This article has been
cited by other articles in ScienceCentral.
Abstract
Background
Inflammation related hematological parameters vary greatly depending on patients. It is not well known how much increase of which parameter warrants suspicion of postoperative infection. This study proposes to identify the normal range and the predictive factors for postoperative infection by conducting a time series analysis of the hematological parameters of patients after the spinal posterior fusion.
Methods
A retrospective study was done with 608 patients who underwent spinal posterior fusion with pedicle screw fixation. Laboratory assessment including the leucocyte, neutrophil, C-reactive protein (CRP), and erythrocyte sedimentation rate (ESR) of patients for 2 weeks after operation. The patients were divided into the one-level fusion group (group I), the two-level fusion group (group II), the three or multi-level fusion or reoperation group (group III), and the postoperative infection group (group IV). Blood was drawn before breakfast prior to the operation, and then 2-3 days, 4-7 days, 8-11 days, and 12-14 days after the operation. The leucocyte count, neutrophil count, CRP, and ESR were measured.
Results
From 4-7 days after the operation, the CRP and neutrophil count of group IV were significantly higher than those of group I and II, and from 8-11 days after operation, the CRP and neutrophil counts were significantly higher than those of all groups. Twelve to fourteen days after the operation, the neutrophil count of group IV was significantly higher than that of group I and II, while the neutrophil count of group III was also higher than that of group I. The lower limit of the 95% confidence interval (CI) of the CRP and neutrophil count group IV was greater than the upper limit of the 95% CI of group I and II. The ESR of group IV was significantly higher than that of group I and III.
Conclusions
If the postoperative CRP and neutrophil counts are high, or if the CRP begins to rise again 8 days after the operation, the likelihood of infection increases, but caution must be exercised in interpreting the results. If the hematological parameters are higher than the lower limit of the 95% CI of the postoperative infection group, infection must be strongly suspected.
Keywords: Postoperative infection, Spinal posterior fusion, C-reactive protein, Neutrophil count, Erythrocyte sedimentation rate
The broad use of antibiotics and improvements in surgical and aseptic techniques in recent years has led to a lower incidence of infection after surgical procedures, but infections still remain a problem. In particular, the increased use of metal instruments in surgery has added to the risk of infection. Due to anatomical characteristics of the spine, serious complications may rise by spread of infections to the dura mater. Therefore, it is essential to prevent deep infection by detecting and treating it early. Postoperative infections took place in 1%, 2%, and 6% of cases following standard discectomy, posterolateral fusion, or by the insertion of additional instruments.
1-
4) To detect and treat postoperative infection early, a time series study of pyrexia, pain, delirium, inflammation-related hematological parameters, and drainage of the wound was conducted. To use hematological parameters to verify infection, a time series evaluation of those patients who underwent surgery in the lumbar region was conducted through blood tests during their hospitalization and a certain period of outpatient service. However, it was difficult to determine the normal range, and to identify which parameters warrant investigation of postoperative infection is not well known. There are many reports on time series analysis of these indicators, but only a few studies have conducted quantitative analysis.
5)
The objectives of this study are to describe the normal postoperative kinetics of hematological parameters after instrumented spinal surgery, to compare their usefulness as predictive factors for postoperative infection in the early postoperative period and to conduct a quantitative analysis of the hematological parameters of each group. The hematological parameters in patients who developed a postoperative infection versus those who did not were also compared. Finally, we attempted to discover indicators and their ranges for early detection or prediction of infection for different postoperational periods.
METHODS
From November 1999 to February 2008, out of a total of 787 patients of the Seoul Metropolitan Government Seoul National University (SMG-SNU) Boramae Medical Center who underwent fusion using pedicle screw insertion in the thoracic and the lumbar spine, 608 patients who underwent blood tests for two weeks were included in this study and reviewed retrospectively. Institutional Review Board approval was obtained for this study and informed consent was waived.
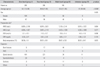
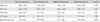
The patients were divided into the one-level fusion group (group I), the two-level fusion group (group II), the three or multi-level fusion or reoperation group (group III) and the postoperative infection group (group IV). The patient characteristics and underlying diseases are shown in
Table 1. The preoperative inflammation related hematological parameters such as white blood cell (WBC), absolute neutrophil count (ANC), C-reactive protein (CRP), and erythrocyte sedimentation rate (ESR) were not different between four groups.
The group IV patients were those who had drainage from the wound during hospitalization, hyperthermia and redness around the wound, constant pain in the wound, and whose temperature rose above 37.5℃. They were diagnosed as infected when microbes were identified and infected tissue was observed in the operating room, and consequently included in the postoperative infection group. Pathogens were identified in 12 patients. For 4 patients it was methicillin-resistant Staphylococcus aureus. For 4 other patients it was methicillin-resistant coagulase-negative Staphylococcus (MRCNS) and for 2 patients it was Enterococcus faecalis. Both E. faecalis and MRCNS were identified in one patient, and both methicillin-sensitive S. aureus and MRCNS were identified in one patient. The pathogen was not identified in 2 patients who were included in the postoperative infection group because they had clearly identifiable pus drainage from the wound. The number of fusion levels in group IV was 1 for 3 patients, 2 for 8 patients, 2 with revision surgery for 2 patients, and 4 for 1 patient. Blood was drawn before breakfast prior to the operation, and then 2-3 days, 4-7 days, 8-11 days, and 12-14 days after the operation. The leucocyte count, neutrophil count, CRP, and ESR were measured.
Analysis of variance (ANOVA) tested differences among the groups using SPSS ver. 11 (SPSS Inc., Chicago, IL, USA), and the Bonferroni correction was used to correct for multiple comparisons. Also, changes in hematological parameters of each group by period were examined by repeated measures ANOVA. Null hypotheses of no difference were rejected if p-values were less than 0.05.
RESULTS
Hematological Comparison of the Infection and the Normal Group
Two to three days after the operation, there was no significant difference between the infection group and the normal group (
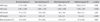
Table 2). Four to seven days after the operation, the leucocyte and neutrophil count of group IV (8,144 and 5,680 n/µL, respectively) was highest among the groups but there was no significant difference between groups. The CRP of group IV (7.47 mg/dL) was significantly higher than those of group I and II (3.62 mg/dL,
p = 0.005 and 3.61 mg/dL,
p = 0.004, respectively) (
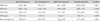
Table 3). Eight to eleven days after the operation, the neutrophil count of group IV (7,076 n/µL) was significantly higher than that of group I and II (4,597 n/µL,
p < 0.0001 and 4,984 n/µL,
p = 0.00019, respectively). The neutrophil count of group II and III (4,984 and 5,458 n/µL, respectively) was also significantly higher than that of group I (
p = 0.012 and
p = 0.003, respectively). Also, the CRP of group IV (7.8 mg/dL) was significantly higher than that of group I and II (1.63 mg/dL,
p < 0.0001 and 2.04 mg/dL,
p < 0.0001, respectively) (
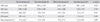
Table 4). Twelve to fourteen days after the operation, the leucocyte count of group III (8,011 n/µL) was significantly higher than that of group I (7,078 n/µL,
p = 0.006). The neutrophil count of group IV (5,994 n/µL) was significantly higher than that of group I (4,489 n/µL,
p = 0.012) and the neutrophil count of group III (5,449 n/µL) was also significantly higher than those of group I and II (4,769 n/µL and
p = 0.00022,
p = 0.011, respectively). In addition, the CRP of group IV (7.95 mg/dL) was significantly higher than that of group I, II, and III (1.03 mg/dL,
p < 0.0001; 1.68 mg/dL,
p < 0.0001; and 1.68 mg/dL,
p < 0.0001, respectively) (
Table 5).
Quantitative Comparison of the Infection Group and the Normal Group
Results obtained 8-11 days after the operation were quantitatively compared. For the neutrophil count, the lower limit of the 95% confidence interval (CI) of group IV (5,899 n/µL) was greater than the upper limit of the 95% CI of group I and II (
Fig. 1). For the CRP, the lower limit of the 95% CI of group IV (4.27 mg/dL) was higher that the upper limit of the 95% CI of group I, II, and III (
Fig. 2).
For the neutrophil count 12-14 days after the operation, the lower limit of the 95% CI of group IV (4,946 n/µL) was higher than the upper limit of the 95% CI of group I (
Fig. 1). Also, for the CRP, the 95% CI of group IV (4.71 mg/dL) did not overlap the 95% CI of group I, II, and III (
Fig. 2). With respect to the ESR, the 95% CI of group IV (37.83 mm/hr) did not overlap with the 95% CI of group I and III (
Fig. 3).
Comparison between Normal Groups by Period
Two to three days after the operation, the leucocyte count and neutrophil counts of group II were lower than those of group III. The CRP of group II was higher than that of group I and the CRP of group IV was also significantly higher than that of group III (
p = 0.016) (
Table 2). Four to seven days after the operation, the CRP of group IV was significantly higher than those of group I and II (
p = 0.005 and
p = 0.004, respectively) (
Table 3). Eight to eleven days after the operation, the neutrophil count of group IV were significantly higher than those of group I and II (
p < 0.0001 and
p = 0.00019, respectively) and the CRP of group IV were significantly higher than those of group I and II (
p < 0.0001, both). Also, the neutrophil count of group I was significantly lower than those of group II and III (
p = 0.012 and
p = 0.003, respectively) and the CRP of group I was significantly lower than that of group II (
p < 0.0001) (
Table 4). Twelve to fourteen days after the operation, the leucocyte count of group I was significantly lower than that of group III (
p = 0.006). The neutrophil count of group IV was significantly higher than that of group I (
p = 0.0012). The neutrophil count of group III was also significantly higher than those of group I and II (
p = 0.00022 and
p = 0.011, respectively). Finally, the CRP of group IV was significantly higher than those of group I, II, and III (
p < 0.0001, all) (
Table 5).
Comparison of Hematological Parameters of Different Groups by Period
The leucocyte and neutrophil count of group IV significantly increased from before the operation to 2-3 days after the operation (
p = 0.011 and
p = 0.0034, respectively), whereas 4-14 days after the operation, there was no significant decrease. The CRP was significantly higher than prior to the operation compared to 2-3 days after the operation (
p < 0.0001) and significantly lower 4-7 days after the operation (
p = 0.036) (
Fig. 4A). The ESR rose significantly both 2-3 days after the operation (
p = 0.0005) and 4-7 days after the operation (
p = 0.0057), and continued to rise 8-11 days after the operation as well.
In the normal groups (group I, II, and III), the leucocyte and neutrophil count 2-3 days after the operation were significantly higher than prior to the operation (p < 0.0001, all), and the leucocyte count 4-7 days after the operation was significantly lower than 2-3 days after the operation in all groups (p < 0.0001, all). Twelve to fourteen days after the operation, the leucocyte and neutrophil count significantly declined only in group II (p = 0.0047 and p = 0.0291, respectively).
The CRP of all normal groups rose significantly 2-3 days after the operation as compared to before the operation (
p < 0.0001, all), and 4-7 days after the operation there was a significant change (
p < 0.0001, all). There was a significant decrease in all normal groups 8-11 days after the operation (
p < 0.0001, all), as well as 12-14 days after the operation (group I and II,
p < 0.0001; group III,
p = 0.0035) (
Fig. 4B-D). The ESR of all normal groups increased significantly 2-3 days after the operation (
p < 0.0001, all) as compared to before the operation, and 4-7 after the operation as well (
p < 0.0001, all). Eight to eleven days after the operation, there was a significant decline in all normal groups (group I and II,
p < 0.0001; group III,
p = 0.019), and 12-14 days after the operation there was a significant decline from 8-11 days after the operation in all normal groups (group I and II,
p < 0.0001; group III,
p = 0.016).
DISCUSSION
The neutrophil count is an important indicator in checking the postoperational leucocyte count. Takahashi et al.
2) argued that a re-increase of the postoperation neutrophil count is an important hematological parameter indicative of postoperative infection, and that, if the CRP increases again 7 days after the operation, postoperative infection must be suspected. CRP is made in the liver in response to inflammation, infection, malignancy and tissue damage, and is characterized by a relatively high sensitivity and quick response.
6,
7) Several studies on postoperative changes in the CRP have reported that the CRP reaches its peak 2 or 3 days after the operation and declines, slowly returning to normal, eventually reaching the normal level between 14 and 21 days after the operation.
2,
8-
13) In contrast, the ESR is indirectly measured in proportion to the quantity of blood albumin and globulin, and remains increased until one year after the operation.
14) Unlike the ESR, CRP quantity is directly measured, and as the normal range is narrow and the postoperative count returns to normal quickly, CRP is believed to be a better indicator of postoperative infection.
15)
Since we quantitatively compared the changes in hematological parameters between the infection group and the normal groups while describing these changes at the same time, and tried to discover hematological parameters that are statistically different, this study is significantly different from others. One of the strengths of this study is that it divided the normal group according to the scope of the operation, and compared each normal group with the infection group. This study is also differentiated from others by the fact that it included more groups in the study than any other previous report. In this study, 2-3 days after the operation, the hematological parameters of the normal group and the infection group did not show any difference. This shows that, 2-3 days after the operation, the hematological parameters increased due to the effect of tissue damage from the surgery rather than infection in the postoperative infection group.
In particular, Thelander and Larsson
8) reported that the CRP reached its peak in the posterior lumbar fusion 3 days after the operation, and the creation of the liver cell CRP due to bacterial infection is known to start 6 hours after infection.
9) In this study the CRP of the postoperative infection group decreased significantly 4-7 days after the operation, and began to increase significantly 8-11 after the operation. The CRP of the infection group began to rise again 8-11 days after the operation, which was the same as reported by Aono et al.,
5) showing that the re-increase of the CRP 7 days after the operation warrants suspicion of infection.
15) Piper et al.
16) reported that a CRP of 4.6 mg/L had a sensitivity of 79 and a specificity of 68% to detect infection of spine implant. Although there was no difference between the normal groups 2-3 days after the operation despite postoperative infection, there was a significant increase 8-11 days after the operation compared to 4-7 days after the operation in the infection group. In addition, the CRP was significantly higher in the infection group than in the one-level fusion group and the two-level fusion group 4-7 days after the operation. Therefore, 2-3 days after the operation, the rise in CRP due to tissue damage was high in the infection group as well, and there was a small increase of CRP due to infection. Accordingly, no difference was observed in the normal group. A second interpretation is that, from 4-7 days after the operation, the increase of CRP due to tissue damage is normalized, and the rise in CRP due to the progress of infection continues. Consequently, the absolute value is different from that of the normal groups (one-level and two-level fusion groups) in the same period. Therefore, 8-11 days after the operation, the CRP increases again in the infection group compared to 4-7 days after the operation. In summary, the increase of the CRP due to infection can be reflected in the clinical hematological test only when infection progresses.
Four to seven days after the operation, when the one-level fusion group was compared to the infection group, there was a significant difference in the leucocyte count, neutrophil count and CRP, and only the CRP of the two-level fusion group was different. The CRP of the multi-level fusion group was not significantly different from that of the infection group. This shows that as the one-level fusion group has less tissue damage than the multi-level fusion group, the hematological parameters are normalized faster, and many indicators show there is a significant difference from the infected group. The CRP of the two-level fusion group is significantly different from that of the infected group, but the CRP of the multi-level fusion group is not significantly different from that of the infected group because multi-level fusion involves greater tissue damage. As for the multi-level fusion group, it is difficult to use the hematological parameters such as the CRP to predict the occurrence of infection.
Eight to eleven days after an operation, there was a significant difference between the neutrophil count and the CRP of all normal groups and those of the postoperative infection group. The neutrophil count and the CRP rapidly declined in the normal groups after the operation for 7 days, while at the same time the parameters increased in the postoperative infection group due to inflammation. Moreover, the CRP of this period can be regarded as an important indicator of early diagnosis of infection because the CRP increases again in the postoperative infection group. Therefore, the neutrophil as well as the CRP are useful indicators.
Twelve to fourteen days after the operation, there were differences between the multi-level fusion group and the postoperative infection group in terms of the neutrophil count, ESR, and CRP. In this period the hematological parameters are also normalized in the multi-level fusion group, and this leads to a significant difference from the infection group. Eight to eleven days after the operation, hematological parameters begin to normalize in the normal group, and in the infected group the indicators increased due to infection.
The ESR did not show any significant difference depending on the size of surgery in the normal group, and the difference between the postoperative infection group and the normal groups was observed only 12-14 days after the operation. This indicates that normalization is slow here, and the number itself does not directly reflect the extent and size of inflammation. While the quantity is directly measured for the CRP, the ratio of albumin to globulin in the serum is indirectly measured for the ESR.
Hematological parameters exhibiting a significant difference from the postoperative infection group and the periods were quantitatively analyzed. Since the ranges of the hematological parameters of the normal and infection groups overlap each other to a great extent, it would be difficult to use the absolute values to predict the infection. However, the lower limit of the 95% CI of the postoperative infection group was higher than the upper limit of the 95% CI of the normal group in some parameters. Accordingly, if any number exceeds the lower limit of the 95% CI of the postoperative infection group, infection can be strongly suspected. In the one-level and the two-level fusion groups, if the neutrophil count 8-11 days after the operation exceeds 5,898.5 n/µL, and if the neutrophil count is greater than 4,949 n/µL in the one-level fusion group 12-14 days after the operation, there should be strong suspicion of infection. Also, in the normal group, if the CRP exceeds 4.27 mg/dL at 8-11 days after the operation and 4.71 mg/dL at 12-14 days after the operation, infection can be strongly suspected. In this study, all the infection patients met more than one of the above standards. However, there were some among those who met the above standards yet had no infection. In conclusion, if the CRP and neutrophil counts are high, or if the CRP begins to rise again 8 days after the operation, the likelihood of infection increases. If the hematological parameters are higher than the lower limit of the 95% CI of the postoperative infection group, infection must be strongly suspected.
ACKNOWLEDGEMENTS
This work was supported by a clinical research grant-in-aid from the Seoul Metropolitan Government Seoul National University (SMG-SNU) Boramae Medical Center (03-2011-4). The authors thank Hye Soo Lee for her assistance in this study.
References
1. Abbey DM, Turner DM, Warson JS, Wirt TC, Scalley RD. Treatment of postoperative wound infections following spinal fusion with instrumentation. J Spinal Disord. 1995. 8(4):278–283.

2. Takahashi J, Ebara S, Kamimura M, et al. Early-phase enhanced inflammatory reaction after spinal instrumentation surgery. Spine (Phila Pa 1976). 2001. 26(15):1698–1704.

3. Zucherman J, Hsu K, White A, Wynne G. Early results of spinal fusion using variable spine plating system. Spine (Phila Pa 1976). 1988. 13(5):570–579.

4. Keller RB, Pappas AM. Infection after spinal fusion using internal fixation instrumentation. Orthop Clin North Am. 1972. 3(1):99–111.

5. Aono H, Ohwada T, Kaneko N, Fuji T, Iwasaki M. The post-operative changes in the level of inflammatory markers after posterior lumbar interbody fusion. J Bone Joint Surg Br. 2007. 89(11):1478–1481.

6. Black S, Kushner I, Samols D. C-reactive protein. J Biol Chem. 2004. 279(47):48487–48490.

7. Vigushin DM, Pepys MB, Hawkins PN. Metabolic and scintigraphic studies of radioiodinated human C-reactive protein in health and disease. J Clin Invest. 1993. 91(4):1351–1357.

8. Thelander U, Larsson S. Quantitation of C-reactive protein levels and erythrocyte sedimentation rate after spinal surgery. Spine (Phila Pa 1976). 1992. 17(4):400–404.

9. Larsson S, Thelander U, Friberg S. C-reactive protein (CRP) levels after elective orthopedic surgery. Clin Orthop Relat Res. 1992. (275):237–242.
10. Neumaier M, Metak G, Scherer MA. C-reactive protein as a parameter of surgical trauma: CRP response after different types of surgery in 349 hip fractures. Acta Orthop. 2006. 77(5):788–790.
11. Scherer MA, Neumaier M, von Gumppenberg S. C-reactive protein in patients who had operative fracture treatment. Clin Orthop Relat Res. 2001. (393):287–293.

12. White J, Kelly M, Dunsmuir R. C-reactive protein level after total hip and total knee replacement. J Bone Joint Surg Br. 1998. 80(5):909–911.

13. Mok JM, Pekmezci M, Piper SL, et al. Use of C-reactive protein after spinal surgery: comparison with erythrocyte sedimentation rate as predictor of early postoperative infectious complications. Spine (Phila Pa 1976). 2008. 33(4):415–421.

14. Jonsson B, Soderholm R, Stromqvist B. Erythrocyte sedimentation rate after lumbar spine surgery. Spine (Phila Pa 1976). 1991. 16(9):1049–1050.

15. Foglar C, Lindsey RW. C-reactive protein in orthopedics. Orthopedics. 1998. 21(6):687–691.

16. Piper KE, Fernandez-Sampedro M, Steckelberg KE, et al. C-reactive protein, erythrocyte sedimentation rate and orthopedic implant infection. PLoS One. 2010. 5(2):e9358.









 PDF
PDF ePub
ePub Citation
Citation Print
Print


 XML Download
XML Download