were excluded. This study protocol was reviewed and approved by the Institutional Review Board of Myongji Hospital of Kwandong University.
Patients were placed in the supine position under the spinal anesthesia. A 4.0 mm, 30 degree arthroscope was inserted into the anteromedial and anterolateral portals, and overall ankle examination was performed. During the procedure, the anterior space of the ankle joint and both gutters were examined, and then a 2.7 mm, 30 degree arthroscope was inserted for posterior of ankle joint. Status of ligaments was classified as elongation (if loosening or thinned), thickening, and rupture (if there was no continuity). In treatment of osteochondral lesion of talus (OLT), debridement was done in those who had rough surface or fibrillation of the articular cartilage overlying the lesion; multiple drilling or microfracture technique was used when flap or displaced fragments were present. Synovitis was diagnosed by the increase of synovial fold and hypertrophy by a reddish color change in arthroscopic findings. Bony impingement was determined by impingement of bony spur of talar neck area and distal tibia when the ankle joint was dorsiflexed. Soft tissue impingement was determined by impingement of tibiotalar joint by fibrous tissue or band during range of motion of ankle joint. Furthermore, debridement was performed for synovitis and anterior impingement syndrome (osteophyte, soft tissue impingement), and fibrous tissue and loose body were also removed. About a 4 cm sized anterior curved longitudinal skin incision was then made along the anterior border of lateral malleolar tip. A lateral ankle reconstruction using a modified Bröstrom technique was performed to treat the chronic lateral ankle instability.
T1 and T2 sagittal, axial, and coronal images were obtained using a MRI system (Philips Intera 1.5 Tesla; DA Best, Netherlands). The repetition time and echo time for the T1-weighted and T2-weighted images were 500 to 600 msec and 11 to 15 msec, and 2,000 msec and 11 to 15 msec, respectively. The repetition time and echo time for the T2-weighted fat suppression images were 3,400 to 3,600 msec and 11 to 15 msec. The other acquisition parameters were: field of view, 150 × 150 mm; matrix size, 224 × 224; and slice thickness, 4 mm.
MR images obtained were assessed by two radiologists using picture archiving and communication system (PACS; M-view ver. 5.0; Marotech, Seoul, Korea). The radiologists were unaware of the patients' clinical symptoms and other test results. They were asked to assess MRI data on two occasions in two separate places without consultation or discussion with each other. The assessments were performed with an interval of 2 weeks and the inter- and intra-observer reliability was calculated. The patients were identified only by randomly assigned numbers. Synovial hypertrophy and fibrotic scarring in the medial and lateral gutter were determined by a display of low signal on T1-weighted and low to intermediate signal on T2-weighted images.3) Anterior impingement syndrome was defined by the presence of a distal anterior tibial osteophyte. Impingement was defined as a condition where there is contact between the anterior surface of the tibia and the superior aspect of the talar neck. Typical MRI findings included osteophyte, subchondral sclerosis, tibiotalar effusion, talar and anterior distal tibial subchondral edema, and fibrous overgrowth. Joint cartilage lesions were classified as four grades.4)
American Orthopedic Foot and Ankle Society (AOFAS) and visual analogue scale (VAS) scores were used to compare the preoperative and the last follow-up status. Patient satisfaction was recorded at the last follow-up visit by classifying "poor, fair, good, and excellent" as a level of satisfaction.
SAS ver. 9.1 (SAS Institute, Cary, NC, USA) was used for every statistical analysis and weighted kappa values (κ) were calculated to determine intra- and inter-observer reliability. The agreement was rated as follows: poor, 0 to 0.2; fair, 0.21 to 0.4; moderate, 0.41 to 0.6; substantial, 0.61 to 0.8; and excellent, > 0.81.
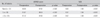
Sixty-five cases of intra-articular abnormality were observed by arthroscopic examination. Four cases of rupture of anterior talofibular ligament (ATFL), 50 cases of its elongation, and 11 cases of its thickening were observed. Thirty-three cases of cartilage lesion of talus and 13 cases of anterior inferior tibiofibular ligament injury-induced scar tissue were observed by arthroscopy (Table 1). Thirty-two cases were found at cartilage lesion of talus alone, two at cartilage lesion of tibia alone, and one at the kissing lesion. Cartilage lesions of talus were defined as grade 1 included 10 cases; grade 2, 12 cases; grade 3, eight cases (Fig. 1); and grade 4, three cases; where grade 2 was the biggest group with cartilage lesions of talus. Nineteen cases were observed from the medial side and 14 were from the lateral side. Moreover, 39 cases of synovitis, nine of anterior impingement syndrome by osteophytes (Fig. 2), 14 cases of impingement by fibrotic band (Fig. 3), and gutter syndrome by scar tissue at medial (five cases) and lateral (four cases) talus were observed.
In this study, sensitivities of preoperative diagnosis by MRI examination and postoperative diagnosis by arthroscopic examination were as follows: 39 (60%) cases of 65 showed ATFL injuries, 15 (46%) of 33 showed cartilage lesions of talus, one (10%) of 10 was included in grade 1, five (42%) of 12 were in grade 2, six (75%) of 8 were in grade 3, and three (100%) of 3 were included in grade 4. Three (21%) cases of scar tissue caused by distal tibiofibular ligament injuries, nine (21%) of synovitis, two (22%) of impingement syndrome caused by osteophyte, and none (0%) of impingement syndrome by fibrotic band, medial and lateral gutter syndrome, tram-track lesion, and loose body were found (Table 2). Paired intra-observer reliability was measured by a kappa statistic of 0.787 (95% confidence interval [CI], 0.641 to 0.864) for ATFL injury, 0.818 (95% CI, 0.743 to 0.908) for OLT, 0.713 (95% CI, 0.605 to 0.821) for synovitis, and 0.739 (95% CI, 0.642 to 0.817) for impingement. Paired inter-observer reliability was measured by a kappa statistic of 0.381 (95% CI, 0.241 to 0.463) for ATFL injury, 0.613 (95% CI, 0.541 to 0.721) for OLT, 0.324 (95% CI, 0.217 to 0.441) for synovitis, and 0.394 (95% CI, 0.249 to 0.471) for impingement.
In the arthroscopic findings, 12 showed no intra-articular lesion other than the ATFL injury, 28 showed one intra-articular lesion, and 25 showed more than two intra-articular lesions. Mean AOFAS score increased from 64.5 to 87.92 (p < 0.001) when there were no intra-articular lesion, and there was also an increase in the mean AOFAS score from 61.07 to 89.04 (p < 0.001) in those who had one intra-articular lesion. Patients who had more than two intra-articular lesions showed an increase from 61.12 to 87.6 (p < 0.001). VAS score decreased from 6.0 to 2.0 (p < 0.001) in those with no intra-articular lesion, from 6.32 to 2.0 (p < 0.001) in patients who had one intra-articular lesion, and from 6.52 to 2.08 (p < 0.001) in the patients who were diagnosed with more than two intra-articular lesions (Table 3).
Depending on the number of intra-articular lesions, patients showed an increase in the AOFAS score of 23.4, 28.0, and 26.5 when there were zero, one, and more two intra-articular lesions, respectively, and there were no statistically significant differences between the three groups. There was a decrease of VAS score of 4.0, 4.3, and 4.4 when there were zero, one, and more than two intra-articular lesions respectively, and the differences were also not statistically significant.
Depending on the grade of OLT, AOFAS scores increased from 61.1 to 89.7 (p = 0.007) when there were grade 1, from 60.83 to 85.25 (p = 0.002) in those who had grade 2, from 60.63 to 87.75 (p = 0.012) in the patients who were diagnosed with grade 3, and from 61.33 to 86.67 (p = 0.109) in the patients who were diagnosed with grade 4. VAS score decreased from 6.5 to 1.7 (p = 0.007) in those with grade 1, from 6.33 to 2.5 in patients who had grade 2, from 6.75 to 2.13 (p = 0.001) in the patients who were diagnosed with grade 3, and from 7.0 to 2.33 (p = 0.109) in the patients who were diagnosed with grade 4.
Ten (83.34%) of 12 patients with no intra-articular lesions, 26 (92.86%) of 28 patients with one intra-articular lesion, and 21 (84%) of 25 patients with two or more intra-articular lesions rated their satisfaction as grade "good" or "excellent". Three patients graded their satisfaction score as "poor"; one of them underwent total ankle arthroplasty due to severe osteoarthritis, one had osteochondral autograft transplantation because large OLT was observed, and the other showed extensively cartilage denuded of medial malleolar. Five patients graded as "fair", and these patients had either goutic arthritis, large OLT, mild osteoarthritis, re-injury, or superficial peroneal nerve injury. Especially, 3 patients had symptoms of superficial peroneal nerve injury which subsided naturally.
Injury of the lateral ankle ligament is the most common type caused by sports activities, with an incidence of 45% among baseball players and 17% to 31% among soccer players.5) Sprains account for 75% of ankle injuries, and 85% of these are caused by inversion.6) Gerber et al.7) have reported that 23% of total sports injuries affect the ankle, and 85% of them seem to be lateral sprain, 10% are sprain of syndesmosis, and only 5% are medial sprain. Most ankle ligamentous injuries are treated by conservative methods, however, 20% to 40% of patients complain of chronic instability and persistent discomfort.8) Structured instability, loss of proprioceptive capabilities, and the weakness of peroneal muscles seem to induce chronic instability, however, its specific mechanism is unclear yet.9) Many surgical techniques for the reconstruction of ATFL and calcaneofibular ligament have been introduced. Anatomically direct suture techniques for ruptured lateral ankle ligament have been reported by Brostrom,1) and Gould et al.2) also have reported outstanding results using methods to suture the stretched proximal area additionally to fibula, to prevent the ankle inversion. However, these conservative or surgical treatments only consider the ligamentous structures, without the aspects of intra-articular lesions.
In 1955, Bosien et al.10) reported that 33% of patients still have continued disability after the onset of acute ankle sprain, and 60% of them have ankle abnormalities. This continued disability also has been reported in many other reports ranging from 32% to 76%.10-14) Several authors have pointed the reason for this continuous pain is related with intra-articular problems of the ankle joint, while Liu and Jason15) reported that 6.8% of patients with ankle sprains seem to accompany osteochondral lesion, and they also said that this, with or without chronic ankle instability, seems to become a common cause of ankle pain. Recently, the importance of intra-articular lesions in patients with chronic lateral ankle instability has been recognized, and cases using arthroscopy together with ligamentous repair and reconstruction are increasing. In 31 patients with acute or chronic ankle instability, Taga et al.16) performed arthroscopic examination before ligament reconstruction, and 95% of chronic injury group and 89% of acute injury group were found to have cartilage lesions. Lesions mainly happened on the lateral side of ankle, with increasing severity if the injury was chronic. The authors found no relation between the instability and the grade of cartilage lesion, and reported that the grade of cartilage lesion increases with time. Other studies of OLT also have reported that its risk seems to increase with acute injuries, and the grade of lesion increases as time passes.16,17) These superficial cartilage lesions seem to be healed time after time, resulting with the higher incidence of acute ones, while cartilage lesions of high grade are not easily treated, lesions get worse as time passes. In our study, risk of OLT was higher in grade 1 and 2, which is contrary to the previous reports. Further studies may be needed to understand the cause of this result.
For 30 patients with acute ligamentous injury on lateral side, van Dijk et al.17) performed primary repair of the injured ligament and also the arthroscopic examination. Twenty (67%) cases of cartilage lesion were found, and 19 of these were medial lesions. Also, six (20%) cases of loose body and 19 (63%) cases of traumatic synovitis were found. Seven (37%) of 19 patients who previously had cartilage lesions at the time of injury complained of medial pain caused by medial cartilage lesion, and five (26%) of these patients said that they have difficulties during daily life. They said that intra-articular damages happened at the time of injury. Kibler18) had also performed arthroscopic examination before reconstructing ligamentous injuries in 46 patients; 38 (83%) had intra-articular lesions. The authors reported that these intra-articular lesions included 12 (26%) impingement lesions, 12 (26%) osteophytes, 6 (13%) cartilage lesions, 7 (15%) fibrotic bands, and 6 (13%) cases of loose body, and argued that arthroscopic examination before ligament repair is important, because other preoperative tests are insufficient. In addition, many associated lesions have been demonstrated by arthroscopic examination (Table 4).18-20)
From 68 cases of anterior ankle impingement syndrome induced by osteophytes, Kim et al.21) performed arthroscopic examinations and found six cases of tram-track lesion on talus. All six patients were soccer players, who had osteophytes at anteromedial area of distal tibia. Reporting that all tram-track cartilage lesions were located on the anteromedial side of the talus, the authors pointed out that a tram-track cartilage lesion might result from osteophytes of the tibia. However, in the present three cases, we did not find any anterior impingement syndrome caused by osteophytes and, from one case, we found two at the medial and lateral cartilage lesions of talus. One presented tram-track cartilage lesion at the anterolateral side, while the other showed loose body at the intra-articular area. These observations support the view that tram-track cartilage lesion might occurred by osteophytes; the cartilage is injured by joint motions if the loose body remains inside the ankle and finally cartilage lesions are induced.
Preoperative MRI examination has been performed frequently in recent years, and it is helpful for diagnosis of intra or extra-articular lesion, which is the reason for ankle pain after a sprain and which is difficult to diagnose clinically. MRI examination is useful for diagnosing injuries of lateral ankle ligaments and peroneal tendon, among others.22,23) However, even if cartilage lesions of grade 3 or 4 are detectable by preoperative MRI examination, its 4-mm thickness of sample vision actually makes it hard to identify superficial or smaller lesions than the interval. Moreover, it is hard to diagnose abnormalities of articular capsules or thickening of ligament, to perform dynamic tests of ligamentous stability, and can readily led to misdiagnoses. As found presently and previously, MRI sensitivity seems to be relatively low for the diagnosis of synovitis, impingement syndrome by fibrotic band and osteophyte, and loose body, while it is useful for diagnosis of ligamentous instability and cartilage lesion. To our knowledge, there are no previous reports about intra or inter-observer reliability of MRI findings of intra-articular in ankle joint. Because a low inter-observer reliability was observed, clinical findings should be incorporated with the MRI findings to diagnose intra-articular lesion in ankle joint. After the arthroscopic operation, clinical result and patient satisfaction showed a significant increase in all the cases regardless of the number of intra-articular lesions. However, our study had no control group, and further studies may be indicated as the sample size was not sufficiently large to understand how each form of the intra-articular lesion affected the clinical results.
In conclusion, MRI examination is a commonly used diagnostic modality for detecting intra-articular abnormalities in patients with chronic lateral ankle instability. However, inter-observer reliability and sensitivity of MRI findings were found to be relatively low in this study. Therefore, arthroscopic examination before ligament repair is a useful and recommended method for diagnosis and treatment of intra-articular lesions.19,20) In addition, it can improve patients' residual symptoms and significantly increase the patient satisfaction.
Figures and Tables
Fig. 2
Exostosis of anterior side of distal tibia and talar neck causes an anterior bony impingement.

Fig. 3
This arthroscopic view shows an anterior soft tissue impingement by fibrotic tissue in tibiotalar joint.

Table 2
MRI and Operative Finding Sensitivity and Specificity Concerning Chronic Lateral Ankle Instability (n = 65)

References
1. Brostrom L. Sprained ankles. VI. Surgical treatment of "chronic" ligament ruptures. Acta Chir Scand. 1966. 132(5):551–565.
2. Gould N, Seligson D, Gassman J. Early and late repair of lateral ligament of the ankle. Foot Ankle. 1980. 1(2):84–89.

3. Rubin DA, Tishkoff NW, Britton CA, Conti SF, Towers JD. Anterolateral soft-tissue impingement in the ankle: diagnosis using MR imaging. AJR Am J Roentgenol. 1997. 169(3):829–835.

4. Berndt AL, Harty M. Transchondral fractures (osteochondritis dissecans) of the talus. J Bone Joint Surg Am. 1959. 41-A:988–1020.

6. Baumhauer JF, Alosa DM, Renstrom AF, Trevino S, Beynnon B. A prospective study of ankle injury risk factors. Am J Sports Med. 1995. 23(5):564–570.

7. Gerber JP, Williams GN, Scoville CR, Arciero RA, Taylor DC. Persistent disability associated with ankle sprains: a prospective examination of an athletic population. Foot Ankle Int. 1998. 19(10):653–660.

8. Cass JR, Morrey BF. Ankle instability: current concepts, diagnosis, and treatment. Mayo Clin Proc. 1984. 59(3):165–170.

9. Freeman MA, Dean MR, Hanham IW. The etiology and prevention of functional instability of the foot. J Bone Joint Surg Br. 1965. 47(4):678–685.

10. Bosien WR, Staples OS, Russell SW. Residual disability following acute ankle sprains. J Bone Joint Surg Am. 1955. 37(6):1237–1243.

11. Jackson DW, Ashley RL, Powell JW. Ankle sprains in young athletes: relation of severity and disability. Clin Orthop Relat Res. 1974. (101):201–215.
12. MacCartee CC Jr. Taping treatment of severe inversion sprains of the ankle: early return to functional activities. Am J Sports Med. 1977. 5(6):246–247.
13. Lentell G, Baas B, Lopez D, McGuire L, Sarrels M, Snyder P. The contributions of proprioceptive deficits, muscle function, and anatomic laxity to functional instability of the ankle. J Orthop Sports Phys Ther. 1995. 21(4):206–215.

14. Staples OS. Result study of ruptures of lateral ligaments of the ankle. Clin Orthop Relat Res. 1972. 85:50–58.

15. Liu SH, Jason WJ. Lateral ankle sprains and instability problems. Clin Sports Med. 1994. 13(4):793–809.

16. Taga I, Shino K, Inoue M, Nakata K, Maeda A. Articular cartilage lesions in ankles with lateral ligament injury. An arthroscopic study. Am J Sports Med. 1993. 21(1):120–126.

17. van Dijk CN, Bossuyt PM, Marti RK. Medial ankle pain after lateral ligament rupture. J Bone Joint Surg Br. 1996. 78(4):562–567.

18. Kibler WB. Arthroscopic findings in ankle ligament reconstruction. Clin Sports Med. 1996. 15(4):799–804.

19. Hintermann B, Boss A, Schafer D. Arthroscopic findings in patients with chronic ankle instability. Am J Sports Med. 2002. 30(3):402–409.

20. Takao M, Uchio Y, Naito K, Fukazawa I, Ochi M. Arthroscopic assessment for intra-articular disorders in residual ankle disability after sprain. Am J Sports Med. 2005. 33(5):686–692.

22. Oae K, Takao M, Naito K, et al. Injury of the tibiofibular syndesmosis: value of MR imaging for diagnosis. Radiology. 2003. 227(1):155–161.

23. O'Neill PJ, Van Aman SE, Guyton GP. Is MRI adequate to detect lesions in patients with ankle instability? Clin Orthop Relat Res. 2010. 468(4):1115–1119.




 PDF
PDF ePub
ePub Citation
Citation Print
Print





 XML Download
XML Download